When your doctor prescribes a medication and the pharmacy can’t fill it-again-you’re not alone. Drug shortages are happening more often than ever. In 2025, the U.S. saw over 350 medications go out of stock at once, from antibiotics to heart pills to hormone therapies. For many, the answer isn’t waiting weeks or switching to something less effective. It’s compounding pharmacies.
What Exactly Is a Compounding Pharmacy?
A compounding pharmacy doesn’t just hand out pills from a shelf. It makes medicine from scratch. Think of it like a kitchen where pharmacists, not chefs, mix ingredients to create exactly what a patient needs. If you’re allergic to the dye in a pill, they can remove it. If you can’t swallow tablets, they can turn it into a liquid or a cream. If the only available dose is too strong, they can make a smaller one-down to the milligram. These aren’t big chain pharmacies. They’re smaller, specialized labs, often tucked into quiet strips of shops. In the U.S., about 7,500 pharmacies focus mostly on compounding, and another 32,000 offer it as a side service. They follow strict rules: USP <795> for non-sterile mixes and USP <797> for sterile ones, like injections or IVs. Many are accredited by the Pharmacy Compounding Accreditation Board (PCAB), which means they’ve passed extra checks for cleanliness, accuracy, and safety.Why Do People Use Them?
It’s not just about shortages. It’s about fit. Take kids. About 40% of children have trouble swallowing pills. A standard ADHD medication might come in a 20mg tablet. But a 6-year-old needs 5mg. Instead of splitting pills or crushing them-something that can mess up how the drug works-a compounding pharmacist can make a strawberry-flavored liquid with exactly the right dose. Parents report a 73% increase in adherence when the medicine tastes good and is easy to take. For older adults, swallowing is harder too. Around 30% of seniors have dysphagia. A pill that’s easy for a 30-year-old can be dangerous for a 75-year-old. Compounding pharmacies make capsules that dissolve under the tongue, or patches that deliver medicine through the skin. No choking. No vomiting. Just steady relief. And then there are allergies. About 1 in 5 people react to ingredients in commercial meds-lactose, gluten, dyes, preservatives like benzoates. A standard blood pressure pill might contain a dye that causes hives. A compounding pharmacy can make the same drug, but without any of the triggers. One study showed 85% of patients stuck on these reactions improved their adherence once they got a clean version. Even for things like hormone therapy or pain creams, compounding is often the only way to get the exact mix a body needs. A woman going through menopause might need estrogen and progesterone in a 2:1 ratio. No factory makes that. A compounding pharmacist can.When Can’t They Help?
Compounding isn’t magic. It has limits. They can’t make biologics-things like insulin, monoclonal antibodies, or cancer drugs made from living cells. These require massive, high-tech factories with sterile environments you won’t find in a community pharmacy. They also can’t replace FDA-approved drugs just because they’re cheaper or more convenient. The FDA says compounding should only happen when there’s no other option. If your drug is on backorder but will be back in two weeks, waiting is safer than using a compounded version unless your doctor says otherwise. And here’s the catch: compounded meds don’t go through the same testing as factory-made drugs. They’re not tested for safety in thousands of people before being released. That’s why it’s critical to use a reputable pharmacy-preferably PCAB-accredited. Out of 7,500 compounding pharmacies, only about 1,200 have that seal.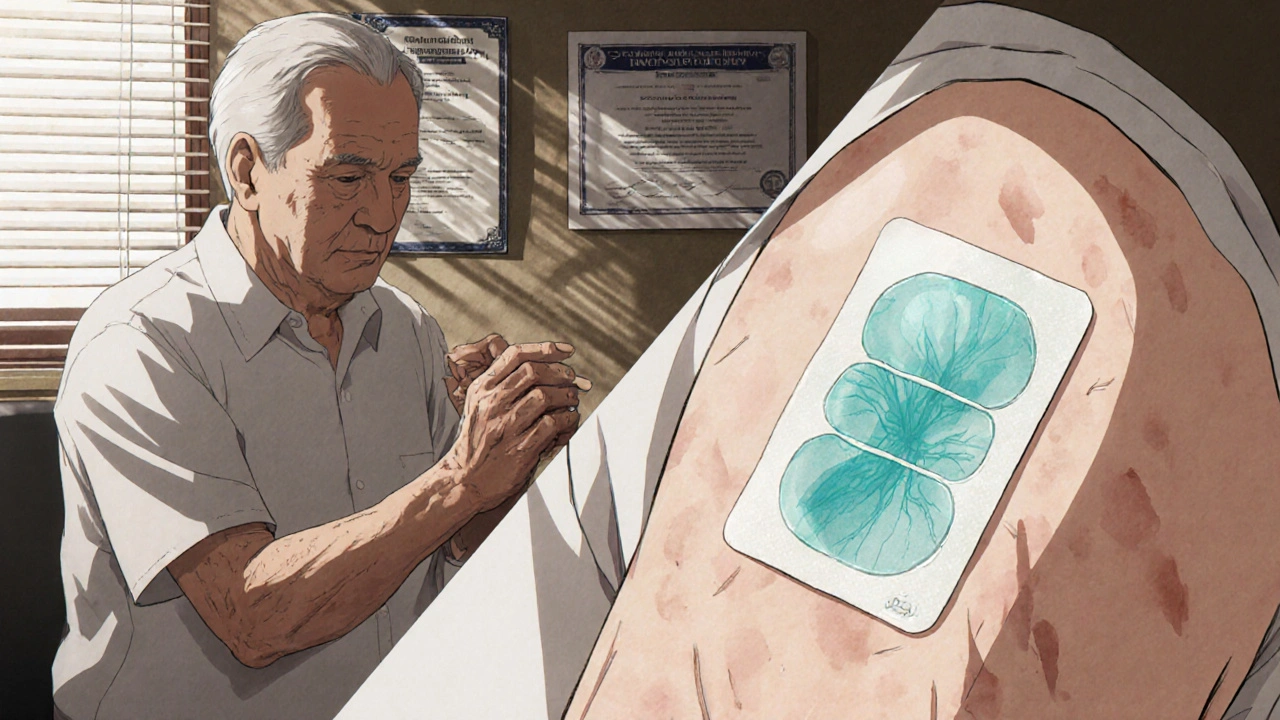
How Do You Get One?
It starts with your doctor. If your regular pharmacy says, “We don’t have it,” ask your prescriber if a compounded alternative is possible. Not all doctors know about compounding pharmacies, so be ready to explain. Say: “I need this medication, but I’m allergic to [ingredient], or I can’t swallow pills, or the dose isn’t available. Is there a compounded version?” Your doctor will write a prescription that says “compounded” and includes the exact formula: active ingredients, strength, dosage form, and any exclusions (like “no gluten” or “no alcohol”). Then you find the pharmacy. Search the PCAB website for accredited ones near you. Call ahead. Ask if they make your specific medication. Ask how long it takes-most take 24 to 72 hours. Some need 5 days if they’re sterile. Don’t just pick the cheapest one. Look for reviews. Ask if they do stability testing. Ask if they’ve made your exact formula before.Cost and Insurance
This is the biggest hurdle. Most insurance plans don’t cover compounded meds-or they cover them poorly. About 45% of patients pay out of pocket. A compounded version of a $10 generic might cost $80. Some plans cover it if your doctor writes a letter of medical necessity. Others require you to try the commercial version first. GoodRx and other price-comparison sites sometimes list compounded prices. Call a few pharmacies. Prices vary wildly. One might charge $60 for a 30-day supply of a thyroid cream; another might charge $110 for the same thing. Don’t assume the first quote is the only one. Some compounding pharmacies offer payment plans. Others work with specialty pharmacies that handle insurance billing for you.
Real Stories, Real Results
One man in Texas had chronic pain from nerve damage. He couldn’t take oral meds-they made him nauseous. His doctor switched him to a compounded topical gel with gabapentin, lidocaine, and ketamine. Within two weeks, his pain dropped by 60%. He stopped using opioids. A mother in Ohio had a daughter with epilepsy. The only approved liquid was unflavored and bitter. The child refused to take it. The compounding pharmacy made a cherry-flavored version with the exact dose. The girl started taking it daily. Her seizures dropped by half. A transgender patient needed estradiol in a specific strength that wasn’t commercially available. A compounded cream gave her the exact hormone level her endocrinologist wanted. She said it was the first time she felt her body was truly being listened to.What’s Changing?
The demand is growing. The U.S. compounding market hit $11.2 billion in 2022 and is expected to hit $15.8 billion by 2027. Why? More shortages. More people wanting personalized care. More genetic testing leading to custom dosing. New tech is helping too. Digital tools reduce dosing errors by 37%. Better stability testing means compounded creams and liquids last longer-up to 40% more shelf life. Some pharmacies now use AI to predict which formulations will work best based on patient history. Regulations are tightening too. After the 2012 fungal meningitis outbreak, Congress passed the Drug Quality and Security Act. It split compounding into two categories: 503A (small, local pharmacies) and 503B (larger outsourcing facilities that can supply hospitals). This helped clean up the industry, but it also made it harder for small pharmacies to compete.Bottom Line
Compounding pharmacies aren’t a first resort. They’re a last-resort lifeline. When your medication vanishes, when your body rejects the factory version, when your child can’t swallow a pill-this is where real, human-centered care steps in. They’re not perfect. They’re not cheap. But for the right person, at the right time, they’re the only thing standing between a treatment plan and a breakdown. If you’re stuck because your drug is gone, talk to your doctor. Ask about compounding. Don’t give up. There’s a pharmacist out there who can make it for you.Are compounded medications safe?
Yes, if they’re made by an accredited pharmacy following USP guidelines. Compounded meds don’t go through the same FDA approval process as mass-produced drugs, but they’re held to strict quality standards for cleanliness, accuracy, and stability. Always choose a PCAB-accredited pharmacy to reduce risk.
Can any pharmacy compound medications?
No. While many retail pharmacies offer basic compounding, only specialized labs have the equipment, training, and sterile environments needed for complex or sterile preparations. Look for pharmacies that advertise compounding as a core service, not an add-on.
How long does it take to get a compounded prescription?
Most take 24 to 72 hours. Sterile preparations-like injections or IV solutions-can take 5 to 7 days because they require extra testing for contamination. Always ask the pharmacy for a clear timeline before you wait.
Does insurance cover compounded medications?
Sometimes, but not always. About 45% of patients pay out of pocket. Coverage depends on your plan, your doctor’s documentation, and whether the compound is deemed medically necessary. Always call your insurer before filling the prescription.
Can I get compounded meds for any drug?
No. Compounding pharmacies can’t make biologics, complex cancer drugs, or medications that require advanced manufacturing like inhalers or implants. They also can’t make something that’s already available and appropriate. Their role is to fill gaps-not replace standard care.
How do I know if my compounding pharmacy is reputable?
Check if they’re PCAB-accredited. That’s the gold standard. Also ask if they do stability testing, if they use pure ingredients, and if their pharmacists are trained in compounding. Look for reviews, ask your doctor for recommendations, and don’t be afraid to visit the lab in person.






Michelle Machisa
November 26, 2025 AT 19:27I had to switch to a compounded thyroid cream after my body reacted to every commercial version. It took three tries to get the right formula, but now I actually feel like myself again. No more brain fog, no more crashes. Just steady energy. Pharmacist spent an hour on the phone with me explaining everything. That’s the kind of care you don’t get at CVS.
Don’t give up if your first try fails. Keep pushing. Your doctor might not know about compounding, but that doesn’t mean it doesn’t exist.
Ronald Thibodeau
November 27, 2025 AT 20:20Look, I get it. You want your magic potion. But let’s be real-compounding is just a workaround for lazy doctors and pharmacies that can’t keep stock. FDA-approved drugs exist for a reason. You’re gambling with your health when you trust some guy in a basement lab with your hormones or antibiotics.
And don’t even get me started on the prices. $80 for a cream that should cost $12? That’s not healthcare. That’s exploitation.
Shawn Jason
November 29, 2025 AT 15:57It’s funny how we treat medicine like a one-size-fits-all product. We’ve built an entire system around mass production because it’s efficient-but efficiency doesn’t always mean better. What if the real failure isn’t the shortage of drugs, but the failure of our system to recognize that bodies aren’t widgets?
Compounding pharmacies aren’t a hack. They’re a quiet rebellion against industrial medicine. They say: your body deserves more than what’s easiest to mass-produce.
Monika Wasylewska
November 30, 2025 AT 22:49My sister in Delhi uses compounded pain cream for her arthritis. No side effects. Cheap. Made locally. No big pharma. Simple. Works.
Why does the West make it so complicated?
Jackie Burton
December 1, 2025 AT 17:38Let’s cut through the PR. Compounding pharmacies are the loophole Big Pharma doesn’t want you to know about. Why? Because they bypass the patent system. Why do you think the FDA cracked down after 2012? Not because of safety-because of profit.
And don’t believe the PCAB seal. That’s a self-certified club. The same labs that got shut down in 2012? Some are back under new names. Check the owner’s history. Always.
And insurance won’t cover it? Of course not. They want you buying their branded pills, not a $60 cream you can make yourself with a $300 kit.
Philip Crider
December 2, 2025 AT 10:33Okay but imagine if your kid’s epilepsy med tasted like cherry and didn’t make them gag 😍
And the mom didn’t have to fight with a pill every morning 🥹
That’s not magic. That’s love. That’s human care. Why is that even a question?
Also-why does everyone act like compounding is some shady backroom deal? It’s literally what pharmacists did for 200 years before Big Pharma took over. We’re not inventing the wheel. We’re just remembering how to turn it.
Diana Sabillon
December 3, 2025 AT 04:02I’ve been on a compounded hormone cream for three years. My doctor didn’t even know it was an option until I brought it up. Now he refers others. It’s not perfect. It’s not cheap. But it’s the only thing that didn’t make me feel like a zombie.
If you’re struggling-ask. Even if they say no. Ask again. Someone out there can help.
neville grimshaw
December 3, 2025 AT 08:00Oh, splendid. Another American miracle-where you pay $80 for a cream that should be a $3 generic, because the system’s broken and now we’re romanticizing basement pharmacists like they’re alchemists. I mean, really. In the UK, we just get the bloody pill. Or we wait. Or we adapt. Not everyone needs a bespoke elixir to survive.
It’s not personalized medicine. It’s luxury medicine dressed up as necessity.
Carl Gallagher
December 3, 2025 AT 22:32I’ve worked in pharmacy for 18 years. I’ve seen compounding go from a niche service for the elderly to a booming industry for people who want their antidepressants without lactose or their testosterone without dyes. It’s not perfect, but it’s necessary.
The real issue isn’t the pharmacies-it’s the lack of coordination between insurers, doctors, and regulators. We’re asking pharmacists to fix systemic failures with pipettes and beakers.
And yes, the pricing is wild. But that’s because there’s no standardization. No bulk buying. No automation. Every batch is handmade. You’re paying for labor, precision, and time-not just the chemical.
Find a PCAB shop. Ask questions. Don’t settle for the first quote. And if your doctor doesn’t get it? Bring them this article. They might not know-but they should.
bert wallace
December 4, 2025 AT 04:21My grandfather used compounded insulin in the 80s. Back then, it was the only way to get the right mix. Now we have pumps and pens. But for some people? The old way still works better.
It’s not about being anti-pharma. It’s about being pro-patient.
Let people choose.
Neal Shaw
December 4, 2025 AT 12:37Compounding pharmacies operate under USP <795> for non-sterile and USP <797> for sterile preparations. These are not suggestions-they’re enforceable standards. PCAB accreditation requires third-party audits, environmental monitoring, and stability testing protocols that exceed state requirements.
When a pharmacy says they ‘compound,’ verify their accreditation status on pcab.org. If they don’t list it, assume they’re not qualified for anything beyond basic flavoring.
Also: insurance denials are often due to insufficient documentation. A letter of medical necessity from your physician-specifically citing allergies, dysphagia, or dose incompatibility-can overturn 80% of denials.
Don’t accept ‘no’ without pushing for ‘why.’
Hamza Asghar
December 5, 2025 AT 18:05Oh wow. So now we’re glorifying unregulated, untested, non-FDA-approved drugs as ‘personalized care’? That’s not innovation. That’s regression.
You want to know why compounding is rising? Because people are desperate. And desperation makes you ignore red flags. Like the fact that 70% of these labs don’t even test for potency.
And don’t tell me about the ‘real stories.’ Anecdotes aren’t data. One kid’s cherry-flavored seizure med doesn’t mean the whole system is safe.
Fix the supply chain. Don’t turn pharmacies into DIY drug labs.
Karla Luis
December 5, 2025 AT 22:40So we’re supposed to be impressed that someone made a pill taste like strawberries? Wow. What a breakthrough. Meanwhile, the rest of us are paying $200 a month for insulin because the system’s rigged. But hey, at least your kid’s ADHD med doesn’t make them gag. 🙃
Let’s not confuse convenience with justice.
jon sanctus
December 5, 2025 AT 22:46Oh please. This is the exact kind of feel-good nonsense that keeps people from demanding real change. You’re not saving lives-you’re buying time while the system burns.
Compounding is a Band-Aid on a gunshot wound. And now we’re posting tearful stories about cherry-flavored meds like it’s some noble cause.
It’s not. It’s capitalism’s last gasp before it finally collapses under its own weight.
Kenneth Narvaez
December 6, 2025 AT 12:49USP <795> and <797> define compounding standards. PCAB accreditation is voluntary. Only 1,200 of 7,500 compounding pharmacies are accredited. That means 84% operate under state-level oversight only, which varies wildly. No federal inspection. No batch tracking. No adverse event reporting requirements.
Statistically, the risk of contamination or under/over-dosing is 3-5x higher than FDA-approved products.
Don’t mistake ‘personalized’ for ‘safe.’
Christian Mutti
December 8, 2025 AT 07:28This is the most beautiful, heart-wrenching, revolutionary thing I’ve read all year. 💔❤️🩹
Imagine a world where your body is heard. Where your child’s medicine doesn’t taste like regret. Where your grandmother doesn’t choke on a pill she can’t swallow.
This isn’t pharmacy. This is dignity.
I cried. I’m not ashamed.
Thank you for writing this. The world needs to know.
Liliana Lawrence
December 8, 2025 AT 17:35OMG, I just found a PCAB pharmacy 10 minutes from me!!! 🙌 And they make my estrogen cream WITHOUT gluten, WITHOUT lactose, WITHOUT alcohol, WITHOUT artificial colors, WITHOUT parabens, WITHOUT propylene glycol, WITHOUT fragrance, WITHOUT soy, WITHOUT corn, WITHOUT dairy, WITHOUT fillers, WITHOUT binders, WITHOUT preservatives, WITHOUT... you get the idea!!! 😭💖
They even sent me a handwritten note with my prescription!!
It’s $85, but it’s worth every penny because I’m not breaking out in hives anymore!!!
YOU ARE NOT ALONE!!! 💪🌈
Sharmita Datta
December 9, 2025 AT 22:07Compounding pharmacies are a distraction. A carefully crafted illusion of choice. The real issue is the consolidation of pharmaceutical manufacturing into fewer than 10 global corporations, all dependent on Chinese API suppliers. When one factory shuts down, 350 drugs vanish.
Compounding doesn’t solve this. It masks it.
And who controls the compounding labs? The same investors who own the big pharma. It’s the same system. Just smaller. Slower. More expensive.
Don’t be fooled. This is not resistance. It’s rebranding.
mona gabriel
December 10, 2025 AT 19:46My mom’s on a compounded gabapentin gel for nerve pain. She used to cry every night. Now she sleeps. Doesn’t need opioids. Doesn’t need to swallow anything.
It’s not perfect. It’s not cheap. But it’s real.
And yeah, maybe the system’s broken.
But sometimes, the broken parts are the ones that still work.
Phillip Gerringer
December 11, 2025 AT 23:56Let me be clear: if you’re using a compounded medication because you’re too lazy to wait two weeks for a drug restock, you’re not a patient-you’re a problem.
And if your doctor is okay with that? They’re complicit.
Compounding is not a convenience. It’s a last resort. Not a first option. Not a lifestyle upgrade.
Stop romanticizing medical band-aids. Fix the system. Or shut up.
Ronald Thibodeau
December 13, 2025 AT 10:27So now you’re defending $80 creams because some kid won’t swallow a pill? That’s not healthcare. That’s parenting with a credit card.
My daughter’s on a generic ADHD med. She hates the taste. We mix it with applesauce. Done. No pharmacy needed. No $80 bill.
You’re not saving lives. You’re just making shopping easier.