When you’re pregnant and diagnosed with gestational diabetes, the first thing you might feel is overwhelm. It’s not just about cutting out sugar-it’s about relearning how to eat for two, while keeping your blood sugar steady. The good news? You don’t need to follow a complicated diet. With the right structure, you can eat real food, feel satisfied, and keep both you and your baby healthy.
What Are the Blood Sugar Targets for Gestational Diabetes?
Knowing your numbers isn’t about fear-it’s about control. The International Association of Diabetes and Pregnancy Study Groups (IADPSG) sets clear targets that most doctors follow:
- Fasting: Below 95 mg/dL
- 1 hour after eating: Below 140 mg/dL
- 2 hours after eating: Below 120 mg/dL
These aren’t arbitrary numbers. Studies show that staying within this range cuts the risk of having a baby over 9 pounds by nearly half. It also lowers your chance of needing a C-section and reduces the odds of your newborn having low blood sugar right after birth.
Some women use a continuous glucose monitor (CGM), which gives real-time readings. Others check with a finger prick four times a day. Either way, the goal is the same: avoid spikes and dips. The biggest mistake? Waiting until after meals to adjust. The fix? Plan your meals so your blood sugar never gets too high in the first place.
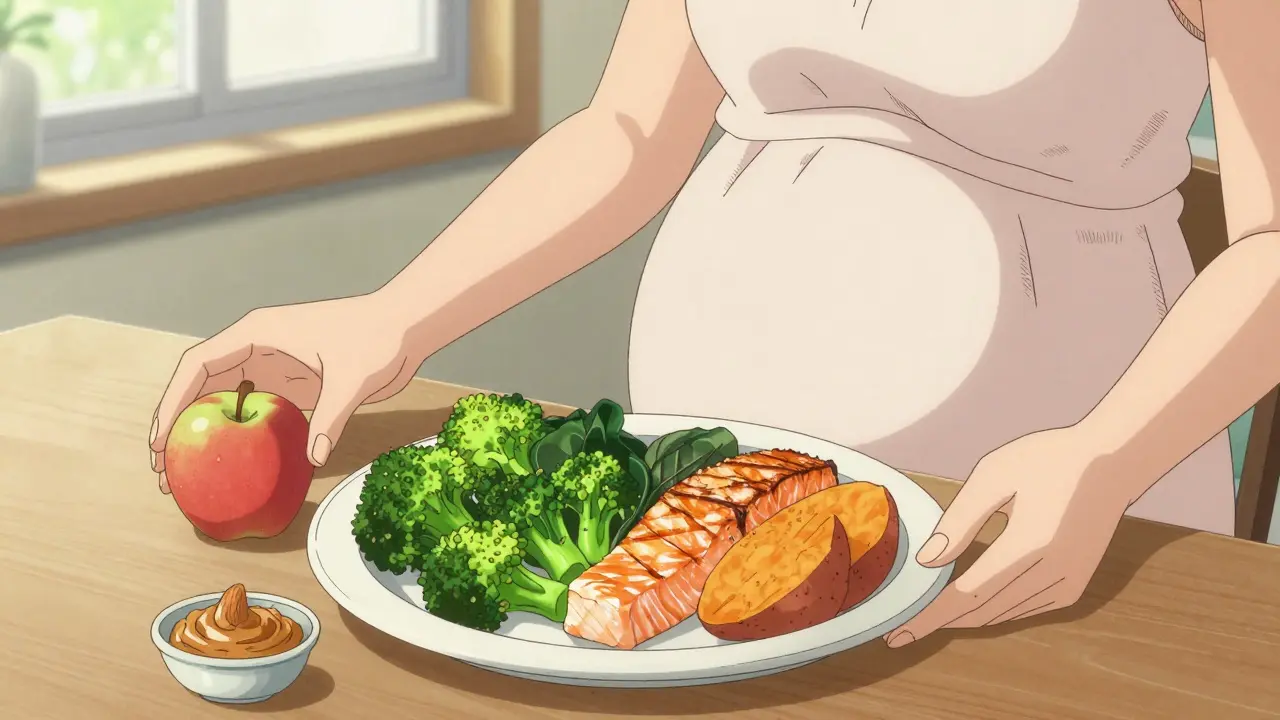
The Plate Method: Simple, Visual, and Effective
Counting grams of carbs can feel like doing math homework-especially when you’re tired, nauseous, or just done with spreadsheets. That’s why the plate method works so well for most women.
Here’s how it works:
- Take a nine-inch plate.
- Fill half with non-starchy vegetables: broccoli, spinach, peppers, zucchini, cauliflower, salad greens.
- Fill one-quarter with lean protein: chicken, fish, tofu, eggs, lean beef, lentils.
- Fill one-quarter with carbohydrate sources: brown rice, quinoa, whole grain bread, sweet potato, oats, fruit.
This method isn’t just easy-it’s proven. A 2020 study in the Journal of the Academy of Nutrition and Dietetics found women using the plate method had the same blood sugar control as those counting carbs-but they stuck with it 37% longer. Why? Because you don’t need a scale or a phone app. You just look at your plate.
For example: dinner could be grilled salmon (protein), roasted Brussels sprouts and asparagus (vegetables), and ½ cup of cooked brown rice (carbs). That’s it. No counting. No guesswork.
How Many Carbs Should You Eat Per Meal?
If you prefer numbers, the American Diabetes Association recommends 45 to 60 grams of net carbohydrates per meal. Net carbs = total carbs minus fiber. So if a serving of oats has 25g total carbs and 5g fiber, that’s 20g net carbs.
Snacks? Aim for 15 grams of net carbs. That’s about:
- One small apple
- One cup of berries
- One slice of whole grain toast
- Half a cup of plain Greek yogurt with a handful of almonds
But here’s the key: don’t eat carbs alone. Always pair them with protein or fat. Eating a banana by itself? Blood sugar spikes. Eating a banana with a tablespoon of peanut butter? Slow, steady rise. That’s the difference between control and chaos.
Protein and Fat Are Your Allies
Many women with gestational diabetes think they need to eat less fat and more carbs. That’s the opposite of what works.
Protein slows down how fast carbs turn into sugar. Fat does the same. That’s why a snack of cheese and an apple is better than just the apple. A meal with chicken, broccoli, and olive oil is better than pasta with tomato sauce.
In the third trimester, your body needs more protein-about 2.5 ounces per meal. That’s the size of a deck of cards. Good sources include eggs, Greek yogurt, cottage cheese, chicken breast, tofu, and beans. If you’re vegetarian, combine beans with rice or quinoa to get complete protein.
Fats like avocado, nuts, seeds, and olive oil don’t raise blood sugar at all. They help you feel full longer and support your baby’s brain development. Don’t fear them-use them.

Meal Timing Matters More Than You Think
It’s not just what you eat-it’s when.
Many women skip breakfast because of morning sickness. Bad idea. Skipping meals causes your liver to dump glucose into your blood, raising fasting levels. That’s why even if you’re not hungry, eat something light within an hour of waking up.
Try this pattern:
- Breakfast: 15-30g net carbs + protein
- Mid-morning snack: 15g net carbs
- Lunch: 45-60g net carbs + protein + veggies
- Afternoon snack: 15g net carbs
- Dinner: 45-60g net carbs + protein + veggies
- Bedtime snack (if needed): 15g net carbs + protein
Spreading carbs across six eating occasions prevents your body from overproducing glucose overnight. That’s why some women have high fasting numbers-not because they ate too much the night before, but because they didn’t eat enough before bed.
Real Food Over Processed ‘Diabetic-Friendly’ Products
Walk down the ‘diabetic’ aisle at the grocery store and you’ll see cookies, breads, and bars labeled ‘low sugar’ or ‘no added sugar.’ Don’t be fooled.
A 2023 Lancet study found these products contain 27% more sodium than regular whole foods. They’re often low in fiber, high in refined starches, and full of artificial sweeteners that can still trigger insulin spikes.
Stick to whole foods:
- Instead of sugar-free cereal → oatmeal with chia seeds and berries
- Instead of diabetic crackers → whole grain toast with avocado
- Instead of sugar-free yogurt → plain Greek yogurt with cinnamon and a few blueberries
Real food doesn’t come with a label you need to decode. It comes from the ground, the farm, or the sea.
What Works for One Woman Might Not Work for Another
Not every plan fits every body. Some women need to eat fewer carbs. Others do fine with more. Cultural food preferences matter too.
A 2021 Diabetes Care study found 22% of women needed personalized adjustments because standard plans didn’t match their diet. For example:
- A Filipino woman might prefer adobo chicken with half a cup of brown rice instead of quinoa.
- A Mexican woman might swap rice for black beans and corn tortillas.
- A vegetarian might rely on lentils, chickpeas, and paneer.
There’s no one-size-fits-all. The goal is to find what works for you-not what looks right on a brochure.
Common Mistakes and How to Avoid Them
Here’s what trips up most women:
- Underestimating portion sizes: A half-cup of cooked rice is about the size of a tennis ball. Most people pour way more. Use measuring cups for the first week until you get the hang of it.
- Drinking fruit juice: Even 100% juice spikes blood sugar fast. Eat the whole fruit instead.
- Skipping snacks: That leads to overeating at meals and bigger spikes.
- Not checking blood sugar after meals: You won’t know what works unless you test. Even twice a week helps.
- Using artificial sweeteners daily: Some studies link them to altered gut bacteria and insulin resistance. Use sparingly.
And if you’re struggling with anxiety around food? You’re not alone. A 2021 study in the Journal of Eating Disorders found 15% of women with GDM developed disordered eating patterns from strict carb counting. If you feel obsessed, guilty, or fearful around meals, talk to your doctor or a dietitian. Mental health is part of your treatment.
Support Is Available-Use It
You don’t have to do this alone. Over 147,000 women are in the ‘Gestational Diabetes Support’ Facebook group. They share meals, troubleshoot spikes, and celebrate wins.
Many hospitals offer free classes on GDM nutrition. The ADA-certified Gestational Diabetes Self-Management Program teaches you how to identify carbs, measure portions, and time meals in just three 60-minute sessions.
And if your insurance covers it (and most do now), a virtual dietitian visit can be life-changing. One woman in Melbourne told me she saved $400 by doing her sessions online instead of driving to a clinic every week.
What to Eat: A Sample Day
Here’s a realistic, doable day of eating:
- Breakfast: 2 scrambled eggs + ½ cup cooked oats + 1 tbsp chia seeds + ½ cup blueberries
- Mid-Morning Snack: 1 small apple + 1 tbsp almond butter
- Lunch: Grilled chicken salad with spinach, tomatoes, cucumbers, ½ cup quinoa, 1 tbsp olive oil & lemon dressing
- Afternoon Snack: ½ cup plain Greek yogurt + 10 almonds
- Dinner: Baked salmon + 1 cup roasted broccoli + ½ cup sweet potato
- Bedtime Snack (if needed): 1 oz cottage cheese + 1 small pear
This plan gives you about 50g net carbs per meal and 15g per snack. It’s high in fiber, protein, and healthy fats. And it doesn’t feel like a diet-it feels like normal, good food.
Long-Term Outlook: It’s Not Just About Pregnancy
Gestational diabetes doesn’t disappear after birth. Women who have it are 7 times more likely to develop type 2 diabetes later in life. But here’s the hopeful part: eating well during pregnancy cuts that risk in half.
What you learn now-how to balance carbs, choose fiber, eat protein first, avoid processed foods-becomes your lifelong health toolkit. This isn’t a temporary fix. It’s the foundation for decades of better health-for you and your child.
Can I eat fruit with gestational diabetes?
Yes, but choose wisely. Berries, apples, pears, and oranges are great because they’re high in fiber and have a low glycemic index. Stick to one small serving at a time, and always pair it with protein or fat-like a handful of nuts or a spoon of yogurt. Avoid fruit juice and dried fruit, which spike blood sugar quickly.
Do I need to avoid all sugar?
You don’t need to eliminate all sugar, but you should avoid added sugars in processed foods-soda, candy, pastries, sweetened yogurts. Natural sugars in fruit and dairy are fine in controlled amounts. The issue isn’t sugar itself-it’s how fast it hits your bloodstream. Pairing carbs with protein or fat slows absorption and keeps levels steady.
What if my blood sugar is still high even after following the plan?
You’re not failing-your body might just need more support. Talk to your doctor. You might need to adjust your carb intake, increase physical activity (like walking 20 minutes after meals), or start insulin. Many women do. It’s not a personal shortcoming-it’s a medical adjustment. About 15-20% of women with gestational diabetes eventually need insulin, and that’s completely normal.
Is it safe to lose weight during pregnancy with gestational diabetes?
No. Weight loss during pregnancy is not recommended, even if you’re overweight. Your baby needs energy and nutrients to grow. Instead of losing weight, focus on gaining the right amount-usually 15-25 pounds total, depending on your pre-pregnancy weight. Eat nutrient-dense foods and avoid empty calories. Healthy weight gain is part of managing GDM.
Can I drink alcohol occasionally?
No. Alcohol is not safe during pregnancy, regardless of gestational diabetes. It crosses the placenta and can affect your baby’s development. Even small amounts carry risks. If you’re struggling with cravings or stress, talk to your care team. There are safer ways to cope.
Will my baby have diabetes because I had gestational diabetes?
Your baby won’t be born with diabetes, but they do have a higher risk of developing type 2 diabetes or obesity later in life. The good news? Breastfeeding and healthy eating habits from the start can reduce that risk significantly. Your actions during pregnancy set the stage for your child’s long-term health.
Next Steps: What to Do Today
Don’t wait for your next appointment. Start now:
- Grab a nine-inch plate and mark the sections with a marker-half for veggies, quarter for protein, quarter for carbs.
- Write down your blood sugar targets and keep them on your fridge.
- Replace one processed snack with a real-food option: swap crackers for apple and cheese.
- Take a 10-minute walk after dinner. It lowers your post-meal sugar by up to 20%.
- Join a support group-even if you just read posts for a week.
You’re not just managing a condition. You’re building habits that will last a lifetime-for you and your child.



Kayleigh Campbell
December 15, 2025 AT 15:50So basically, you’re telling me I can eat avocado like it’s my job and no one will judge? Because I’m all in. This post felt like someone handed me a life raft made of broccoli and almond butter.
Souhardya Paul
December 16, 2025 AT 21:51I love how this breaks it down without making you feel like you’re back in high school chemistry. The plate method is genius - no apps, no spreadsheets, just look at your dinner. I showed my wife this last night and she actually smiled while eating salmon. That’s a miracle in our house.
Ron Williams
December 18, 2025 AT 13:45As someone who grew up eating rice with every meal, I appreciate the nod to cultural flexibility. My mom used to say, 'If it grows in the ground, it’s probably good for you.' Turns out she was right - even if she didn’t know the word 'glycemic index.' Swapping white rice for brown rice and adding lentils? That’s my grandma’s wisdom meets modern science.
Elizabeth Bauman
December 19, 2025 AT 23:53Why do they let big pharma sell you 'diabetic-friendly' junk that’s basically sugar with a side of sodium? It’s not a coincidence these products are marketed to pregnant women - they know we’re desperate. Stick to real food. Real food doesn’t need a label that says 'FOR DIABETICS.' That’s just a red flag.
Dan Padgett
December 20, 2025 AT 03:34There’s something beautiful about how food becomes medicine without needing a prescription. You don’t need to be perfect - just present. I remember eating a banana with peanut butter during my second trimester and feeling like I’d unlocked some ancient secret. The body knows what it needs if we just stop overcomplicating it.
Aditya Kumar
December 21, 2025 AT 12:28Too much info. Just tell me what to eat. I’m tired.
Joanna Ebizie
December 23, 2025 AT 08:22If you’re still eating sweet potatoes after reading this, you’re doing it wrong. You think you’re being healthy? You’re just sugar-bombing yourself with a side of pretentious veggies. Cut the carbs. All of them. That’s the real fix.
Andrew Sychev
December 24, 2025 AT 07:10They’re lying to you. They say 'eat real food' but the FDA is secretly pushing insulin because Big Pharma owns the hospitals. I know a woman who went keto and her sugar dropped to 70 overnight - then they told her she was 'at risk' for hypoglycemia. That’s not medicine. That’s control.
Dave Alponvyr
December 25, 2025 AT 02:38Walk after dinner. 10 minutes. Do it. Your blood sugar will thank you. And yes, it’s that simple.
Billy Poling
December 26, 2025 AT 20:12It is imperative to underscore that the physiological mechanisms governing postprandial glycemic response in gestational diabetes are fundamentally distinct from those observed in type 2 diabetes, particularly with regard to placental hormone-mediated insulin resistance. The plate method, while visually intuitive, lacks the precision required for optimal metabolic regulation, especially in the third trimester when human placental lactogen levels peak. Empirical data from the 2022 JAMA Obstetrics study indicate that carbohydrate distribution across six meals yields a 23% greater reduction in HbA1c variability compared to three-meal protocols. Furthermore, the recommendation to consume 15g of net carbs per snack may be insufficient for women with BMI >30, where hepatic gluconeogenesis is amplified. Therefore, I strongly advise individualized glycemic targets calibrated via continuous glucose monitoring, with nutritional counseling conducted by a certified diabetes care and education specialist - not random Reddit posts.
Josias Ariel Mahlangu
December 26, 2025 AT 22:51People think they’re being smart by eating fruit with peanut butter. But the truth? You’re just delaying the inevitable spike. If you can’t control yourself, then maybe you shouldn’t be eating carbs at all. This isn’t a diet. It’s a moral test.
Hadi Santoso
December 27, 2025 AT 12:01my mom’s from mexico and she always said ‘comida real, no mas cosas de la tienda’ - and she was right. i swapped those ‘diabetic’ tortillas for corn ones and my sugar’s been steady since. no fancy apps, just abuela’s kitchen. 🙏
anthony epps
December 29, 2025 AT 08:14Wait, so I can eat cheese and an apple? Like… for real? I thought I had to give up everything I liked.
Arun ana
December 31, 2025 AT 07:09Thank you for this. As a dad, I didn’t know how to help my wife until I read this. We started doing the plate method together - now we both eat better. And yes, I’ve started walking after dinner too. 😊