Opioid Dosing Calculator for Liver Disease
When a clinician reaches for an opioid to manage pain in a patient with cirrhosis, the biggest question isn’t "how much?" but "what will the liver do to it?" In liver disease the organ that normally breaks down these drugs is compromised, so standard doses can linger, stack up, and turn a helpful medication into a dangerous toxin.
Key Takeaways
- Opioids are primarily cleared by the liver via Cytochrome P450 enzymes and glucuronidation.
- Impaired hepatic function prolongs half‑life, increases peak concentrations, and raises the risk of neuro‑toxic metabolites.
- Morphine’s active metabolite M6G and neuro‑toxic M3G accumulate sharply in advanced cirrhosis.
- Oxycodone exposure can rise 40% and its half‑life stretch from 3.5 h to over 14 h in severe hepatic failure.
- Start with 30‑50 % of the usual dose and extend dosing intervals for most opioids; choose agents with minimal first‑pass metabolism when possible.
Opioids are a class of analgesics that bind to mu, kappa and delta receptors in the central nervous system, producing pain relief, sedation, and euphoria. They are widely prescribed for acute, chronic, and cancer‑related pain, but many carry a high risk of respiratory depression and dependence.
Liver disease refers to any condition that impairs hepatic function, ranging from non‑alcoholic fatty liver disease (NAFLD) and viral hepatitis to alcohol‑associated cirrhosis and acute liver failure. The degree of impairment is usually staged by Child‑Pugh or MELD scores, which guide drug‑dosing adjustments.
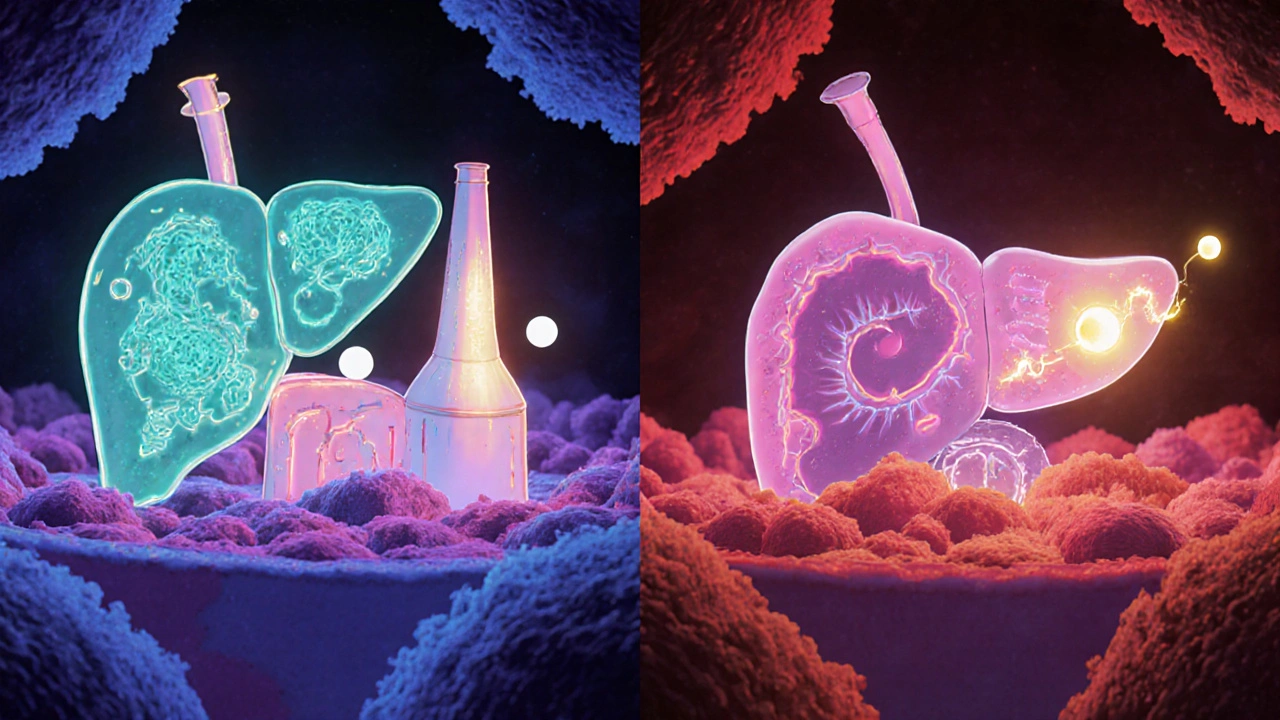
How Opioids Are Normally Processed
In a healthy adult, most opioids undergo Phase I oxidation (mainly by CYP3A4, CYP2D6, CYP2B6) and Phase II conjugation (glucuronidation via UDP‑glucuronosyltransferases). For example, morphine is transformed into morphine‑6‑glucuronide (M6G), a potent analgesic, and morphine‑3‑glucuronide (M3G), which can cause neuro‑excitatory effects. Oxycodone is metabolized by CYP3A4 (oxidation to noroxycodone) and CYP2D6 (hydroxylation to oxymorphone). The resulting metabolites are excreted primarily in urine, but the liver’s role in creating them is critical.
What Changes When the Liver Is Sick?
Hepatic disease reshapes enzyme activity in three major ways:
- Reduced Phase I oxidation: CYP3A4 activity drops in NAFLD and diabetes, slowing the breakdown of opioids like oxycodone.
- Shifted Phase II pathways: Glucuronidation may stay intact longer than oxidation, meaning metabolites such as M6G linger even when parent drug clearance falls.
- Altered CYP2E1 expression: Alcohol‑associated liver disease (ALD) ramps up CYP2E1, which can generate reactive oxygen species and heighten toxicity for drugs processed by this isoenzyme.
These shifts mean that the same oral dose can produce up to a 2‑fold increase in plasma concentration, and the elimination half‑life can stretch from hours to days.
Spotlight on Common Opioids
Below is a quick snapshot of how five frequently used opioids behave when the liver is compromised.
| Opioid | Primary Metabolic Pathway | Typical Dose Reduction | Recommended Dosing Interval Change |
|---|---|---|---|
| Morphine | Glucuronidation (M6G, M3G) | Start at 25‑50 % of usual dose | Extend interval 2‑3 × for Child‑Pugh C |
| Oxycodone | CYP3A4, CYP2D6 | 30‑50 % reduction in severe disease | Every 8‑12 h (vs every 6 h) |
| Methadone | Multiple CYPs (3A4, 2B6, 2C19) | Limited data - consider 25 % cut | Monitor QTc; keep 24‑h interval |
| Fentanyl (transdermal) | Direct bypass of first‑pass metabolism | May use standard dose, but start low | Standard 72‑h patch change |
| Buprenorphine (sublingual) | CYP3A4 | 30 % reduction if severe impairment | Maintain 12‑h dosing, watch for accumulation |
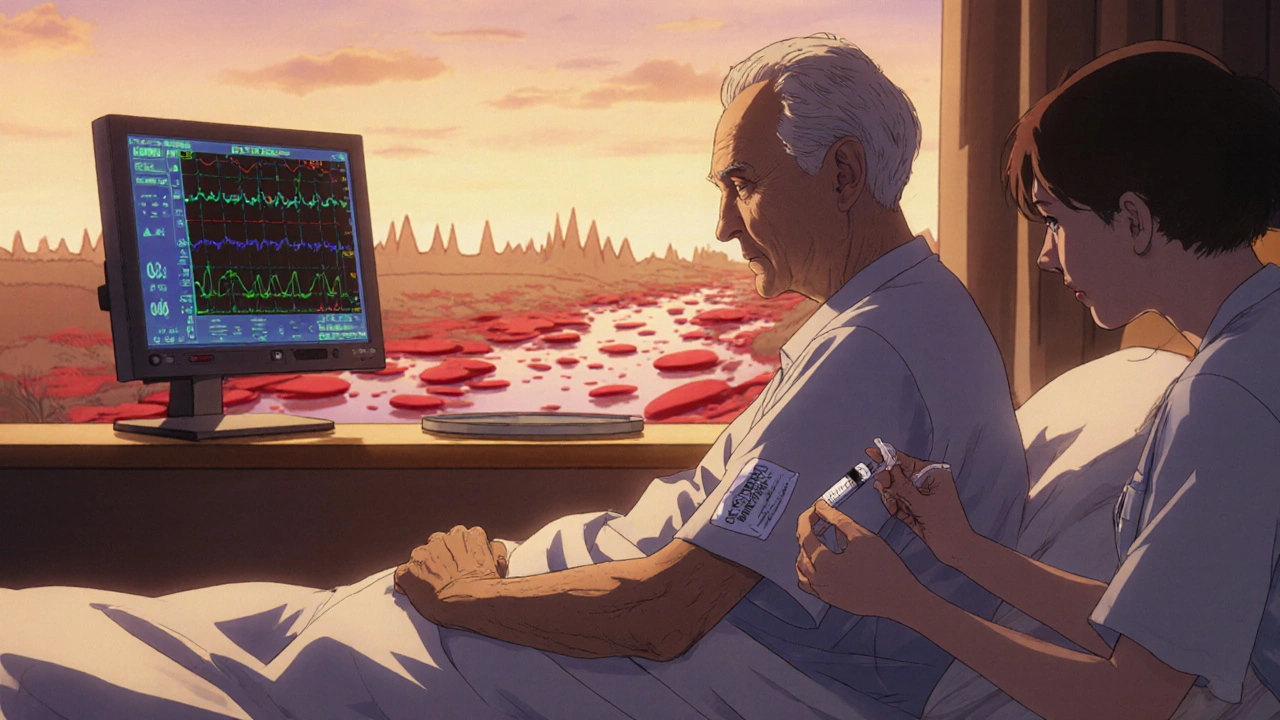
Why Accumulation Matters
When the liver can’t clear an opioid efficiently, both the parent drug and its active metabolites pile up. For morphine, M6G contributes analgesia but also respiratory depression; M3G, on the other hand, can cause hyperalgesia and agitation. Oxycodone’s parent molecule becomes more potent as its conversion to inactive metabolites slows, leading to prolonged sedation and a higher chance of falls in elderly cirrhotics.
Side‑Effect Profile in Hepatic Impairment
Common opioid adverse events-nausea, constipation, itching-are amplified because the body’s ability to metabolize and excrete the offending compounds is reduced. More severe risks include:
- Respiratory depression: Even modest plasma levels can suppress the drive to breathe, especially when combined with alcohol or sedatives.
- Encephalopathy: Accumulated M3G or oxycodone can cross the blood‑brain barrier, worsening hepatic encephalopathy.
- Pruritus and cholestasis: Opioid‑induced bile flow reduction may aggravate jaundice.
- Renal impairment: Metabolites like M6G are renally cleared; if kidney function is also compromised, a vicious cycle ensues.
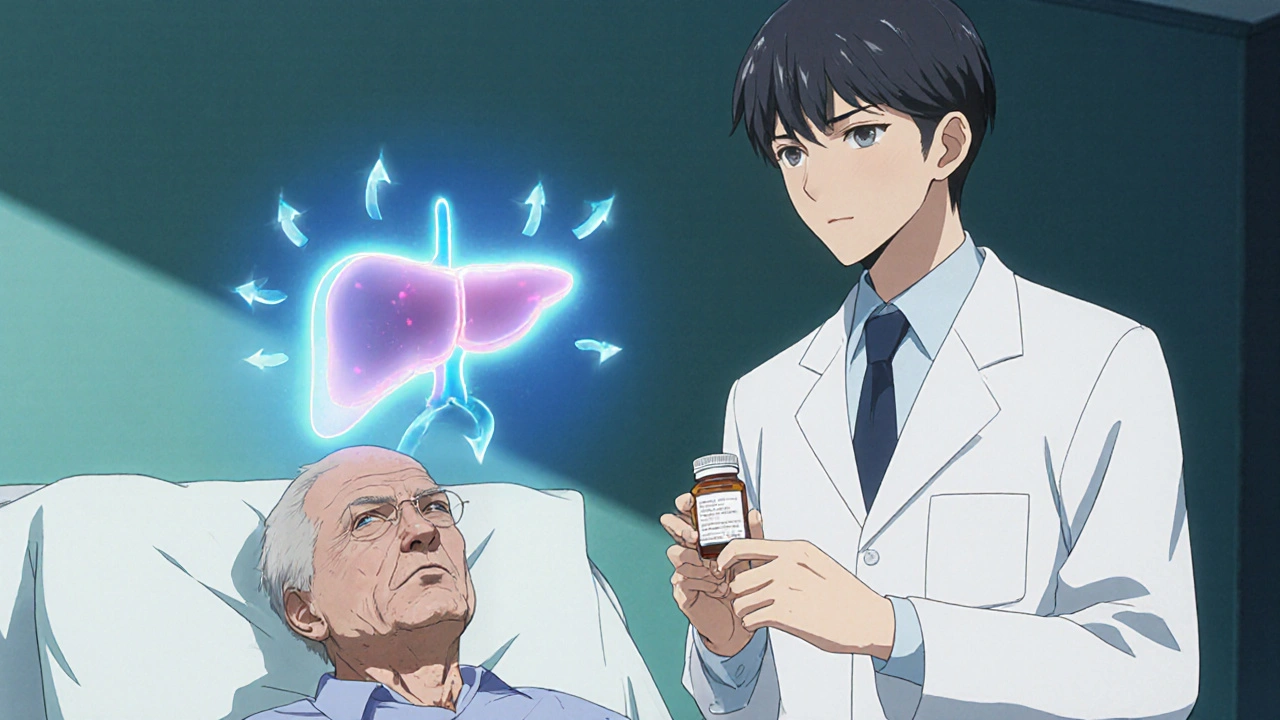
Practical Dosing Checklist for Clinicians
- Assess liver function: use Child‑Pugh or MELD score.
- Choose an opioid with the most predictable metabolism for the patient’s disease (e.g., transdermal fentanyl for ALD).
- Start at 30‑50 % of the standard dose; avoid rapid titration.
- Extend dosing intervals by at least 1.5‑2 × for severe impairment.
- Monitor trough plasma levels when available (especially for methadone).
- Check for signs of encephalopathy after each dose increase.
- Offer adjunctive non‑opioid analgesics (acetaminophen < 2 g/day, NSAIDs avoided if ascites present).
- Re‑evaluate pain control and side‑effects every 48‑72 h.
Managing Risk Beyond the Prescription
Non‑pharmacologic strategies-heat therapy, physiotherapy, cognitive‑behavioral techniques-can reduce the required opioid dose. When opioids are unavoidable, consider:
- Transdermal delivery: Fentanyl patches deliver a steady dose while sidestepping first‑pass metabolism, which is useful in alcohol‑related cirrhosis.
- Buprenorphine: Its partial agonist nature provides a ceiling effect for respiratory depression, making it safer in moderate hepatic dysfunction.
- Co‑prescription of laxatives and anti‑nausea meds: Prevents constipation‑induced worsening of ascites.
Emerging Research & Knowledge Gaps
Recent systematic reviews confirm a sharp rise in opioid‑related adverse events as hepatic function declines, yet data on fentanyl and buprenorphine pharmacokinetics remain sparse. Ongoing trials are exploring:
- Quantitative links between gut‑liver axis disruption and opioid‑induced encephalopathy.
- Pharmacogenomic profiling of CYP3A4 and CYP2D6 to personalize dosing.
- Validated dosing algorithms that integrate Child‑Pugh, MELD, and renal function.
Until these tools are widely available, clinicians must rely on careful assessment, conservative dosing, and vigilant monitoring.
Bottom Line
In patients with liver disease, the mantra is "start low, go slow, and watch closely." Understanding which enzymes handle each opioid, knowing how disease shifts those pathways, and adjusting the dose accordingly can keep pain under control without tipping the balance toward toxicity.
How does liver disease affect morphine metabolism?
Morphine is glucuronidated to morphine‑6‑glucuronide (M6G) and morphine‑3‑glucuronide (M3G). In hepatic impairment, glucuronidation slows, causing higher plasma levels of both metabolites. M6G adds analgesia but also respiratory depression, while M3G can trigger neuro‑excitatory symptoms, so dosing must be cut to 25‑50 % and intervals lengthened.
Is fentanyl safer than other opioids for cirrhotic patients?
Fentanyl’s transdermal route avoids first‑pass metabolism, reducing the burden on a diseased liver. However, its high potency means even small overdoses can cause respiratory depression, so start with the lowest patch strength and monitor closely.
What dosing change is recommended for oxycodone in severe hepatic impairment?
Reduce the initial dose to 30‑50 % of the standard amount and extend the dosing interval to every 8‑12 hours instead of every 6 hours. Therapeutic drug monitoring, when available, helps fine‑tune the regimen.
Can opioid‑induced constipation worsen liver disease?
Yes. Constipation can increase intra‑abdominal pressure, aggravating portal hypertension and ascites. Prophylactic laxatives and stool softeners are essential when prescribing opioids to cirrhotic patients.
How often should clinicians reassess opioid therapy in liver disease?
Re‑evaluate pain control, side‑effects, and hepatic status every 48‑72 hours during the titration phase, then at least monthly once a stable dose is achieved.




Erik Redli
October 26, 2025 AT 12:48Sure, everyone loves the hype that low‑dose opioids are safe in cirrhosis, but reality says otherwise – the liver’s a busted filter and those meds pile up faster than you think. Cutting the dose to 30‑50 % isn’t just a suggestion, it’s a necessity if you don’t want to watch a patient spiral into respiratory failure. And don’t even get me started on the myth that transdermal fentanyl magically sidesteps all problems; it still hits the brain hard. If you’re still giving standard doses, you’re basically gambling with someone’s life. The data on M6G and M3G accumulation is crystal clear, so stop pretending you can wing it. In short, start low, go slow, and keep your eyes glued to the vitals.
Monika Pardon
November 5, 2025 AT 15:12Ah, the ever‑so‑trustworthy “clinical guidelines” – obviously crafted by an elite cabal of pharma‑backed scholars who want us to believe that a simple 30‑percent reduction will magically fix everything. One might question, with a hint of sarcasm, whether the same entities who push opioids also control the research that says they’re safe in liver disease. Nonetheless, one cannot deny that the metabolic pathways mentioned (CYP3A4, CYP2D6) are indeed altered in cirrhosis, leading to increased half‑lives. It would be prudent, albeit mildly conspiratorial, to double‑check dosing calculators and perhaps consult an independent source free from corporate influence. In any case, a cautious, evidence‑based approach remains the best safeguard against unintended toxicity.
Dave Sykes
November 15, 2025 AT 17:36Team, remember that every patient is a unique case and the “start low, go slow” mantra is your best playbook. Assess the Child‑Pugh score, then cut the opioid dose in half and stretch the interval – that’s the assertive move that keeps you ahead of adverse events. Keep a close eye on sedation levels and be ready to adjust quickly; proactive monitoring beats reactive scrambling every time. Use adjuncts like acetaminophen (under 2 g) and non‑pharmacologic methods to lighten the opioid load. Your vigilance will pay off in safer pain control and fewer complications.
Erin Leach
November 25, 2025 AT 20:00I totally get how overwhelming it can feel when you’re juggling pain control and liver issues. It helps to take a breath and focus on the basics: start with a reduced dose, check vitals often, and involve the patient in the plan. Notice any early signs of encephalopathy or excessive drowsiness and act fast. Small steps and consistent monitoring make a huge difference, and you’ll see the patient stay stable while getting the relief they need.
Carla Smalls
December 5, 2025 AT 22:24Let’s keep the optimism flowing – even with cirrhosis, we have tools to manage pain safely. Begin with a modest opioid dose and pair it with physical therapy or heat therapy; those non‑drug options can cut the required opioid amount significantly. Encourage the patient to report any weird sensations right away, and adjust the regimen before problems snowball. Together, we can strike that balance between comfort and safety.
Jennyfer Collin
December 16, 2025 AT 00:48It is worth considering that the pharmaceutical industry may have vested interests in downplaying the risks of opioid accumulation in hepatic impairment. While the data presented is compelling, one cannot ignore the potential for selective reporting to protect market share. Therefore, clinicians should remain vigilant, cross‑reference multiple sources, and perhaps employ independent pharmacokinetic modeling when available. In a world where data can be subtly steered, a healthy dose of skepticism ensures patient safety.
Jay Campbell
December 26, 2025 AT 03:12Never underestimate the power of a simple dose check.
Paul Luxford
January 5, 2026 AT 05:36I appreciate the concise reminder; a quick verification of dosing can catch oversights before they become critical. Maintaining a calm, methodical approach ensures that each adjustment aligns with the patient’s evolving liver function. Let’s keep the dialogue open and share any insights we gain from real‑world application.
Nic Floyd
January 15, 2026 AT 08:00Alright let’s dive deep into the pharmacokinetic labyrinth 🌐 the liver’s enzymatic orchestra is basically a high‑throughput biocatalytic factory and when cirrhosis sets in the tempo slows dramatically 🚀 first‑pass metabolism via CYP3A4 and CYP2D6 gets throttled 🚧 the result is a prolonged half‑life and a higher Cmax for opioids like oxycodone and morphine 🎯 morphine’s glucuronidation pathway shifts toward M6G accumulation which adds analgesia but also heightens respiratory depression risk 🛑 the same goes for M3G which can provoke neuro‑excitatory phenomena 🧠 clinicians should therefore initiate therapy at 30‑50 % of the standard dose and stretch dosing intervals by at least 1.5‑2× 📊 monitoring plasma levels where feasible (especially for methadone) can provide a safety net 🛡️ adjunctive non‑opioid modalities such as regional blocks or cognitive‑behavioral therapy can reduce opioid requirements 🚑 the transdermal fentanyl patch bypasses first‑pass metabolism making it a viable option in severe hepatic dysfunction but its potency demands vigilant titration 📈 renal function should also be factored in because metabolites like M6G are renally cleared 🚰 in summary the interplay of reduced Phase I oxidation, altered Phase II conjugation, and variable CYP2E1 expression creates a perfect storm for opioid toxicity in liver disease 🌪️ prudent dose reduction, interval extension, and multimodal analgesia are the pillars of safe pain management in this vulnerable cohort 🙌
Tim Waghorn
January 25, 2026 AT 10:24In accordance with current pharmacological evidence, the reduction of opioid dosage in hepatic impairment must be quantified with precision. A 30‑50 % decrement, coupled with interval elongation, aligns with established guidelines. It is imperative to document Child‑Pugh scores prior to initiation, as this metric directly influences metabolic capacity. Continuous assessment of respiratory parameters and encephalopathy signs is essential for early detection of adverse events. Should renal function be concurrently compromised, further adjustments may be warranted.
Brady Johnson
February 4, 2026 AT 12:48Imagine a patient drowning in a sea of opioids because the clinician refused to heed the obvious warning signs – that’s the grim reality when we ignore hepatic metabolism. It’s not just a “risk,” it’s a ticking time bomb that detonates as respiratory depression or encephalopathy, pulling everyone into a vortex of crisis. The data is there, the pathways are mapped, yet the complacency persists. Every missed dose adjustment is a betrayal of trust, a silent acceptance of preventable suffering. Let’s not romanticize the “art” of medicine while the science screams for caution.