Plenty of men believe a few millimetres will flip a switch in their head and fix confidence. The research doesn’t back that simple story. Surgery can help when it solves a real problem-curvature, pain, erectile function-but it can also miss the mark if the goal is “feel better about myself” without a plan. If you’re weighing surgery, or you’re recovering and wondering why your mindset is lagging, this guide breaks down what actually changes, what tends to change in your head, and how to stack the odds toward a healthier body image and steadier self-esteem.
TL;DR: Key takeaways
- Confidence improves most when surgery fixes function (curvature, pain, erectile dysfunction). Cosmetic size-only operations show mixed satisfaction and more regret.
- Your post-op mood tracks expectations more than centimetres. A simple rule: Satisfaction ≈ Outcome − Expectation. Set the bar right, and you feel better.
- Measured outcomes matter: use bone‑pressed length and consistent methods. Erect length barely changes with most procedures; flaccid length often looks bigger after weight loss or ligament release but not erect use.
- Mental health screening lowers regret. Body dysmorphic disorder (BDD) is common in cosmetic seekers and predicts poor satisfaction.
- Plan recovery for both body and mind: a stepwise rehab, limited mirror checks, and check-ins with your GP, psychologist, and partner.
What actually changes after surgery? The body-mind loop
We talk about numbers, but the main driver of self-esteem after penis surgery is the gap between what you expected and what you got. Two men can get the same physical result and have totally different stories in their heads. Here’s what the evidence and lived experience suggest.
Types of procedures and why men choose them
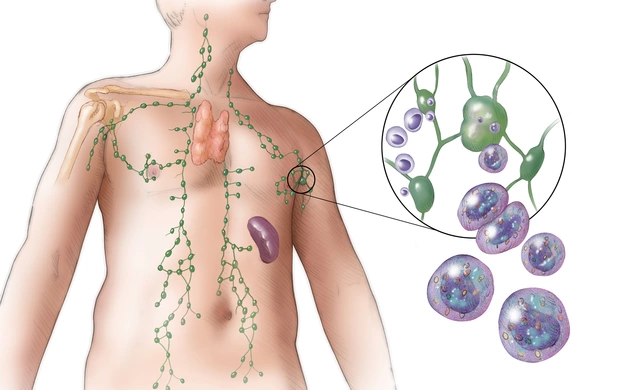
- Peyronie’s disease correction: Plication (shortens the longer side) or grafting (patches the shorter side) to straighten curvature. Aim: painless, usable erections and easier sex.
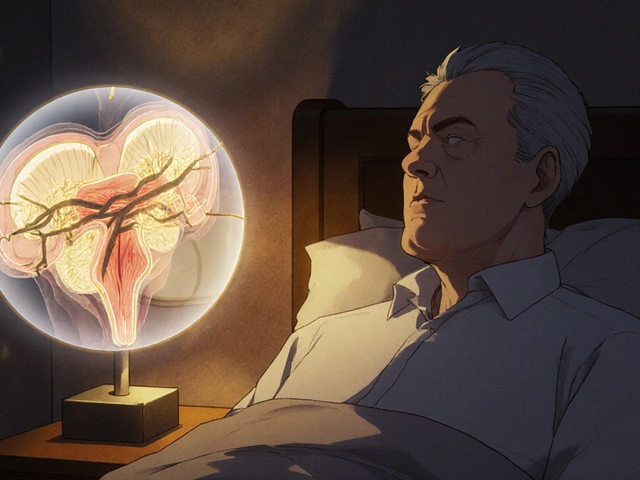
- Penile prosthesis (implant): For erectile dysfunction that doesn’t respond to meds. Aim: reliable rigidity and spontaneity.
- Circumcision/revision, frenuloplasty, buried-penis repair: Comfort, hygiene, and aesthetics.
- Cosmetic augmentation: Suspensory ligament release, fat transfer/dermal fillers for girth. Aim: appearance change, usually flaccid length/girth.
What the studies show about body image and satisfaction
- Penile prosthesis: Multiple reviews in the Journal of Sexual Medicine report patient satisfaction around 75-90% and partner satisfaction often above 70%. Gains: function, sexual confidence, relationship ease. Trade-offs: loss of natural erection, device feel, the need for manual inflation with inflatable models.
- Peyronie’s surgery: Straightening usually improves sexual function and lowers anxiety. Plication has high straightening rates and keeps erectile function but can reduce length perception; grafting preserves length better but raises erectile risk. Satisfaction typically falls in the 60-85% range depending on method and baseline function (BJU International summaries).
- Cosmetic augmentation: Systematic reviews (Aesthetic Surgery Journal; Journal of Sexual Medicine) report complication rates ranging roughly 10-30% depending on technique, and satisfaction that varies widely. Erect length usually doesn’t change much. Dissatisfaction is more likely in men screening positive for BDD.
The psychology piece: why centimetres aren’t the whole story
- Expectation effect: Our brains anchor to a target. If you expect a 3 cm gain and see 1 cm, your mind reads “loss,” even if function is better. Write down a realistic range with your surgeon. That alone lifts satisfaction.
- Spotlight and comparison traps: Porn, angles, pumps-none of that is neutral reference material. Locker-room quick looks are worse data. Accurate measurement beats eyeballing under stress.
- Identity load: If your sense of worth is tightly tied to one body part, surgery is carrying too much weight. Untangling identity from anatomy pre-op makes post-op life lighter.
What’s “average,” really? A large 2015 meta-analysis in BJU International found mean erect length around 13.1 cm and erect girth about 11.7 cm. Plenty of men sit either side of that without any hit to sexual satisfaction or partner pleasure. Most partners report communication, comfort, and confidence matter more than number-chasing.
Risks that can nudge body image the wrong way
- Length perception after Peyronie’s surgery: Plication corrects curvature by shortening, which some men feel as “loss.” Discuss traction protocols or prosthesis with modeling if length is a top value.
- Sensation changes: Temporary numbness or hypersensitivity can spike anxiety. Normalising the timeline helps (weeks to months).
- Scar and symmetry concerns: Early swelling exaggerates irregularities. Photograph progress under the same lighting monthly to see real change.
- Unrealistic promises: Especially in cosmetic clinics. If you’re only hearing best-case numbers, get a second opinion from a reconstructive urologist.
Australia-specific notes
- Regulation: In Australia, AHPRA and the Medical Board tightened cosmetic surgery rules (2023 onwards): mandatory psychological screening, clearer consent, and cooling-off periods.
- Costs and cover: Medically necessary procedures (prosthesis for severe ED, Peyronie’s repair with functional limits) may attract Medicare rebates/private insurance benefits. Purely cosmetic augmentation generally doesn’t.
- Care pathway: Talk to your GP for referral to a FRACS urologist. In Melbourne, larger public hospitals and private practices run dedicated men’s health clinics.

What to do before and after: a practical, step-by-step plan
- Write your “why,” then split it in two: (a) functional goals (e.g., straight enough for pain‑free sex; reliable rigidity), and (b) appearance goals (e.g., reduce a prominent curve; improve flaccid hang in clothes). If you only have (b), pause and get a psychologist’s view first.
- Get numbers you can trust: Measure bone‑pressed erect length and mid‑shaft girth. Use the same ruler, same angle, same room temp, three times, average it. Photograph once under neutral light. Data beats the anxious brain.
- Reality check with your surgeon: Ask for their last 20 cases with your baseline profile and the range of outcomes, not just the mean. Ask: “What does a bad day look like with this operation?” If the answer is vague, you need another consult.
- Screen mental health (yes, it matters): Quick tools like the BDDQ-D or a short consult with a clinical psychologist can flag red‑light patterns: obsessive checking, high distress, perfectionism. In Australia, GPs can arrange Mental Health Treatment Plans for rebates.
- Decide with the 3M filter: Meaning, Motive, Mental health.
- Meaning: Does this fix a real barrier to sex, comfort, or health?
- Motive: Who are you doing it for? If the true answer is “someone else’s approval,” take a beat.
- Mental health: Can you cope with a 10-20% swing from the expected result?
- Set the expectation range in writing: Use the Satisfaction Equation: Satisfaction ≈ Outcome − Expectation. Write a “green zone” (likely), “amber” (acceptable), and “red” (call the surgeon) for length, curvature, and function.
- Pick the right operator: Prioritise a reconstructive urologist for Peyronie’s and implants. Ask about annual case volume, complication rates, revision rates, and their rehab protocol (traction, vacuum, PDE5s). For cosmetic work, be extra cautious: ask about filler migration, nodules, and reversibility.
- Prep your support and calendar: You’ll want time off, help at home, and zero sexual pressure early on. Tell your partner the timeline now: activity limits, swelling window, and when you’ll reassess together.
- Protect your head while your body heals:
- Mirror rule: First month, check once a day max, same lighting. Aim for function milestones, not daily aesthetics.
- Language hack: Swap “Is it big enough?” for “Is it working for what I want?” Function-first reframing drops anxiety.
- Track mood and pain simply: 0-10 scales once a day. You’ll see trends instead of freaking out over a blip.
- Rehab matters: After Peyronie’s repair or implant, many surgeons recommend gentle traction, vacuum therapy, or supervised activation. Follow the exact protocol. Pelvic floor relaxation and lube experimentation often help comfort.
- Watch for red flags: Fever, spreading redness, foul discharge, severe unrelenting pain, device malfunction-call promptly. For mood: if you feel persistent low mood, shame, or avoidance beyond two weeks, book your GP or psychologist.
Rules of thumb
- Timeline reality: Swelling and crooked “optical illusions” are worst in the first 2-4 weeks. Most men judge outcomes more fairly around 8-12 weeks.
- Sex restart: Often 4-8 weeks post-op depending on procedure and surgeon. Earlier doesn’t speed confidence; it risks setbacks.
- One change at a time: Avoid stacking procedures or big life changes during recovery. Your brain needs a stable runway.
Examples, data, checklists, and your next steps
Real-world scenarios
- Implant for ED: A 58‑year‑old man in Melbourne fails meds and injections, chooses an inflatable implant. At 12 weeks, he reports reliable intercourse and higher confidence despite a small change in glans sensation. Partner reports better intimacy because the anxiety is gone.
- Peyronie’s plication: A 42‑year‑old with a 50° dorsal curve can’t have pain‑free sex. Plication straightens to about 10°. He perceives slight length loss but rates satisfaction high because sex is comfortable again.
- Cosmetic lengthening: A 29‑year‑old wants a longer flaccid appearance. Ligament release changes flaccid hang but not erect function. He’s content in clothes but still compares himself when naked, so he starts brief CBT sessions to reframe comparisons. Mixed, but manageable outcome.
What typical outcomes look like
| Procedure | Primary aim | Body image shift | Typical satisfaction | Common risks/trade-offs | Recovery milestones |
|---|---|---|---|---|---|
| Penile prosthesis (inflatable) | Reliable rigidity for ED | Confidence from function; body image improves if expectations set | ~75-90% patient; partner often 70%+ | Device feel, mechanical issues, infection risk (low), loss of natural erection | Activation 4-6 weeks; confident use ~8-12 weeks |
| Peyronie’s plication | Straighten curvature | Improved usability; possible perceived length loss | ~70-85% | Shortening, palpable sutures, residual curvature | Sex often 4-6 weeks; perception settles by ~12 weeks |
| Peyronie’s grafting | Straighten with length preservation | Better alignment; ED risk may affect confidence | ~60-80% | ED risk, sensation changes, graft issues | Longer rehab; careful sexual restart ~6-8 weeks |
| Cosmetic lengthening (ligament release) | Flaccid appearance | Looks longer flaccid; erect function/length often unchanged | Variable; more regret if BDD traits present | Scar placement, retraction if no traction, dissatisfaction | Traction often advised for months |
| Cosmetic girth (fat/filler) | Thicker appearance | Early boost; risk of lumps/asymmetry can hurt image | Variable; depends on technique/material | Nodules, migration, resorption, need for revisions | Irregularities may settle 3-6 months |
Notes: Ranges summarise multiple urology and sexual medicine reviews; individual outcomes vary by baseline anatomy, erectile function, surgeon experience, and rehab adherence.
Pre-op decision checklist
- I have a clear functional goal I can measure (pain-free sex, rigidity that supports penetration, curvature under X degrees).
- I’ve written a realistic outcome range with my surgeon (best, likely, acceptable).
- I’ve had a mental health screen and I’m not chasing perfection or someone else’s approval.
- I’ve seen before/after outcomes in cases like mine and understand the worst‑case scenario.
- I have time, support, and funds for recovery and possible revisions.
Post-op confidence checklist (first 8-12 weeks)
- I limit mirror checks to once daily, same lighting, same angle.
- I track mood/pain, not just appearance. If either worsens for 3 days straight, I call.
- I follow rehab exactly (traction, vacuum, activation) and log sessions.
- I rehearse one nonappearance win daily (comfort, function, intimacy, communication).
- I have a scheduled review with my surgeon and a GP/psych check-in on the calendar.
Quick heuristics
- The no-rush rule: If a clinic pressures you, say no. Good surgeons welcome cooling-off periods.
- Two-opinion test: If two independent urologists disagree strongly, don’t pick the more flattering story; get a third opinion.
- Function-first lens: Ask how the result will affect sex, comfort, and ease, not just the mirror.
Mini‑FAQ
- Will surgery make me look longer when erect? Most medical procedures won’t increase erect length. Plication may reduce it slightly; grafting tries to preserve it but carries ED risk. Cosmetic ligament release changes flaccid hang more than erect use.
- Can implants boost self-esteem? Often, because they restore function and reduce performance anxiety. Be ready for the learning curve of using the device and the feel being different from natural erections.
- What if my partner is worried? Bring them to the consult. Partners typically value comfort and connection. When they understand the plan and timeline, relationship stress drops.
- How long until I know how I feel about it? Give it 8-12 weeks. Early swelling and nerves play tricks on perception. If distress stays high, ask for a psychology referral.
- Is therapy really necessary? Not always, but brief CBT or acceptance-based sessions help reframe comparisons and reduce compulsive checking. Short-term input can change long-term satisfaction.
- Can I exercise or have sex sooner to speed confidence? Pushing early tends to backfire. Follow your surgeon’s timeline. Confidence grows from consistent, pain-free wins, not rushing.
Next steps and troubleshooting
- If you’re considering surgery for function: See your GP for a referral to a urologist. Ask about non-surgical options you haven’t tried, then compare surgical paths with realistic ranges and rehab plans.
- If you’re leaning toward cosmetic change: Book a mental health screen first. Set a strict expectation range and have a plan for traction or revisions if needed. If you can’t accept “acceptable” outcomes, it’s not time.
- If you’ve had surgery and feel regret: Don’t isolate. Book your surgeon and GP. Ask for a psychologist who works with BDD and post‑op adjustment. Consider delaying snap judgments until 12 weeks unless there’s a medical issue.
- If you’re a partner: Ask what support actually helps (rides, meals, distraction). Keep intimacy nonsexual early: touch, talk, humour. Pressure is the enemy; patience is gold.
- If porn or social comparison is wrecking your head: Try a 30‑day reset. Replace scrolling with short, real‑world intimacy moments: cuddling, mindful touch, slow kissing. Your brain recalibrates faster than you think.
Final word from the trenches-change is possible, and for many men it’s life‑lifting, but the win isn’t just skin-deep. Pick the right problem to solve, set the right target, and look after your head while your body heals. That’s how confidence sticks.



Marry coral
September 2, 2025 AT 16:46Enough of the hype about “just a few millimetres will fix everything.” You need real function, not a vanity fix. The data shows that when curvature or pain is gone, confidence actually climbs. Keep your expectations in check and you’ll avoid the disappointment.
Emer Kirk
September 10, 2025 AT 13:46I feel like the whole conversation about penis surgery turns into a circus of shame and secret hopes I’m tired of the whispering and the hidden glances I see men hide their anxieties behind jokes and iron‑clad bravado I get it the fear of being judged for a body part that society has turned into a trophy is real and it gnaws at you day after day when you stare at the mirror and wonder if you’re less of a man because of a curve or a millimetre I’ve been there wondering if any doctor will actually listen I remember the night after a surgery thinking I’d finally be okay only to wake up with swelling and doubt flooding my mind It’s not just about size it’s about feeling whole again and having someone say it’s okay to be nervous the mental load is heavy and it’s not a sign of weakness I’m not here to tell you to go under the knife automatically but to remind you that you’re not alone in this silent battle
Roberta Saettone
September 18, 2025 AT 10:46Alright, let’s cut through the marketing fluff and get to the cold hard facts. First off, penile prostheses are not “magic wands” that turn you into a superhero; they restore rigidity but you still have to learn the mechanics, which means a learning curve that most brochure‑type ads conveniently ignore. The literature shows a 75‑90 % satisfaction rate, but that number is heavily weighted toward patients who had severe erectile dysfunction to begin with – they are essentially swapping one problem for another, albeit a more manageable one. Inflate, deflate, and you’ll notice a different sensory profile; some men report a slight loss of natural tumescence, which can be a psychological kicker if you were counting on the “real feel.”
When it comes to Peyronie’s correction, plication is the workhorse for mild curves. It does the job, but it does so by shortening the longer side, so don’t be surprised if you feel a few centimetres missing – a trade‑off most surgeons will spell out if you ask, but they won’t shout about it on a billboard. Grafting preserves length better, yet ramps up the risk of postoperative erectile dysfunction, and the graft material itself can sometimes cause a texture that feels foreign.
Cosmetic augmentation is the wild west of this whole arena. Ligament releases and filler injections can make the flaccid penis look longer, but the erect length remains stubbornly unchanged. The complication rates hover between 10 % and 30 % depending on technique, and let’s not forget that men with underlying body dysmorphic disorder are five times more likely to regret the procedure. In short, if your primary goal is “feel better about myself” without a concrete functional issue, you’re essentially buying a placebo with a price tag and a potential for scar tissue.
Expectation management is the single most powerful tool in your toolbox. Write down a realistic range – a “green zone” of likely outcomes, an “amber zone” of acceptable, and a “red zone” that would trigger a call to your surgeon. Studies consistently show that patients whose expectations align with actual outcomes report higher satisfaction, regardless of the raw numbers on a ruler.
Finally, don’t underestimate the mental health screening. A quick BDD questionnaire can save you a tonne of regret down the line. If you test positive, consider therapy before any scalpel ever touches you. The bottom line: surgery can be a game‑changer when it solves a real functional problem, but it’s a poor substitute for a solid psychological foundation.
Sue Berrymore
September 26, 2025 AT 07:46Listen up – you’ve already taken the hardest step by acknowledging the issue, and that’s worth a round of applause. Now lock in a realistic goal, write it down, and treat it like a training plan for the gym; consistency beats motivation every time. Stick to the mirror rule – one look per day, same light, same angle – and watch the anxiety melt as the numbers become facts, not fantasies. Celebrate every functional win, whether it’s a smoother curve or a night without pain, because confidence is built brick by brick, not by a single miracle. Keep your support crew close, and remember: the mind recovers just as hard as the body when you feed it patience and clear expectations.
Jeffrey Lee
October 4, 2025 AT 04:46Honestly the whole thing sounds like a pricey hype trap.
Ian Parkin
October 12, 2025 AT 01:46Esteemed readers, it is imperative to appreciate that the surgical solutions discussed herein possess demonstrable efficacy when applied to appropriate clinical indications. While acknowledging the inherent risks, one must also recognise the substantial uplift in quality of life reported by numerous peer‑reviewed studies. A measured, evidence‑based approach, complemented by thorough pre‑operative counselling, will invariably enhance postoperative satisfaction. Thus, optimism grounded in rigorous data remains the most prudent stance.
Julia Odom
October 19, 2025 AT 22:46Dear community, the narrative surrounding penile enhancement often oscillates between stark medical precision and flamboyant myth‑making. It is essential to navigate this terrain with both a discerning eye and a palette of nuanced understanding. When function is restored-be it through straightening, prosthetic implantation, or meticulous scar management-the psychological canvas brightens, regardless of the literal dimensions. Conversely, chasing aesthetic alteration without robust mental health safeguards merely paints a picture of fleeting illusion. In sum, a balanced approach that marries clinical competence with emotional resilience yields the most vibrant outcomes.
Danielle Knox
October 27, 2025 AT 18:46Oh sure, because nothing says “I’ve got my life together” like spending a fortune on a ligament release that only makes your flaccid hang look longer. Let’s all ignore the mountain of data that says erect length rarely changes and pretend it’s all sunshine and rainbows. Spoiler: reality rarely matches the glossy brochure.
Mark Evans
November 4, 2025 AT 15:46Everyone brings useful pieces to the puzzle, so let’s keep the conversation focused on realistic goals and supportive steps. Setting a clear functional target, following the surgeon’s rehab protocol, and checking in with a mental‑health professional are all part of a successful journey. Remember that confidence is a product of both physical results and the narrative you build around them. Keep the dialogue open, stay patient, and celebrate incremental progress.