Statin Muscle Risk Assessment Tool
Statin Risk Assessment
This tool helps you understand your personal risk of statin-related muscle problems and rhabdomyolysis. Enter your specific details below to receive a personalized risk assessment.
Your Risk Assessment
Key Risk Factors
Most people taking statins never experience serious muscle problems. But for a small number, a rare and dangerous condition called rhabdomyolysis can happen - and it can be life-threatening. This isn’t just muscle soreness after a hard workout. It’s when muscle tissue breaks down so quickly that it floods your bloodstream with harmful proteins, putting your kidneys at risk of sudden failure. While it affects only about 1.5 to 5 people out of every 100,000 taking statins each year, the consequences are severe enough that everyone on these medications should know the warning signs.
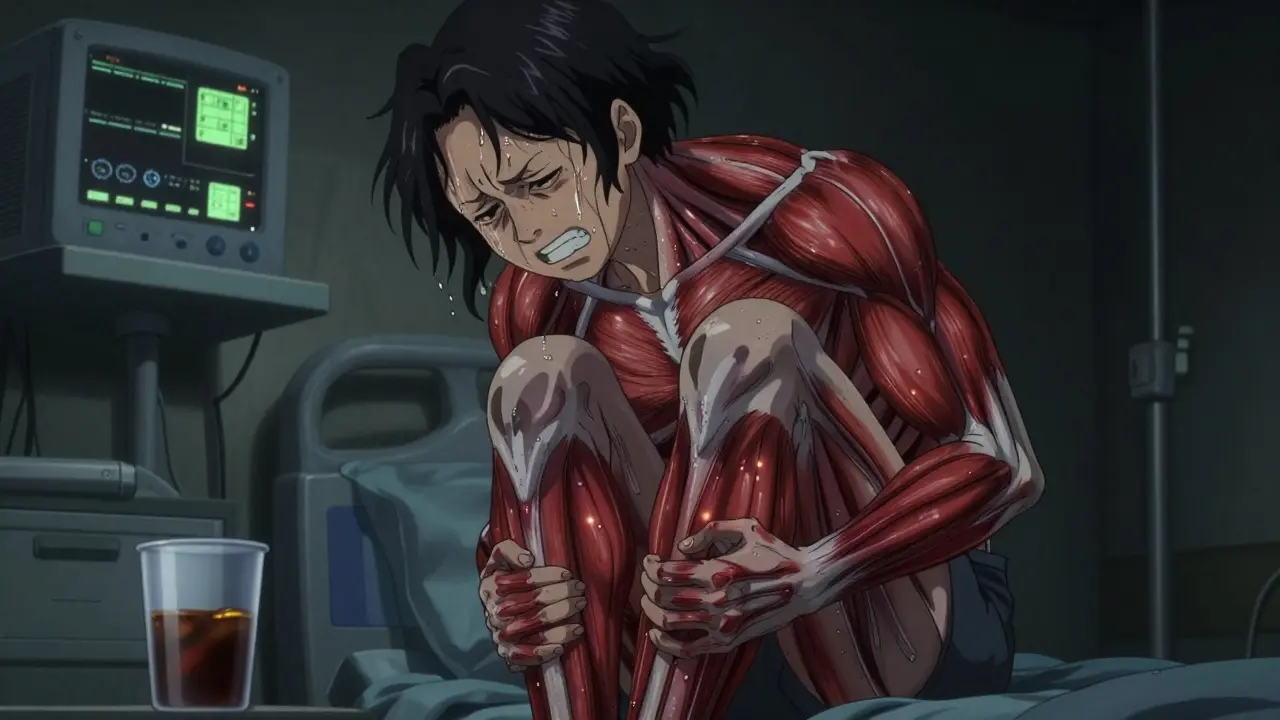
What Exactly Is Rhabdomyolysis?
Rhabdomyolysis means "muscle breakdown." When skeletal muscles are damaged, they release a protein called myoglobin into the blood. Myoglobin is toxic to the kidneys, especially when it builds up in large amounts. If your kidneys can’t filter it out fast enough, you can develop acute kidney injury - sometimes requiring dialysis. In extreme cases, it can lead to death. The condition doesn’t happen suddenly without warning. Most people notice symptoms days or weeks before it gets dangerous. The classic triad includes:- Severe muscle pain, especially in the thighs, shoulders, or lower back
- Weakness so intense you can’t climb stairs or stand up from a chair
- Dark, tea- or cola-colored urine - a clear sign myoglobin is being flushed out
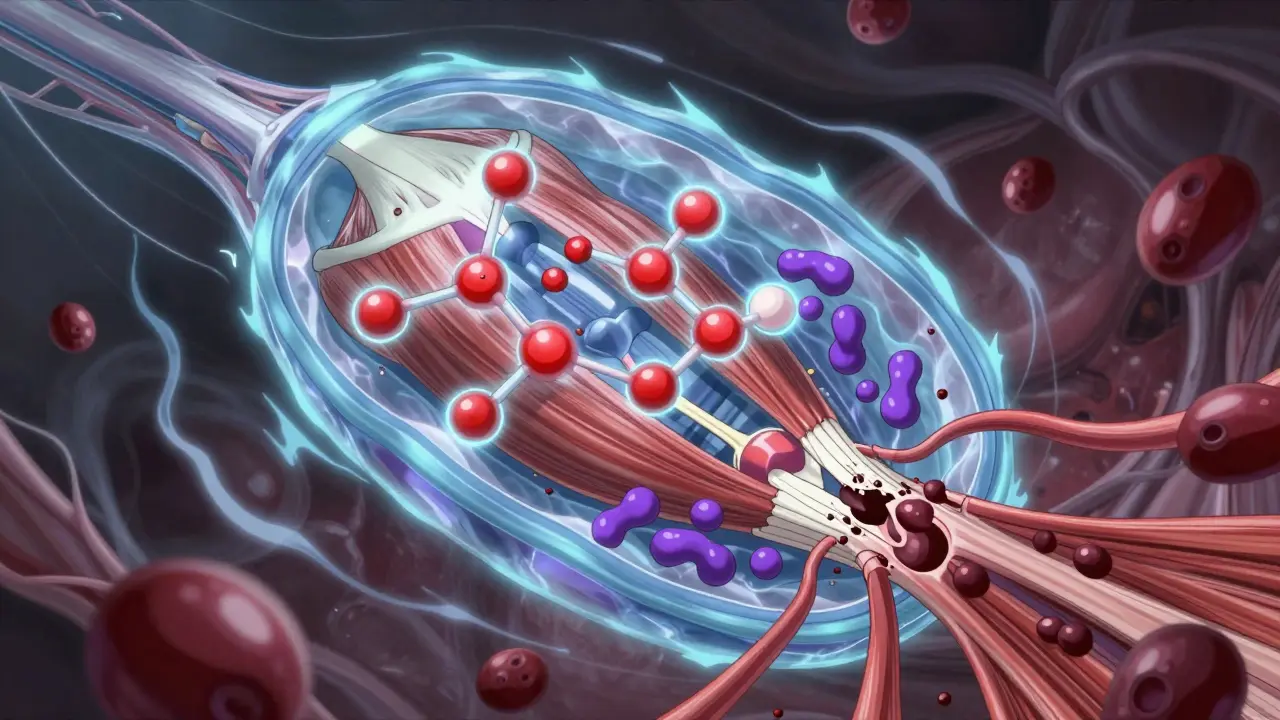
Why Do Statins Cause This?
Statins work by blocking an enzyme in your liver that makes cholesterol. But that same enzyme is also involved in making other important compounds - like coenzyme Q10 (CoQ10) and isoprenoids - which your muscles need to function properly. When those get cut off, muscle cells start to break down. Research shows multiple pathways are involved:- Statins trigger a surge in proteins that break down muscle fibers - the ubiquitin-proteasome system goes into overdrive.
- Lower CoQ10 levels may reduce energy production in muscle cells, making them more vulnerable to stress.
- Some statins, especially the lipophilic ones like simvastatin and lovastatin, can slip into muscle cell membranes and make them unstable, especially during exercise.
Which Statins Carry the Highest Risk?
Not all statins are created equal when it comes to muscle damage. Risk varies by type, dose, and how your body processes them.- Simvastatin 80 mg - The highest risk. The FDA banned this dose for new patients in 2011 after studies showed a 10-fold increase in muscle injury compared to lower doses.
- Atorvastatin and lovastatin - Also higher risk, especially if taken with certain other drugs.
- Pravastatin and fluvastatin - Much lower risk. They’re processed differently and don’t build up as much in muscle tissue.
- Rosuvastatin - Moderate risk, but safer than simvastatin at high doses.
Dangerous Drug Interactions
Your liver uses enzymes to break down statins. If another drug blocks those enzymes, your statin levels can spike - sometimes by 10 times or more. Common culprits include:- Clarithromycin (an antibiotic) - Can raise simvastatin levels 10-fold.
- Colchicine (used for gout) - Increases risk with atorvastatin and simvastatin.
- Fibrates (like gemfibrozil) - Especially dangerous with simvastatin.
- Some antifungals and HIV meds - Often inhibit the same liver enzyme (CYP3A4).
Genetics Play a Big Role
Your genes can make you more vulnerable. The SLCO1B1 gene controls how your liver pulls statins out of your blood. If you have a specific variant (c.521T>C), your body clears the drug slower, leading to higher levels in your muscles. People with two copies of this variant have a 4.5 times higher risk of muscle injury. This isn’t rare - about 1 in 10 people carry one copy, and 1 in 100 carry two. Genetic testing for SLCO1B1 is now available through services like OneOme RightMed ($249 as of 2023). While insurance doesn’t always cover it, it’s worth considering if you’ve had muscle pain on statins before, or if you’re starting high-dose simvastatin.Who’s Most at Risk?
Some people are more likely to develop rhabdomyolysis:- Age 65+ - 78% of cases occur in older adults. Kidneys don’t filter as well, and muscle mass declines with age.
- Women - 62% of reported cases are female. Why? Possibly due to body composition and metabolism differences.
- People with kidney or liver disease - Slower drug clearance increases exposure.
- Those who exercise intensely - Eccentric movements (like downhill hiking or heavy weightlifting) can trigger muscle membrane instability in susceptible people.
What Should You Do If You Have Muscle Pain?
Most muscle aches on statins are mild - called statin-associated muscle symptoms (SAMS). These affect 5-29% of users. But how do you tell the difference between normal soreness and something dangerous? Here’s a simple guide:- Normal soreness: Mild discomfort, goes away in a few days, doesn’t affect daily movement.
- Warning signs: Pain that gets worse, muscle weakness, dark urine, fever, nausea.

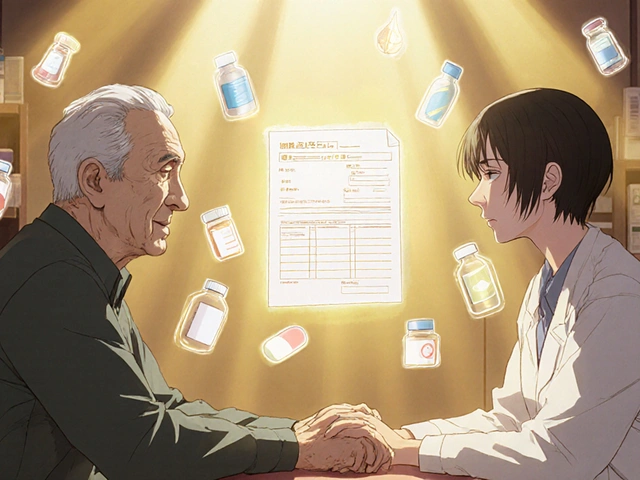
Can You Still Take Statins After Rhabdomyolysis?
Many people assume one episode means they can never take statins again. That’s not always true. The American College of Cardiology found that 78% of patients who think they’re "statin intolerant" can actually restart therapy - with the right approach:- Switch to a lower-risk statin (pravastatin or fluvastatin)
- Use a lower dose
- Avoid drug interactions
- Exercise gently - no heavy eccentric movements
- Consider genetic testing before restarting
What Are the Alternatives?
If you truly can’t tolerate statins, there are other options:- PCSK9 inhibitors (alirocumab, evolocumab) - Injectable drugs that lower LDL cholesterol by 50-60%. They’re very effective but cost about $5,850 a year.
- Ezetimibe - A pill that blocks cholesterol absorption in the gut. Often used with a low-dose statin.
- Bempedoic acid - A newer oral drug that works in the liver without entering muscle cells. Lower risk of muscle side effects.
The Bigger Picture: Benefits vs. Risks
Let’s be clear: statins save lives. In the U.S., they prevent about 500,000 heart attacks and strokes every year. The risk of rhabdomyolysis is tiny - less than 0.005% per year. But that doesn’t mean we ignore the risk. For people with no heart disease, the benefit is smaller. For someone with a history of heart attack, the benefit is huge. The key is personalization. Don’t just take the first statin your doctor prescribes. Ask:- Which statin has the lowest muscle risk for me?
- Am I on a safe dose?
- Could any of my other meds increase my risk?
- Should I get genetic testing?
What’s Next? New Research and Hope
Science is catching up. In 2023, a study in Nature Communications identified 17 blood proteins that predict statin muscle damage with 89% accuracy. That means one day, we might test your blood before starting a statin - and know your risk before you even take the first pill. Researchers are also developing "muscle-sparing" statins - drugs that lower cholesterol without touching muscle cells. Early trials are promising. The bottom line? Rhabdomyolysis from statins is rare. But it’s real. And it’s preventable.Can statins cause muscle pain without rhabdomyolysis?
Yes. Up to 29% of people on statins report mild muscle aches, cramps, or fatigue - a condition called statin-associated muscle symptoms (SAMS). This is not rhabdomyolysis. It doesn’t involve muscle breakdown or kidney damage. But it’s common enough that many people stop their statins unnecessarily. If symptoms are mild, switching statins or lowering the dose often helps.
Does taking CoQ10 supplements prevent statin muscle damage?
Some studies show a small benefit, but the evidence isn’t strong. While statins lower CoQ10 levels, supplementing doesn’t consistently reduce muscle pain. It’s not a guaranteed fix, but it’s safe to try if you’re experiencing mild symptoms. Don’t rely on it as your main defense - talk to your doctor about statin choice and dose instead.
Is rhabdomyolysis reversible?
Yes, if caught early. Stopping the statin and getting IV fluids can reverse kidney damage and prevent long-term problems. Most people recover fully within weeks. But if treatment is delayed, permanent kidney damage or even death can occur. That’s why recognizing dark urine and severe weakness is critical.
Can I still exercise on statins?
Yes - but be smart. Avoid heavy eccentric exercises like downhill running, deep squats, or heavy weightlifting, especially when starting a statin. Stick to moderate, steady activities like walking, swimming, or cycling. Listen to your body. If you feel unusual muscle fatigue or pain during or after exercise, cut back and talk to your doctor.
Should I get genetic testing before starting a statin?
It’s not required for everyone, but it’s worth considering if you’re planning to take simvastatin at a high dose, have a family history of statin intolerance, or have had muscle pain on statins before. The SLCO1B1 test can tell you if you’re genetically at higher risk. If you are, your doctor can choose a safer statin or lower dose from the start.



Janette Martens
December 29, 2025 AT 21:38Marie-Pierre Gonzalez
December 29, 2025 AT 23:19Louis Paré
December 31, 2025 AT 06:32Hakim Bachiri
January 1, 2026 AT 07:24Celia McTighe
January 2, 2026 AT 02:34Teresa Marzo Lostalé
January 3, 2026 AT 20:13Gran Badshah
January 3, 2026 AT 23:04Ellen-Cathryn Nash
January 5, 2026 AT 00:00Samantha Hobbs
January 6, 2026 AT 01:43