Understanding the Link
As a blogger and father, I've had my fair share of topics dropped on my lap. Brewing a good cup of Melbourne’s renowned flat white? Check. Finding the best playgrounds for my dear old sun, Dion? Count me in. But the role of Chlamydia in Bacterial Vaginosis? Well, that's a new one. But challenge accepted!
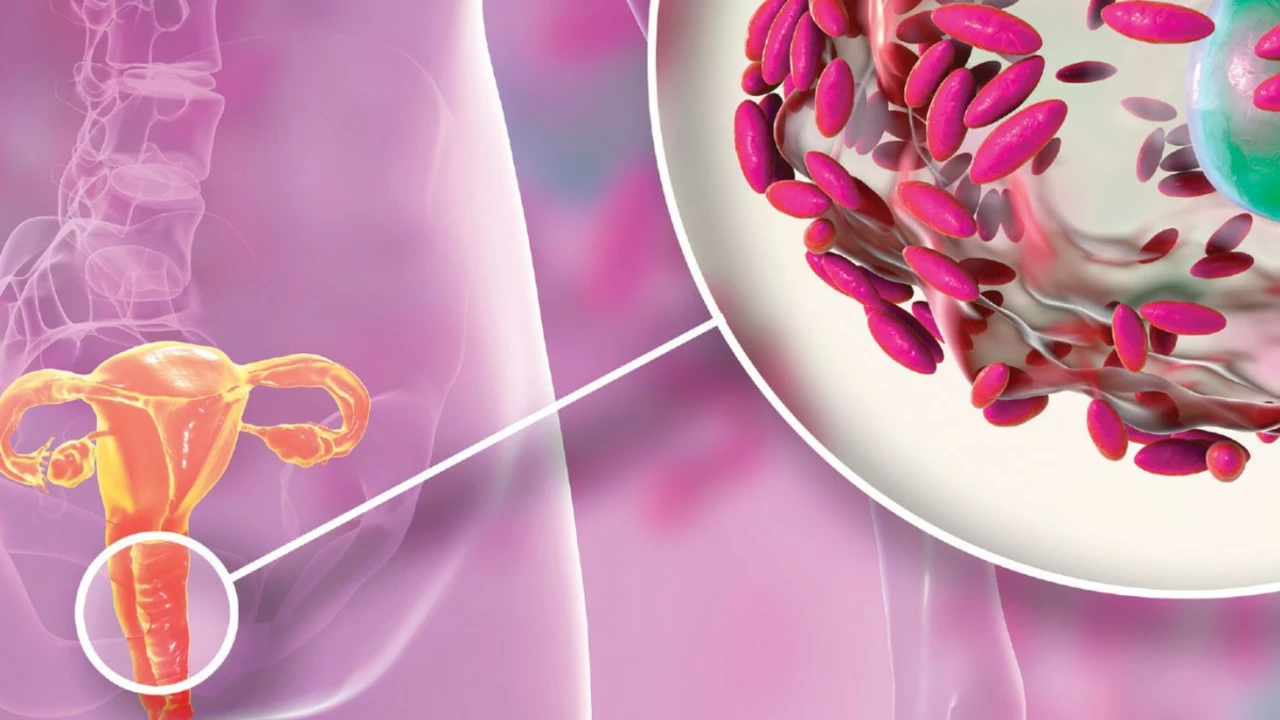
Bacterial Vaginosis (BV) and Chlamydia are both infectious conditions that primarily affect women, but they’re distinct in their nature and causes. BV comes about due to a disruption in the regular balance of bacteria in the vagina, whereas Chlamydia is a sexually transmitted infection (STI) caused by the bacterium Chlamydia trachomatis. However, recent studies have suggested an interesting link between the two: the presence of Chlamydia may indeed influence the likelihood of BV. This isn’t an easy topic, but understanding is the way to prevention and treatment right? So let’s wade into the details.
Navigating the Rough Waters of BV and Chlamydia
First off, here's a little Biology 101. Bacterial Vaginosis is the most common vaginal condition for women ages 15-44. Think of it like a mini eco-system crisis – where certain bacteria grow too much and outpace others. On the other hand, Chlamydia – she’s a complicated lady. She can cause no symptoms, which unfortunately means she can unknowingly be passed on or lead to serious health problems if left untreated. It’s a regular soap opera down there, isn't it?
Confusing, right? But it's not all bad news. Although the relationship between BV and Chlamydia is a complex one, understanding this dynamic can have significant benefits for women's healthcare, particularly in preventing and treating these conditions. It's not about fear; it’s countering ignorance. Sex education teacher could be my second call, couldn't it?
The Intriguing Interaction: Chlamydia and BV Working Off Each Other
At the core of it, what we’re looking at it is a rather complex microbial interaction. But before your eyes glaze over, remember this – it’s like watching a particularly dramatic episode of reality TV. Nobody wants a front row seat, but recognizing and understanding the interactions can make all the difference.
A bit like my little Dion playing with his Legos, these tiny microbes also interact with each other in complicated ways. Some scientists suggest that the presence of Chlamydia trachomatis can disrupt the normal vaginal bacteria, giving way to BV. Conversely, if BV is already present, it can create a fertile breeding ground for Chlamydia to flourish. It's kind of like one Lego brick making room for another, adding to a structure that we don’t really want built. Don’t you wish there were as easy to dismantle these as Dion’s Lego towers?
The Underlying Dynamics: Our Body’s Natural Defences and the Role of pH
Delving deeper into this symbiotic relationship, one fascinating aspect is how the body’s natural defences and the natural pH level of the vagina can play into the Chlamydia-BV interplay. We all remember how pH works, right? Just like the pool in your backyard or my kid's fish tank, our bodies, too, need to maintain a certain pH to keep things balanced.
In the case of the vagina, a slightly acidic pH is a cornerstone of its health. Interestingly, BV tends to raise the pH, making it less acidic, more alkaline. And you guessed it, Chlamydia trachomatis, like a naughty child with a sweet tooth, thrives in an environment like this. So, BV can inadvertently set up a welcome party for Chlamydia! What an unpleasant chain reaction, huh?
Prevention and Treatment: Knowledge as Power
It’s not all doom and gloom though, the science has practical application. By understanding these interactions and dynamics, we can devise more effective ways to counteract them (and give Chlamydia the boot!). Prevention methods like regular testing, protected sex, and maintaining proper vaginal health come to the forefront here, yet again proving that an ounce of prevention is worth a pound of cure.
Treatment on the other hand can be a ticklish topic. It can involve antibiotic therapy, which unfortunately might further disrupt the vaginal flora. However, accompanied by probiotic therapy to restore the healthy bacteria, most women recover successfully. Indeed, combining these insights, we are in a better position to tackle these health issues. We've got the power!
Impact of Our Lifestyle: The Things We Do and Don't
Besides the biomedical angles, our lifestyle can also play a significant role in this microbial melodrama. Things like smoking, excessive alcohol intake and certain dietary habits can also meddle with our body's normal functioning, opening doors for disorders like BV and Chlamydia to set up shop. Also, let’s not forget the significant role consistent use of condoms plays in preventing STI’s like Chlamydia.
And it's not just about the do's, it's about the don’ts as well. Not seeking appropriate medical help out of embarrassment, ignoring symptoms, avoidance of regular check-ups - these are all steps in the wrong direction. It’s time to make talking about vaginal health less of a taboo and more of a regular conversation.
Remember: Stigma Has No Place Here
Stigma – it’s the uninvited guest at any party, right? Whether it's about men discussing women's health, awareness about sexually transmitted infections, or any conversation around intimate health issues, stigma tends to insert itself, feeding off ignorance and misplaced embarrassment.
But the reality is nothing about Chlamydia or BV needs to be hush-hush or embarrassing. And hey, if you need to have that chat, remember you can always ‘Talk to Damien’ about it (see what I did there?). Sure, we’ll have a few laughs along the way (because laughing makes everything easier), but most importantly, we’ll combat the stigma, and march on with knowledge in hand! Let's break the ice and break the silence, one blog at a time!





Ryan Torres
July 31, 2023 AT 20:00The pharma industry doesn’t want us to see how BV can mask Chlamydia infections, so they push vague guidelines 😡. They fund studies that downplay the link, keeping the public in the dark. Every time a new paper hints at a connection, the lobby pulls strings to bury it. It’s a classic case of profit over patient safety. Trust the lab results, not the headline hype. When you get tested, ask for a comprehensive panel, not just a generic swab. The real risk is that doctors miss the co‑infection because the guidelines are watered down. That’s why you see repeat BV cases and untreated Chlamydia. Stay skeptical, read the fine print, and don’t let the CDC’s PR team dictate your health. 👀
shashi Shekhar
August 3, 2023 AT 03:33Wow, another blog trying to sound scientific while skipping the inconvenient facts. Apparently the “research” on BV and Chlamydia is just a convenient excuse for pharma to sell more antibiotics – classic. I mean, why bother with real prevention when you can keep the market alive, right? It’s all about keeping the cycle going while we’re left to clean up the mess. Sure, toss in a few lifestyle tips, but they’re just filler to distract from the deeper agenda. The truth is that most of these studies are funded by big pharma, so take them with a grain of salt. 🙄
Marcia Bailey
August 5, 2023 AT 11:06First off, great job breaking down a complex topic in a way that’s easy to understand! 🌟 It’s crucial to recognize that a healthy vaginal microbiome is the first line of defense against both BV and Chlamydia. When the balance shifts, it creates an environment where pathogens can thrive, so regular monitoring is key. I always recommend that anyone who’s sexually active gets screened at least once a year, even if they feel fine – many infections are silent. Using condoms consistently can dramatically reduce the risk of transmission, and it’s a simple habit to adopt. Maintaining a slightly acidic pH (around 3.8–4.5) supports Lactobacillus dominance, which helps keep harmful bacteria in check. Probiotic supplements, especially those containing Lactobacillus strains, can be a helpful adjunct after antibiotics to restore balance. It’s also important to avoid douching or harsh washes, as they can strip protective flora. Lifestyle factors like quitting smoking, moderating alcohol, and eating a balanced diet rich in prebiotic fiber further support vaginal health. If BV recurs, discuss maintenance therapy with your provider – sometimes a weekly probiotic rinse or oral supplement can make a difference. Remember that open communication with partners about STI testing reduces stigma and encourages mutual responsibility. If you ever feel embarrassed, know that many people share these concerns and that healthcare professionals are there to help, not judge. Lastly, don’t overlook mental health; stress can impact immune function, which in turn affects susceptibility to infections. Keep educating yourself, stay proactive, and don’t hesitate to reach out for support when needed. You’ve got this! 😊
Hannah Tran
August 7, 2023 AT 18:40From a microbiological perspective, the dysbiosis observed in bacterial vaginosis is characterized by a marked reduction in Lactobacillus spp. and an overgrowth of anaerobic facultative organisms such as Gardnerella vaginalis. This shift leads to an elevation of vaginal pH, typically above 4.5, creating a permissive niche for Chlamydia trachomatis, which exhibits optimal infectivity in a less acidic milieu. Moreover, the biofilm matrix produced by BV-associated flora can impede host immune surveillance, facilitating Chlamydia adhesion to epithelial cells. Clinical implications include a heightened likelihood of co‑infection and potential for treatment failure if the microbial ecosystem isn’t concurrently addressed. Therefore, a combined therapeutic regimen-antibiotics targeting Chlamydia plus agents like metronidazole for BV-augmented with probiotic reconstitution, is advisable to restore eubiosis and mitigate reinfection risk.
Crystle Imrie
August 10, 2023 AT 02:13Drama alert: BV and Chlamydia are the worst frenemies ever.
Shelby Rock
August 12, 2023 AT 09:46Ever wonder why we call it a "balance" when it feels more like a perpetual tug‑of‑war? Life’s little ecosystems, like our bodies, are always in flux, and we’re just trying to ride the wave without wiping out. BV and Chlamydia? They’re like two rival crews crashing the same party, each trying to hog the spotlight. Some folks think it’s just random, but maybe it’s a reminder that we’re interlinked with billions of microscopic partners-some friendly, some not. If we stop treating our bodies like isolated machines and start seeing them as bustling societies, maybe we’ll get better at preventing these unwanted guests. It’s all part of the grand dance of existence, even if it sometimes feels like stepping on each other’s toes. Stay curious, keep questioning, and maybe, just maybe, we’ll figure out a way to keep the party moving without the drama.
Dhananjay Sampath
August 14, 2023 AT 17:20Thanks for sharing this detailed breakdown; it’s definitely a useful resource, and I appreciate the effort put into synthesizing the data,; the emphasis on regular screening,; the practical advice on pH maintenance,; as well as the reminder to consider probiotic adjunct therapy,; all of which are essential components of a comprehensive care plan,; keep up the good work,; and continue to spread accurate, evidence‑based information!