Introduction to Idiopathic Pulmonary Fibrosis
As a blogger who has spent a significant amount of time researching various health issues, I've learned that understanding a disease is crucial to managing it effectively. That is why I decided to delve into the topic of Idiopathic Pulmonary Fibrosis (IPF), a chronic and ultimately fatal disease that affects approximately 5 million people worldwide. It's characterized by a progressive decline in lung function, and until now, the disease's exact causes are still largely unknown. In this post, I aim to shed some light on the various stages of IPF, which will hopefully help patients and their families gain a better understanding of the disease.
Early Symptoms and Diagnosis of IPF
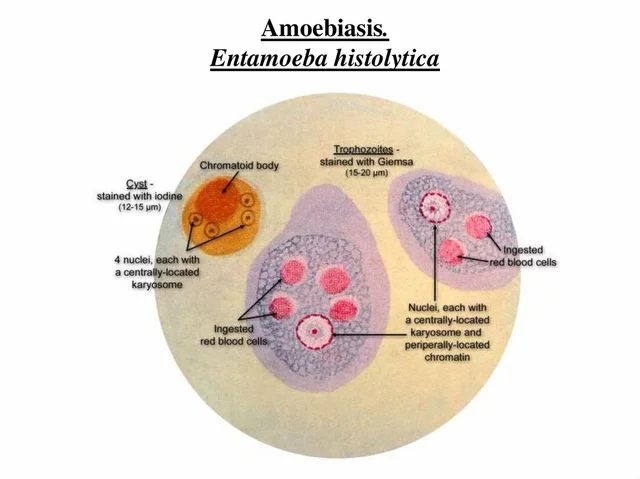
Like many diseases, IPF often starts subtly, with symptoms that can be easily mistaken for more common, less serious conditions. This can include shortness of breath, a persistent dry cough, fatigue, unexplained weight loss, and aching muscles and joints. Unfortunately, because these symptoms are so common, many people don't seek medical help until the disease has progressed significantly. A diagnosis is typically confirmed through various tests such as pulmonary function tests, chest X-rays, CT scans, and sometimes a lung biopsy.
Understanding the Progression of IPF
The progression of IPF can be quite variable, with some people experiencing a slow decline over many years, while others may deteriorate more rapidly. It's important to understand that IPF is a progressive disease, which means that it tends to get worse over time. This can lead to an increased need for supplemental oxygen, and eventually, a lung transplant may be the only viable treatment option.
Managing the Early Stages of IPF
Although there is currently no cure for IPF, there are ways to manage the symptoms and slow the disease's progression in the early stages. Pulmonary rehabilitation, which includes exercises and education, can help improve lung function and quality of life. Certain medications may also be prescribed to slow the disease's progression and manage symptoms. It's also crucial for patients to quit smoking, maintain a healthy weight, and get regular exercise.
Navigating the Intermediate Stages of IPF
As the disease progresses into the intermediate stages, symptoms typically become more severe and more difficult to manage. At this point, the need for supplemental oxygen often becomes necessary. Many patients also begin to experience complications such as pulmonary hypertension, a condition characterized by high blood pressure in the arteries supplying the lungs. Despite these challenges, it's still possible to maintain a reasonable quality of life with the right treatment and support.
Coping with Advanced IPF
Once IPF reaches the advanced stages, it can significantly impact daily life. Breathing difficulties may become severe and patients may become increasingly reliant on oxygen therapy. At this stage, a lung transplant may be considered. This is a major surgery and not without risks, but for some, it can offer a chance for improved quality of life and extended survival.
Support for Patients and Families
Living with IPF can be incredibly challenging, not just for the patient, but for their loved ones as well. It's important that patients and families have access to the right support. This can include counseling, support groups, and palliative care services. Remember, it's not just about managing the physical symptoms of the disease, but also addressing the emotional and psychological impact.
Understanding the stages of Idiopathic Pulmonary Fibrosis is the first step towards effectively managing this condition. I hope this blog post has provided some valuable insight into this complex and challenging disease. Please remember that everyone's journey with IPF is unique, and what works for one person may not work for another. Always consult with a healthcare professional for personalized advice.



Chloe Ingham
July 12, 2023 AT 12:21They don't want us to know how quickly IPF can hijack your lungs, and the “early stage” hype is just a veil. The pharmaceutical companies push the rehab narrative while secret trials are hidden in basement labs. Every cough could be a silent alarm sent by the government to test the limits of public health surveillance. Look at the way oxygen tanks are suddenly everywhere – coincidence? The disease is a pawn in a larger game we’re too scared to name.
Mildred Farfán
July 24, 2023 AT 19:33Oh sure, “just quit smoking and do rehab” – as if it’s that simple, right? In reality, the guidelines I’ve seen actually stress a multidisciplinary approach, with pulmonary rehab, antifibrotic drugs, and close monitoring. If you need specifics, the ATS/ERS consensus provides clear dosage charts and follow‑up intervals. Happy to point you to those papers, but don’t expect a magic bullet.
Danielle Flemming
August 6, 2023 AT 02:45Wow, this breakdown is like a vivid roadmap through a foggy forest – absolutely brilliant! The way you described the transition from a dry cough to oxygen dependence really paints a picture. I love how you highlighted the emotional toll on families; it’s often the hidden scar. Keep sprinkling those colorful analogies, they make the science feel alive!
Anna Österlund
August 18, 2023 AT 09:57Listen up, folks – the middle stage isn’t a death sentence, it’s a call to arms! Ramp up your oxygen, claim your meds, and fight back with everything you’ve got.
Brian Lancaster-Mayzure
August 30, 2023 AT 17:09It’s worth noting that pulmonary rehabilitation isn’t just exercise; it also offers education on pacing and breathing techniques. Many patients report a measurable improvement in six‑minute walk distance after a few weeks. If you’re starting out, consider a program that includes a certified respiratory therapist.
Erynn Rhode
September 12, 2023 AT 00:21When discussing idiopathic pulmonary fibrosis, it is essential to maintain precise terminology, as the nuances can significantly affect patient understanding. Firstly, the term “idiopathic” denotes that the cause remains unknown, which distinguishes IPF from other interstitial lung diseases with identifiable etiologies. Secondly, the staging of the disease commonly references functional metrics such as forced vital capacity (FVC) and diffusing capacity for carbon monoxide (DLCO). Thirdly, early-stage IPF typically presents with a dry, nonproductive cough, a symptom that many clinicians mistake for a simple upper‑respiratory infection. Fourth, high‑resolution computed tomography (HRCT) often reveals a peripheral, reticular pattern that is characteristic yet not pathognomonic. Fifth, a lung biopsy, while invasive, may be necessary when imaging is equivocal, and its histopathological hallmarks include usual interstitial pneumonia (UIP) pattern. Sixth, the progression rate varies widely; some patients experience an annual decline in FVC of less than 5 %, whereas others lose more than 10 % within a year. Seventh, antifibrotic agents such as nintedanib and pirfenidone have been shown in randomized controlled trials to reduce the rate of decline in lung function. Eighth, these medications, however, are not without side effects, including gastrointestinal disturbances that may limit adherence. Ninth, supplemental oxygen therapy becomes indicated when resting arterial oxygen tension falls below 55 mm Hg or when exertional desaturation occurs. Tenth, the psychological impact of chronic breathlessness should not be underestimated, and referral to a mental‑health professional is advisable. Eleventh, pulmonary rehabilitation programs, which combine aerobic exercise, strength training, and education, have demonstrated improvements in quality‑of‑life scores. Twelfth, community support groups can provide invaluable peer insight, especially regarding navigating insurance coverage for high‑cost therapies. Thirteenth, lung transplantation remains the definitive therapeutic option for selected candidates, though eligibility criteria are stringent. Fourteenth, post‑transplant care includes lifelong immunosuppression, which introduces its own set of complications. Fifteenth, regular multidisciplinary team meetings ensure that treatment plans are continuously re‑evaluated in light of new evidence. Finally, staying informed through reputable sources such as the American Thoracic Society can empower patients to participate actively in their care.
Rhys Black
September 24, 2023 AT 07:33One must admit, the discourse surrounding IPF often devolves into a cacophony of half‑baked recommendations, as if the layperson were merely a vessel for profit‑driven hype. Yet, if we elevate our conversation to a scholarly plane, the literature reveals a sobering truth: fibrosis is a relentless architect of architectural decay within the alveoli. The moral imperative, then, is to demand rigorously peer‑reviewed interventions rather than succumb to the siren song of unproven modalities. In short, elevate the standards, lest we perpetuate a cycle of mediocrity.
Abhishek A Mishra
October 6, 2023 AT 14:45Hey guys, i was just wondering how much the oxygen tanks actually help in day to day life? From what i read, they can be a game changer but also kinda bulky. If anyone has tips on portable options, that would be awesome!
Jaylynn Bachant
October 18, 2023 AT 21:57Life, in its fragile breath, mirrors the fibrotic lung – a canvas slowly overlaid with unseen scars. We chase cures as if chasing shadows, yet perhaps the true healing lies in the acceptance of impermanence. Is the disease a teacher, urging us to contemplate the limits of control? Such questions, though unanswerable, stir the soul.
Anuj Ariyo
October 31, 2023 AT 04:09The progression of IPF is relentless, unpredictable, and demands constant vigilance; moreover, patients must adapt, seek support, and manage therapies; consequently, the journey is both challenging and uniquely personal.
Tom Lane
November 12, 2023 AT 11:21Great summary! Let’s keep the conversation going by sharing any new clinical trial results you hear about. Together we can stay ahead of the curve and support each other through every stage.