More than 1 in 5 older adults in the U.S. takes a medication that could be quietly shrinking their brain. It’s not something you’d expect from a pill for bladder control, allergies, or depression - but it’s real. These drugs are called anticholinergics, and while they work well for certain conditions, they come with serious, often overlooked side effects: memory loss, brain shrinkage, and constant dry mouth.
What Are Anticholinergics and Why Are They So Common?
Anticholinergics block acetylcholine, a brain chemical that helps with memory, attention, muscle control, and saliva production. They’ve been around since the early 1900s, originally pulled from deadly nightshade plants. Today, they’re used for everything from overactive bladder to Parkinson’s, motion sickness, and even insomnia.
Drugs like oxybutynin (for bladder control), diphenhydramine (Benadryl), amitriptyline (for depression and nerve pain), and trihexyphenidyl (for Parkinson’s) all fall into this category. What makes them dangerous isn’t just that they’re used - it’s how often they’re used long-term. A 2015 Harvard study found 20-30% of older adults were taking at least one medication with anticholinergic effects. Many don’t even realize they’re on one. A pill for allergies might be labeled Benadryl, but the active ingredient - diphenhydramine - is also in many sleep aids and cold medicines.
The Brain Shrinkage You Can’t See
It’s not just about forgetting where you put your keys. Long-term anticholinergic use is linked to measurable brain changes. Brain scans from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) showed people taking high-ACB (anticholinergic cognitive burden) drugs had 0.5-1.2% more brain shrinkage per year than those who didn’t. That might sound small, but over five years, that adds up to real tissue loss - especially in the hippocampus, the part of the brain responsible for forming new memories.
These drugs also reduce glucose metabolism in the brain by 8-14%, meaning brain cells aren’t getting the energy they need to function. Ventricles - fluid-filled spaces in the brain - were 10-15% larger in users, which is a classic sign of brain atrophy. In one study, 63% of older adults on high-ACB medications developed mild cognitive impairment or Alzheimer’s within 10 years, compared to 38% of non-users.
The effect is dose-dependent. Each extra point on the ACB scale (which rates drugs from 0 to 3) increases annual brain shrinkage by 0.3%. A drug with an ACB score of 3 - like scopolamine or oxybutynin - is far riskier than one with a score of 1, like glycopyrrolate or tolterodine.
Cognitive Test Results: How Bad Is It?
People on these drugs don’t just feel foggy - they perform worse on real cognitive tests. Studies show:
- 23-32% worse on immediate memory recall
- 18-27% worse on tasks requiring planning and problem-solving
- Up to 1.8 standard deviations lower in attention and working memory when using scopolamine
These aren’t subtle differences. They’re the kind of drop that makes someone forget a doctor’s appointment, miss a medication dose, or get lost in their own neighborhood. A 2020 study comparing oxybutynin to tolterodine found users of oxybutynin had 28% greater cognitive decline over time - even though both treat the same bladder condition.
Dry Mouth Isn’t Just Annoying - It’s a Warning Sign
If you’re constantly thirsty, chewing gum all day, or struggling to speak because your mouth feels like sandpaper, that’s not just a side effect - it’s a signal. Dry mouth happens because anticholinergics block the nerves that tell your salivary glands to produce saliva.
According to Drugs.com reviews, 82% of users report severe dry mouth. One person wrote: “I drink 3 liters of water a day and still feel parched.” Another said, “I can’t eat dry food without sipping water every bite.”
But dry mouth isn’t just uncomfortable - it’s dangerous. Less saliva means higher risk of cavities, gum disease, and swallowing problems. It can also make medications harder to take, leading to missed doses. And it’s a red flag: if your mouth is dry, your brain is likely being affected too.
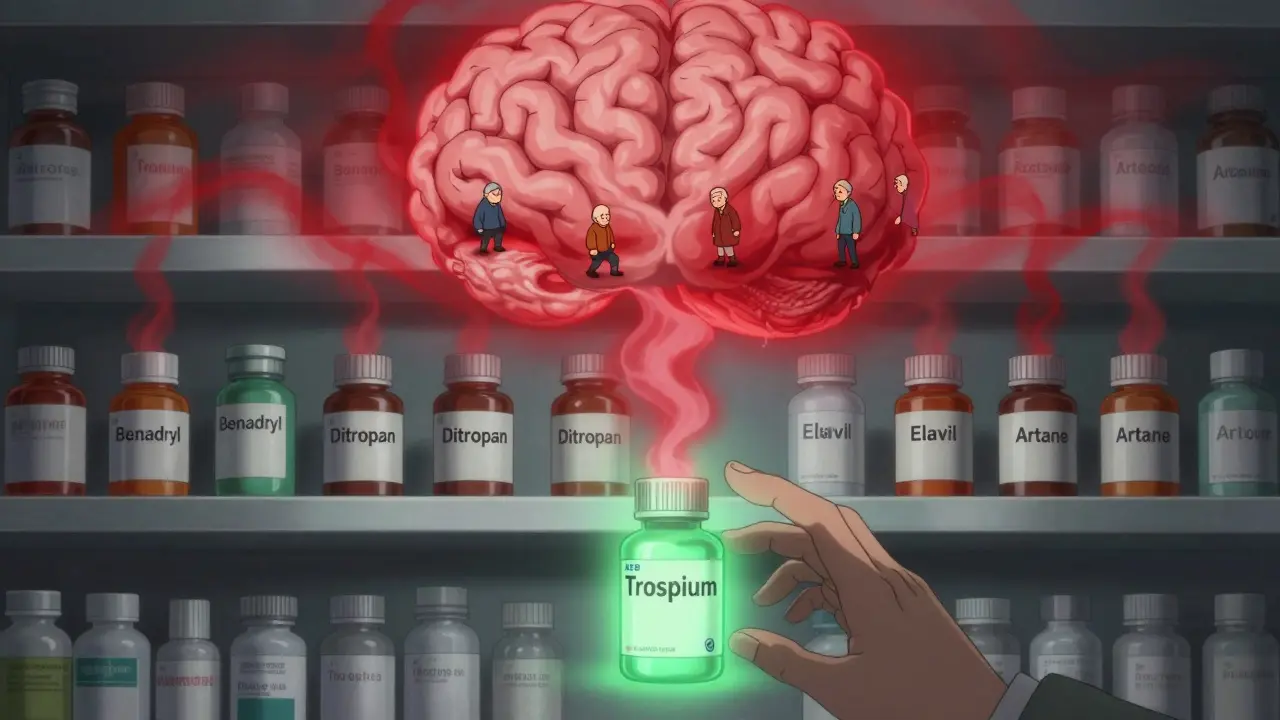
Not All Anticholinergics Are Created Equal
Here’s the crucial part: not every drug in this class is equally risky. The difference matters a lot.
High-risk (ACB 3): scopolamine, oxybutynin, diphenhydramine, amitriptyline, chlorpheniramine
Medium-risk (ACB 2): some older antidepressants, certain Parkinson’s drugs
Low-risk (ACB 1): glycopyrrolate, tolterodine, darifenacin, fesoterodine, trospium, tiotropium, ipratropium
Studies show that low-ACB drugs like trospium and glycopyrrolate cause little to no cognitive decline. In fact, a 2023 review found no significant memory loss with these agents. That’s why experts now say: if you need an anticholinergic, pick the lowest-risk option.
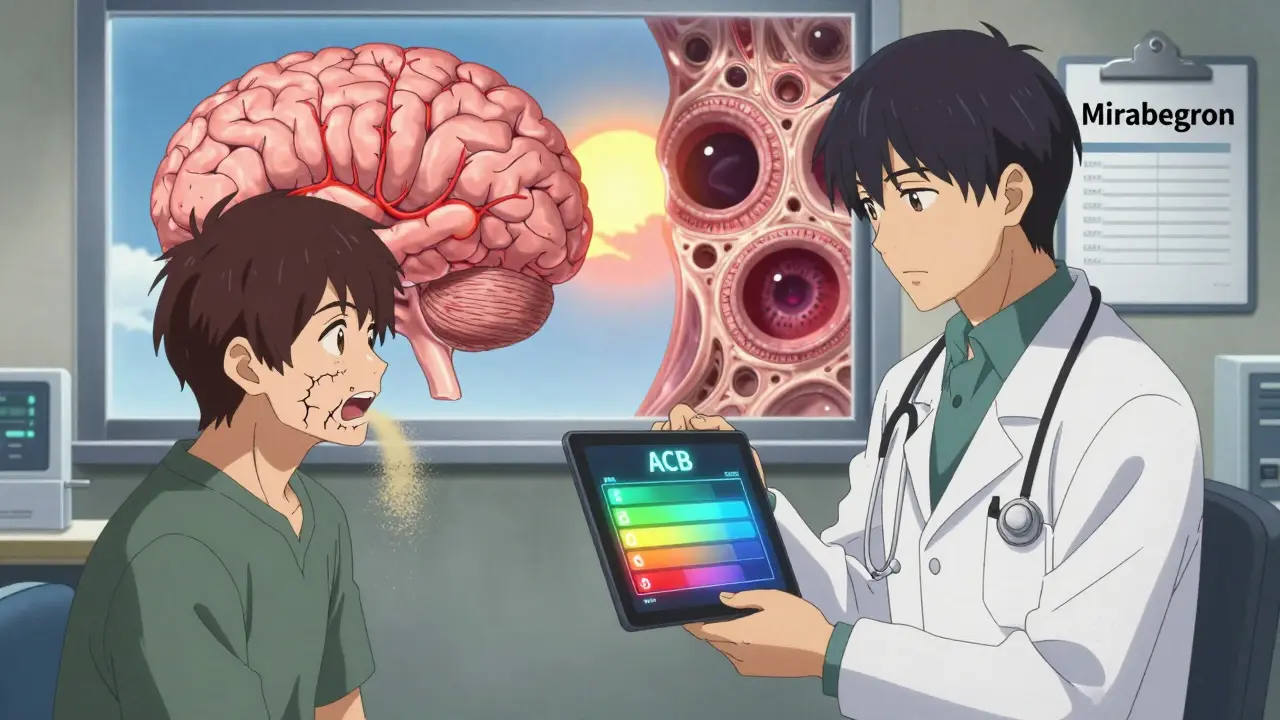
There Are Better Alternatives
For overactive bladder - one of the most common uses - mirabegron (a beta-3 agonist) works just as well as oxybutynin but has zero anticholinergic activity. A 2017 NEJM trial showed identical results in reducing bathroom trips, without the brain fog. The catch? Mirabegron costs about $350/month, while generic oxybutynin is $15. Many patients and doctors stick with the cheap option, unaware of the long-term cost.
For insomnia, melatonin or cognitive behavioral therapy (CBT-I) are safer than diphenhydramine. For depression, SSRIs like sertraline or escitalopram have minimal anticholinergic effects compared to amitriptyline. For Parkinson’s, levodopa remains the gold standard - anticholinergics are now only used when other treatments fail.
What Should You Do?
If you or a loved one is on one of these drugs, don’t stop suddenly. Abruptly quitting can cause rebound symptoms, especially with Parkinson’s or severe depression. Instead:
- Check the medication’s ACB score. Many online tools list them - search “ACB scale drug list.”
- Ask your doctor: Is this the lowest-risk option? Is there a non-anticholinergic alternative?
- For bladder issues: Try behavioral therapy (timed voiding, pelvic floor exercises) or mirabegron first.
- For sleep or allergies: Replace diphenhydramine with non-anticholinergic options.
- Get a baseline cognitive test (like the MoCA) and repeat it every 6-12 months.
For dry mouth, try sugar-free gum or lozenges (they boost saliva by 30-40%). Prescription options like pilocarpine (5mg 3x/day) can increase saliva flow by 50-70%. Saliva substitutes like Xerolube help too - though they cost $25-40/month.
Why Do Doctors Keep Prescribing Them?
A 2020 JAMA Internal Medicine study found only 32% of primary care doctors could correctly identify high-ACB drugs during a test. Many still think “Benadryl is safe for sleep” or “it’s just a bladder pill.” The FDA updated labels in 2022 to include stronger warnings, and the American Geriatrics Society now lists 56 anticholinergics as potentially inappropriate for seniors. But change is slow.
Prescription rates are falling - oxybutynin prescriptions dropped 32% from 2015 to 2022 - as mirabegron use rose. Still, millions of older adults are on these drugs with no idea of the risk.
The Future: Safer Drugs on the Horizon
New drugs are being designed to avoid these problems. Trospium chloride XR (Sanctura XR) has 70% less brain penetration than oxybutynin. Karuna Therapeutics’ xanomeline targets brain receptors more precisely, cutting dry mouth by 40% in trials. And AI tools like MedAware, recently cleared by the FDA, can flag risky prescriptions before they’re written - potentially preventing 200,000-300,000 dementia cases a year in the U.S. alone.
For now, the best defense is awareness. If you’re taking an anticholinergic, ask: Is this still necessary? Is there a safer option? And what’s my plan for monitoring my brain health?
Can anticholinergics cause dementia?
Long-term use of high-ACB anticholinergics (score 2-3) is linked to a doubled risk of dementia after three or more years of use, according to a 2015 BMJ study of over 48,000 patients. Brain imaging shows structural changes - like hippocampal shrinkage and enlarged ventricles - that are early signs of cognitive decline. While they don’t directly cause dementia, they significantly increase the risk, especially in older adults.
Which anticholinergic drugs are safest for the brain?
Drugs with an ACB score of 1 are considered safest. These include glycopyrrolate, tolterodine, darifenacin, fesoterodine, trospium, tiotropium, and ipratropium. Studies show these cause little to no cognitive decline, even with long-term use. For bladder issues, trospium and glycopyrrolate are preferred over oxybutynin or diphenhydramine.
How do I know if my medication is an anticholinergic?
Check the active ingredient, not just the brand name. Common anticholinergics include diphenhydramine (Benadryl), oxybutynin (Ditropan), amitriptyline (Elavil), tolterodine (Detrol), and trihexyphenidyl (Artane). Use the Anticholinergic Cognitive Burden (ACB) scale - a free online tool from the American Geriatrics Society - to look up your drug’s score. Scores of 2 or 3 indicate high risk.
Is dry mouth from anticholinergics reversible?
Yes - if you stop or switch the medication. Saliva production usually returns within days to weeks after discontinuation. In the meantime, sugar-free gum, prescription pilocarpine (5mg 3x/day), or saliva substitutes like Xerolube can help. But if dry mouth persists after stopping the drug, see a dentist or doctor - it could signal another issue like Sjögren’s syndrome or dehydration.
Can I stop taking anticholinergics on my own?
No - especially for Parkinson’s, depression, or severe bladder issues. Stopping suddenly can cause rebound symptoms like worsened tremors, increased incontinence, or severe withdrawal. Always work with your doctor to taper off safely. They can help you switch to a safer alternative or reduce the dose gradually while monitoring your symptoms.