When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. That’s not luck. It’s because of CGMP - Current Good Manufacturing Practices - enforced by the FDA. These rules aren’t suggestions. They’re the law. And for generic drugs, they’re just as strict as those for brand-name medications. The FDA doesn’t cut corners just because a drug is cheaper. If a generic drug doesn’t meet CGMP standards, it can’t be sold. Period.
What Exactly Is CGMP?
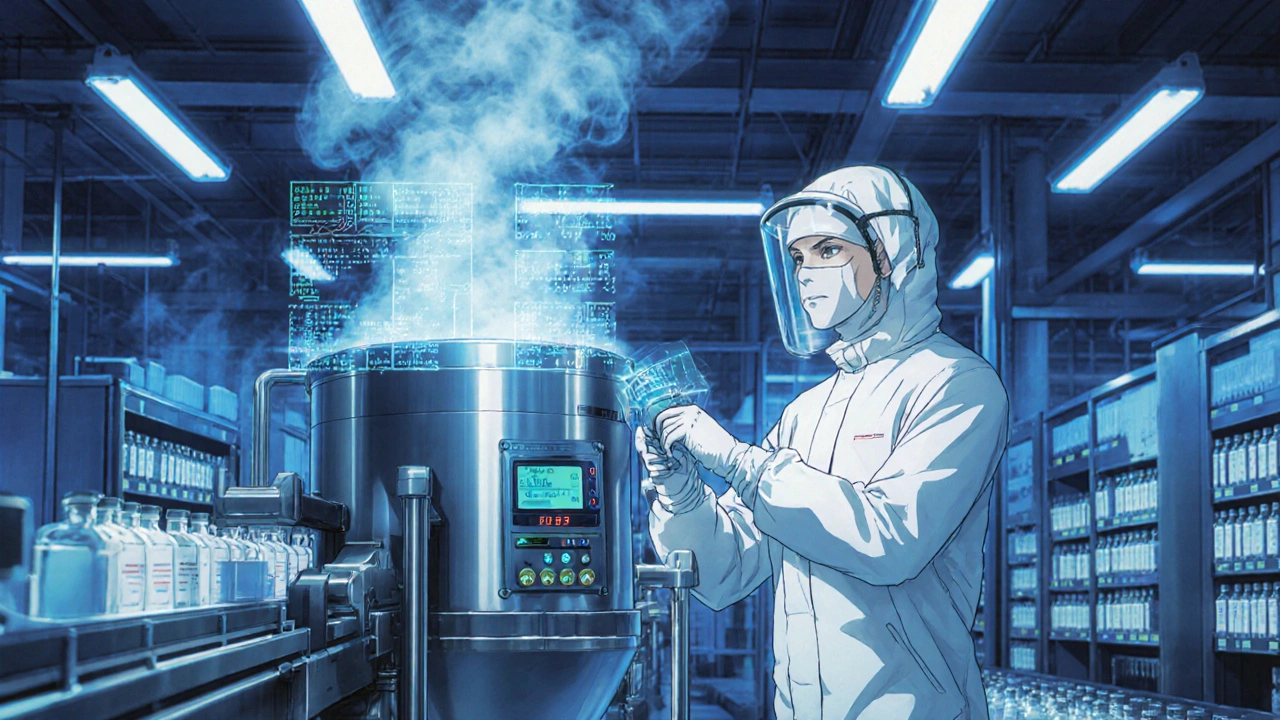
CGMP stands for Current Good Manufacturing Practices. It’s a set of rules written into U.S. law - specifically, 21 CFR Parts 210 and 211. These rules cover every step of making a drug: from the raw ingredients to the final pill in the bottle. The word "current" is key. It means manufacturers can’t rely on old methods. They have to use modern technology, up-to-date equipment, and proven processes. Outdated practices? Not allowed.
The FDA doesn’t just inspect factories once and call it done. They check continuously. Every generic drug application - called an ANDA (Abbreviated New Drug Application) - must prove the company follows CGMP. No compliance? No approval. No approval? No sale. This system keeps the U.S. generic drug market safe. In 2022, 90% of all prescriptions filled in the U.S. were for generics. That’s over 4 billion prescriptions. If even a small fraction of those were made under poor conditions, the public health impact would be huge.
The 11 Rules That Keep Generic Drugs Safe
CGMP isn’t one rule. It’s 11 detailed sections, each targeting a different part of manufacturing. Here’s what they actually require:
- Organization and Personnel (§211.25) - Everyone who touches the drug must be trained. Not just once.每年都得培训。They need to know how to handle materials, clean equipment, and document everything. No exceptions.
- Buildings and Facilities (§211.46) - Clean rooms, air filters, humidity controls. If you’re making pills, the air around them has to be cleaner than in a hospital operating room. Dust, mold, or even skin flakes can contaminate a batch.
- Equipment (§211.68) - Machines must be calibrated. Regularly. And records of every calibration, repair, and cleaning must be kept. A broken scale? Don’t use it. A dirty mixer? Clean it - and prove you did.
- Control of Components (§211.84) - Every batch of active ingredient, even something as simple as lactose, must be tested before use. No guessing. No "it looks fine." You need lab results.
- Production and Process Controls (§211.100-113) - You can’t just wing it. Every step of making the drug must be validated. That means you prove, with data, that your process always produces the same result. And you test during production - not just at the end.
- Packaging and Labeling (§211.122) - Labels must be verified. One wrong label could mean someone gets the wrong dose. Or worse - a drug meant for high blood pressure ends up in a child’s medicine bottle.
- Holding and Distribution (§211.142) - Temperature matters. Humidity matters. Light matters. If a drug needs to be stored at 2-8°C, you have to prove it never went above that. No "we think it was fine." You need logs.
- Laboratory Controls (§211.166) - Stability testing. You have to prove the drug doesn’t break down over time. Is it still potent after 2 years? You need data from real-time aging tests.
- Records and Reports (§211.180) - Every batch record, every test result, every training log - you keep them for at least one year after the drug expires. In some cases, longer. Paper or digital - doesn’t matter. But they must be complete, accurate, and tamper-proof.
- Returned and Salvaged Products (§211.206) - If a customer sends back a bottle, you don’t just toss it. You quarantine it. You investigate why it was returned. You don’t re-sell it unless you prove it’s still safe.
These aren’t vague guidelines. They’re exact, measurable requirements. And the FDA checks them - hard.
Why CGMP Is the Same for Generics and Brand Drugs
Some people think generics are "second-rate." That’s wrong. The FDA requires generics to be identical in strength, purity, and quality to the brand-name version. The only difference? The price. And the packaging. And the name on the bottle.
Pfizer, one of the biggest brand-name drugmakers, says it plainly: "Generics must be manufactured under the same strict standards of FDA’s good manufacturing practice regulations required for brand products." That’s not marketing speak. That’s policy. The FDA doesn’t care who made it. They care if it meets the standard.
That’s why a generic metformin tablet from India, a generic atorvastatin from Germany, and a brand-name Lipitor from New Jersey all have to pass the same tests. Same equipment standards. Same cleaning protocols. Same lab controls.
Where CGMP Gets Hard - and Where It Breaks
CGMP works - but it’s not easy. Small generic manufacturers struggle the most. A 2022 survey found 68% of companies had trouble with documentation. Writing down every step, every test, every decision - it’s time-consuming and expensive. One company on Reddit said switching to electronic batch records cost $1.2 million and took 14 months.
And then there’s data integrity. The FDA cares deeply about this. Are the numbers real? Were records altered? In 2022, 63% of all warning letters for data issues came from foreign facilities. Why? Because some manufacturers still use paper logs, or worse - backdate entries. The FDA now requires audit trails. Every change to a digital record must be tracked. No exceptions.
One of the biggest failures? The 2022 recall of 12 generic metformin products. Why? Inadequate cleaning of equipment. NDMA - a probable carcinogen - built up in the machines and got into the pills. The FDA blamed "failure to validate cleaning procedures." That’s a direct CGMP violation.
Even worse? The 2022 deaths in Pakistan linked to contaminated glycerin. The FDA responded with a new, immediately effective rule in May 2023: every batch of glycerin, propylene glycol, and similar ingredients must be tested for diethylene glycol and ethylene glycol - deadly contaminants. This wasn’t a suggestion. It was a mandate.
How Manufacturers Stay Compliant - and What’s Next
Big companies like Teva are investing in new tech. In 2021, they switched to continuous manufacturing for a cardiovascular generic. Instead of making drugs in batches, they run it like a factory line. Result? Batch failures dropped from 4.2% to 0.7%. And they stayed fully CGMP-compliant.
But most generic manufacturers still use batch production. Why? Because validating new tech under CGMP is slow and expensive. The FDA is trying to help. Their Emerging Technology Program is working on draft guidance for continuous manufacturing - expected in mid-2024.
Another big shift? AI and predictive quality. By 2028, McKinsey predicts 65% of manufacturers will use real-time data analytics to spot problems before they happen. Imagine a machine that tells you, "This batch is likely to fail because the humidity spiked last night." That’s the future. And it’s coming.
For now, the rules are clear: if you make a generic drug in the U.S. - or export it to the U.S. - you must follow CGMP. No shortcuts. No exceptions. The FDA doesn’t just inspect. They audit. They investigate. And they shut down facilities that don’t comply.
What Happens If You Fail?
Getting caught violating CGMP isn’t a fine. It’s a crisis.
- Warning letters - public. Posted on the FDA website. Damages your reputation.
- Import alerts - your drugs get blocked at the border.
- Consent decrees - courts force you to fix everything under supervision. Could take years.
- Product recalls - expensive. Dangerous. Loss of trust.
- Civil penalties - up to $1 million per violation.
Janet Woodcock, former head of FDA’s drug center, warned: "Non-compliance can result in a prohibition on the sale of an adulterated drug." Translation: you lose your business.
Final Reality Check
Generic drugs are safe because of CGMP. Not because manufacturers are nice. Not because consumers demand it. Because the law forces them to do it right.
It’s expensive. It’s complex. It’s exhausting. But it works. The U.S. has the lowest rate of counterfeit drugs in the world - not because of luck, but because of these rules.
If you’re a manufacturer: follow CGMP exactly. Don’t cut corners. Document everything. Train your people. Test your ingredients. Validate your processes. The FDA is watching.
If you’re a patient: trust your generic. It’s not a cheaper version. It’s the same drug - made under the same rules.
Are CGMP requirements different for generic and brand-name drugs?
No. The FDA requires generic and brand-name drugs to follow the exact same CGMP rules. The only difference is the name on the label and the price. Both must meet identical standards for identity, strength, purity, and quality.
What happens if a generic drug manufacturer violates CGMP?
The FDA can issue a warning letter, block imports, force a product recall, or even shut down the facility. Violations can lead to civil penalties of up to $1 million per offense. Companies may also face consent decrees requiring court-supervised fixes, which can take years and cost millions.
How often does the FDA inspect generic drug factories?
Domestic facilities are inspected about every 18 months on average, while foreign facilities get inspected less frequently - about once every 3-5 years. However, the FDA is increasing foreign inspections by 25% through 2027. High-risk facilities, like those with past violations, may be inspected annually.
Is CGMP the same in the U.S. as in Europe?
The U.S. FDA and European EMA share about 85% alignment in GMP standards. Both follow ICH guidelines. But the FDA is stricter on documentation, requires more frequent inspections, and enforces data integrity rules more aggressively. European companies exporting to the U.S. must still meet FDA’s specific requirements.
Why is data integrity such a big deal in CGMP?
Data integrity means the records are accurate, complete, and unaltered. If a lab changes a test result to make a batch look good, that’s fraud. The FDA uses ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, Available) to judge data quality. Violations here are the #1 reason for warning letters.
Can small companies afford CGMP compliance?
It’s tough. Mid-sized generic manufacturers spend an average of $2.3 million annually on CGMP compliance. For small firms, this can be 15-20% of total revenue. Many use electronic quality management systems (eQMS) to reduce costs over time. Some partner with third-party consultants, but hiring one can cost $250-$500 per hour. The barrier is high, but the FDA doesn’t offer exemptions.
What’s the biggest mistake generic manufacturers make?
Underestimating documentation. Many companies focus on making the drug right but skip writing down how they made it. The FDA doesn’t care what you think you did - they care what you wrote. Missing records, backdated entries, or unverified data are the top reasons for inspection failures.
Do CGMP rules apply to active pharmaceutical ingredients (APIs)?
Yes. APIs - the actual drug substance - must also follow CGMP. The FDA inspects API facilities separately. In 2022, 43% of generic manufacturers reported component testing failures, often because their API supplier didn’t meet standards. That’s why the FDA now requires full traceability from raw materials to finished product.
How long does it take to set up a CGMP-compliant facility?
From ground-up construction to first commercial batch, it typically takes 18-24 months. This includes facility qualification (IQ/OQ/PQ), process validation, staff training, and system audits. Rushing this process leads to compliance failures later. The FDA doesn’t approve shortcuts.
Will CGMP rules change in the next few years?
Yes. The FDA is pushing for real-time quality control using AI and advanced analytics. Expect stricter rules on data integrity, supply chain security, and continuous manufacturing. The Drug Supply Chain Security Act will also require more tracking of ingredients. By 2028, most manufacturers will need predictive quality systems to stay compliant.





Benjamin Gundermann
November 26, 2025 AT 11:19Man, I love how the FDA doesn't play games. I mean, you think generics are some cheap knockoff? Nah. They're the same damn pill, just without the fancy logo. And the fact that they inspect factories like they're checking for bombs? That's American efficiency right there. We don't cut corners because it's cheaper-we cut corners because we're lazy. And the FDA? They don't care if you're in India or Iowa. If it doesn't pass, it stays out. Period. 🇺🇸
Manish Pandya
November 26, 2025 AT 21:19As someone who works in pharma in India, I can say this: CGMP is not optional. We train our staff daily, audit every batch, and keep digital logs that even my grandma could read. It's expensive, yes-but imagine if a child got the wrong medicine because we skipped a test. No. We don't do that. The FDA isn't being harsh. They're being responsible.
Adesokan Ayodeji
November 28, 2025 AT 07:42Hey, I just want to say-this is one of those rare topics where the system actually works. 🙌 Yes, it's expensive. Yes, it's a headache. But think about it: 4 billion prescriptions a year, and almost none of them are dangerous? That’s not magic. That’s thousands of people showing up every day, wearing gloves, calibrating machines, logging temps, and refusing to cut corners. That’s the quiet heroism of manufacturing. We don’t cheer for them, but they’re the reason your diabetes meds don’t kill you. Keep doing the work, folks.
Karen Ryan
November 28, 2025 AT 22:55So… if my generic metformin is from India, and the FDA says it’s safe… does that mean I can trust it? 😅 I just want to know I’m not taking a gamble with my health. Also, thank you for explaining this so clearly. 🙏
Terry Bell
November 30, 2025 AT 13:24Man, I used to think generics were just… cheaper versions. Like, you know, the generic soda that tastes like the real thing but has less fizz. But this? This is like comparing a Walmart bike to a Trek-same wheels, same frame, same safety standards. Just no carbon fiber and a lower price tag. The FDA’s not being picky. They’re being smart. And honestly? I’m glad they are.
Lawrence Zawahri
November 30, 2025 AT 19:13YOU THINK THIS IS SAFE? LOL. The FDA’s got lobbyists in their pocket. That metformin recall? Total cover-up. NDMA? That’s from the Chinese labs-they’ve been poisoning our meds for DECADES. And they let it happen because they’re making billions off our prescriptions. You think they care if you live or die? Nah. They care about profit. They’re letting dangerous drugs in because they’re too lazy to inspect properly. Wake up, sheeple. 🚨
Rachelle Baxter
December 2, 2025 AT 10:17Let me just say-this is why I refuse to take anything that isn't made in the USA. 🇺🇸 I don't care if it's 'the same formula.' If it's not made under American oversight, with American workers, in American facilities, then it's a gamble. And I'm not gambling with my body. The FDA is doing their job, but foreign factories? They cut corners. Always. Always. Always. And you're paying for it with your health.
Dirk Bradley
December 2, 2025 AT 16:13It is imperative to underscore that the Current Good Manufacturing Practices, as codified under 21 CFR Parts 210 and 211, constitute a non-negotiable regulatory framework-enforced with unwavering rigor by the U.S. Food and Drug Administration. The notion that generic pharmaceuticals are somehow less stringent in their compliance is not only erroneous, but emblematic of a profound misunderstanding of pharmaceutical jurisprudence. The FDA’s enforcement posture is not merely bureaucratic-it is bioethical.
Emma Hanna
December 3, 2025 AT 03:43Wait-so you’re telling me that a company in India can make my blood pressure pill… and the FDA says it’s fine? But they don’t inspect every single factory every year?!! That’s insane. And what about the people who backdate logs? That’s fraud. And the FDA just… lets it happen? No. No. NO. This is a disaster waiting to happen. Someone’s going to die. And then we’ll all cry. But by then, it’ll be too late. 🙄
Mariam Kamish
December 4, 2025 AT 03:04Yeah, sure. 'Same standards.' But you know what? I’ve seen the price of my generic go up 300% in 2 years. Who’s really benefiting here? Not me. Not you. It’s the same old story: big pharma, big government, same players. 😒