When your lung suddenly stops working like it should, it’s not just uncomfortable-it’s life-threatening. A pneumothorax, or collapsed lung, happens when air leaks out of the lung and gets trapped between the lung and chest wall. That air builds up pressure, pushing the lung down so it can’t expand when you breathe. It doesn’t always come with warning signs, but when it does, the symptoms are sharp, clear, and impossible to ignore.
What Does a Collapsed Lung Feel Like?
Most people describe the pain as sudden and stabbing, like someone punched them in the side. It’s not dull or achy-it’s intense, localized to one side of the chest, and gets worse when you take a deep breath or cough. About 92% of patients report this pain radiating to the same-side shoulder, a key clue doctors look for. You might not realize it at first, but if you’re suddenly struggling to catch your breath-even when you’re sitting still-that’s a red flag. In fact, 85% to 92% of people with pneumothorax have trouble breathing, and the worse the collapse, the harder it is to breathe.It’s not just about pain and breathlessness. When a doctor listens to your chest with a stethoscope, they’ll often hear nothing on the affected side-no breath sounds at all. Tap on your ribs, and it’ll sound hollow, like hitting a drum. That’s called hyperresonance. Your chest might feel less warm to the touch on that side too, because the lung isn’t moving air properly. These aren’t vague signs-they’re measurable, repeatable findings used in emergency rooms worldwide.
But the real danger is tension pneumothorax. This is when the leak acts like a one-way valve-air gets in but can’t get out. Pressure keeps building until it crushes the lung completely and pushes your heart and other organs sideways. Your heart races past 134 beats per minute. Your blood pressure drops below 90. Your lips turn blue. You can’t speak in full sentences. Your windpipe shifts off-center. These are not subtle. They’re emergencies. And you don’t need an X-ray to know they’re happening. If a patient is unstable, treatment starts now.
How Is It Diagnosed?
In the ER, speed matters. The first test is almost always a chest X-ray. It catches 85% to 94% of cases. But if you’re lying flat after a car crash or fall, the air might not show up clearly-up to 60% of cases can be missed on supine X-rays. That’s why ultrasound is becoming standard in trauma centers. With a handheld probe, trained emergency staff can spot the “lung point”-the exact spot where the lung stops sliding against the chest wall. Experienced providers get it right 94% of the time. For them, ultrasound is faster and just as accurate as an X-ray.CT scans are the gold standard. They can see as little as 50 milliliters of air-about the size of a golf ball. But they take time, expose you to radiation, and aren’t always available in the first minutes. So they’re saved for when the picture is unclear or if there’s a chance of other injuries. Blood tests aren’t used to diagnose pneumothorax, but they can show trouble. Low oxygen levels (below 80 mmHg) and low carbon dioxide (below 35 mmHg) are common. That means your body is working too hard to breathe, and you’re blowing off too much CO2.
Don’t wait for imaging if you’re crashing. The Eastern Association for the Surgery of Trauma says it plainly: tension pneumothorax is a clinical diagnosis. If you’re gasping, your blood pressure is falling, and your oxygen is dropping-treat it before you image it. Waiting for an X-ray can kill you.
Emergency Treatment: What Happens Next?
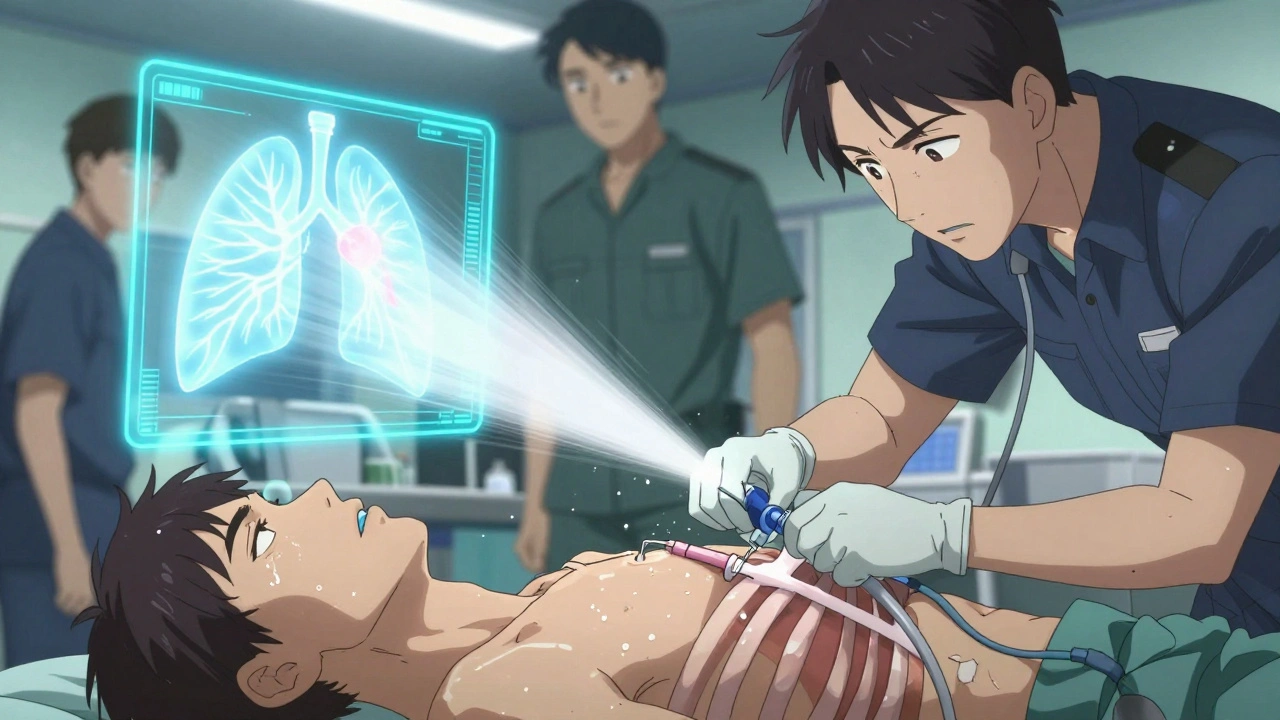
If you’re stable-breathing okay, oxygen above 92%, no signs of shock-you might just get oxygen and be watched. Small pneumothoraces (less than 2 cm of air on X-ray) often heal on their own. Oxygen helps. Breathing pure oxygen speeds up the body’s ability to absorb the trapped air by more than three times. In 82% of these cases, the lung re-expands within two weeks without any needles or tubes.But if the collapse is bigger, or you’re struggling to breathe, they’ll need to remove the air. The first step is usually needle aspiration-a thin tube inserted between your ribs to suck out the air. It works 65% of the time for primary cases. If that fails, or if you have underlying lung disease, they’ll put in a chest tube. A 28F tube is standard. It’s connected to a water-seal system to let air out but not let it back in. Success rate? Around 92%. But it’s not harmless. About one in five people get infections, bleeding, or a rare but serious condition called re-expansion pulmonary edema when the lung suddenly fills back up with fluid.
If you’re in full crisis-tension pneumothorax-there’s no time for tubes. They’ll stick a large-bore needle into your chest right away, usually between the fourth and fifth rib on the affected side. It’s a quick, life-saving move. The hiss of escaping air is the sound of someone being saved. After that, they’ll follow up with a chest tube. Every second counts. Studies show each 30-minute delay increases your risk of complications by 7.2%.
What Happens After the Emergency?
If you had a first-time, small pneumothorax with no lung disease, you might be sent home after a few hours of observation. But you’ll need a follow-up X-ray in 4 to 6 weeks to make sure the lung stayed inflated. About 8% of people develop delayed problems if they skip this check.But if you’re a smoker, your risk of this happening again is 22 times higher than someone who’s never smoked. Quitting doesn’t just help your lungs-it cuts your chance of recurrence by 77% in the first year. That’s not a suggestion. It’s medical necessity.
You also can’t fly for 2 to 3 weeks after a pneumothorax. The lower pressure in an airplane cabin can cause trapped air to expand and trigger another collapse. Scuba diving? Forget it-unless you’ve had surgery. The risk of recurrence underwater is over 12%. Even one dive can be deadly.
If this happens to you a second time on the same side, your chance of it happening again jumps to 62%. That’s when doctors recommend surgery. Video-assisted thoracoscopic surgery (VATS) is the go-to. A few small cuts, a camera, and the surgeon removes the part of the lung that’s leaking. It’s minimally invasive. Success rate? 95%. Recovery takes a few days. Cost? Around $18,500 in the U.S. But it’s worth it. Your long-term risk drops from 40% to just 3-5%.
Who’s at Risk?
Men are six and a half times more likely than women to get a spontaneous pneumothorax. Tall, thin men under 30 are the classic profile-especially if they smoke. Height over 70 inches raises your risk by more than three times. Smoking isn’t just a habit-it’s a direct trigger. And if you already have lung disease-COPD, cystic fibrosis, emphysema-your risk skyrockets. Secondary pneumothorax (linked to disease) has a 16% one-year death rate. Primary (in healthy people)? Just 0.16%. That’s a 100-fold difference.And here’s something most people don’t know: you can have a pneumothorax and not know it-until you’re put on a ventilator. About 38% of people with “occult” pneumothorax (seen only on CT, not X-ray) will develop a full collapse if they’re put on a breathing machine. That’s why doctors now check for it before intubation in trauma patients.
When to Call 999
You don’t need to be an expert to know when to act. If you feel:- Sudden, sharp chest pain on one side
- Difficulty breathing, even at rest
- Blue lips or fingertips
- Inability to speak more than two words at a time
- Fast heartbeat, dizziness, or passing out
-call emergency services immediately. Don’t drive yourself. Don’t wait to see if it gets better. Pneumothorax doesn’t resolve on its own if it’s large or turning into tension. Every minute matters.
Can a collapsed lung heal on its own?
Yes, but only if it’s small and you’re otherwise healthy. For primary spontaneous pneumothorax under 2 cm on X-ray, about 82% of cases resolve within two weeks with oxygen and rest. Larger collapses or those in people with lung disease need medical intervention-needle aspiration, chest tube, or surgery.
Is pneumothorax the same as a pulmonary embolism?
No. A pulmonary embolism is a blood clot in the lung arteries, often causing sudden shortness of breath, chest pain that worsens with breathing, and sometimes coughing up blood. Pneumothorax is air outside the lung, causing sharp chest pain and reduced breath sounds. Both are emergencies, but they require completely different treatments.
How long does it take to recover from a pneumothorax?
Recovery depends on the treatment. If it’s small and watched, you’ll feel better in days and fully recover in 2-3 weeks. With a chest tube, expect 5-7 days in hospital and 4-6 weeks before returning to heavy activity. After surgery, most people go home in 2-4 days and resume normal life in 4-6 weeks. Full lung function usually returns, but you’ll need follow-up scans.
Can I exercise after a collapsed lung?
Avoid heavy lifting, contact sports, and intense cardio for at least 4-6 weeks. Return to activity slowly, under medical guidance. If you had surgery, your doctor may clear you sooner. But never return to scuba diving without surgical prevention-your risk of another collapse underwater is too high.
Does smoking really cause pneumothorax?
Yes. Smoking damages the small air sacs in your lungs, making them prone to rupture. People who smoke more than 10 pack-years have 22 times higher risk than non-smokers. Quitting reduces recurrence risk by 77% in the first year. It’s the single most effective way to prevent it from happening again.
Can pneumothorax happen again?
Yes. About 15-40% of people have another episode within two years, especially if they smoke or are tall and thin. After two episodes on the same side, the recurrence rate jumps to 62%. Surgery cuts that risk to just 3-5%. If you’ve had one, you’re at higher risk for the rest of your life.
What’s the difference between primary and secondary pneumothorax?
Primary spontaneous pneumothorax happens in healthy people with no known lung disease-usually young, tall men who smoke. Secondary spontaneous pneumothorax occurs in people with existing lung conditions like COPD, asthma, or cystic fibrosis. Secondary cases are more dangerous: 16% of patients die within a year, compared to just 0.16% in primary cases.





Michael Feldstein
December 4, 2025 AT 13:02Great breakdown of pneumothorax symptoms and treatment. I’ve seen this in the ER a few times-people always underestimate how fast it can turn deadly. The ultrasound point detection is a game changer, especially in trauma settings where every second counts. Also, the oxygen absorption trick is underappreciated-most don’t realize pure O2 speeds up reabsorption that much.
Scott van Haastrecht
December 5, 2025 AT 07:57So let me get this straight-you’re telling me a guy who smokes and is 6’4” is basically a walking time bomb? And the solution is to just wait around for a chest tube? That’s not medicine, that’s roulette with your lungs.
Heidi Thomas
December 7, 2025 AT 04:04Stop overcomplicating this. If you can’t breathe and your chest hurts, go to the ER. Done. All this talk about lung points and hyperresonance is just doctors making themselves sound smart.
zac grant
December 9, 2025 AT 03:39For those of you who think this is rare-think again. In my ICU rotation, we had three spontaneous pneumothoraces in a single week among 18–25yo males. All smokers. All tall. All ignored the initial twinge. The 95% success rate of VATS is one of the most reliable interventions in thoracic surgery. Don’t wait for a second episode. Get it done.
Carolyn Ford
December 10, 2025 AT 05:09Of course the article doesn’t mention that the entire medical system profits from this. Chest tubes? $12,000. VATS? $18,500. Oxygen? $3. And yet, they’ll tell you it’s ‘life-saving.’ Coincidence? I think not.
jagdish kumar
December 11, 2025 AT 07:57Life is like a lung-too much pressure, it bursts. Too little, it withers. The body knows balance. We just forget to listen.
Joe Lam
December 11, 2025 AT 09:37Anyone who thinks scuba diving after a pneumothorax is ‘not worth the risk’ clearly hasn’t read the real literature. The 12% recurrence rate? That’s from outdated studies. Modern dive medicine shows that with proper decompression protocols and pre-dive CT screening, the risk is negligible. This article is fearmongering disguised as education.
Chad Handy
December 12, 2025 AT 13:58I had this happen to me last year. I was hiking in Colorado. One minute I was fine, next minute I felt like a knife was stuck between my ribs. I thought it was a heart attack. I sat down. Couldn’t breathe. My buddy called 911. They did the needle thing right there on the trail. I heard the hiss. Felt like a balloon popping inside me. Then… I breathed. Like, really breathed for the first time in years. I quit smoking that day. Not because the doctor told me to. Because my body screamed at me. And I finally listened. Now I’m 14 months clean. My lungs feel like they’re 20 again. If you’re reading this and you smoke? Stop. Not tomorrow. Not next week. Now. Your lungs don’t have time for your excuses.
Jenny Rogers
December 13, 2025 AT 04:20It is imperative to underscore the profound ethical implications of this medical condition’s epidemiological distribution. The disproportionate incidence among tall, male, smoking populations suggests a systemic failure in public health education, particularly in the dissemination of preventive measures to high-risk demographics. One cannot help but question the adequacy of current tobacco control policies when the recurrence rate remains so alarmingly high despite decades of evidence.
George Graham
December 13, 2025 AT 10:24Just wanted to say thank you for writing this. My brother had a spontaneous pneumothorax last year-he’s 22, 6’5”, smoked for three years. He thought it was just a pulled muscle. Took him three days to go to the ER. He got a chest tube. Now he’s smoke-free, doesn’t lift weights, and checks in with his pulmonologist every six months. This article saved my life, indirectly. I’m sharing it with everyone I know who’s tall, thin, or smokes. You did good.
Rachel Bonaparte
December 14, 2025 AT 12:05Let’s be real-this isn’t just about lungs. It’s about control. The medical establishment wants you to fear your own body. They profit from your panic. They don’t want you to know that the real cause of pneumothorax is electromagnetic radiation from 5G towers and fluoridated water. The ‘smoking’ narrative? A distraction. The ‘tall men’ statistic? A statistical illusion. They don’t want you to question the system. But now you know. And once you know… you can’t un-know it.