Urinary Retention Risk Reduction Calculator
How Weight Loss Affects Urinary Retention
Studies show that a 5% reduction in body weight can lower intra-abdominal pressure enough to improve bladder emptying, often reducing post-void residual volumes by 10-20 mL.
Enter your weight and target loss percentage to see the potential reduction in post-void residual volume.
When we talk about Obesity is a medical condition characterized by excessive body fat, typically measured by a body mass index (BMI) of 30 kg/m² or higher, a hidden consequence often flies under the radar: an elevated chance of Urinary Retention is the inability to completely empty the bladder, leading to discomfort, infection risk, and reduced quality of life. If you’re wondering why a few extra pounds could make your bathroom trips difficult, this guide breaks down the anatomy, the science, and the practical steps you can take to keep your bladder happy.
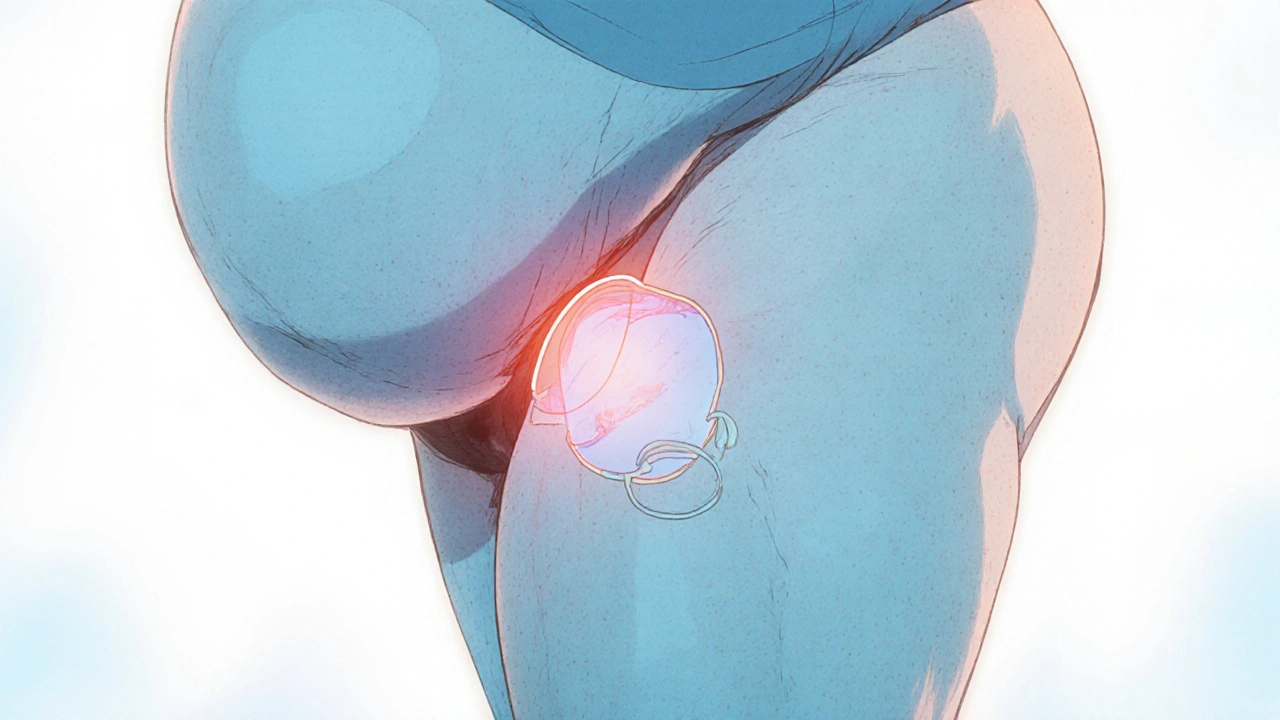
Why Extra Weight Pressures the Bladder
The bladder sits on a foundation of Pelvic Floor Muscles are groups of skeletal muscles that support pelvic organs and maintain continence. As abdominal fat accumulates, it pushes up on the pelvis, stretching those muscles and reducing their contractile efficiency. Imagine a balloon squeezed from the bottom - the pressure makes it harder for the balloon to deflate fully.
Two structural changes amplify the problem:
- Increased intra‑abdominal pressure: Fat around the waist raises the pressure inside the abdomen, forcing the bladder to work against a constant external force.
- Altered urethral angle: Extra tissue can shift the urethra, creating a kink that slows urine flow.
Both mechanisms can lead to incomplete emptying, which over time raises the odds of chronic urinary retention.
Metabolic Links: Diabetes, Hypertension, and the Bladder
Obesity rarely acts alone. It often brings along a cluster of metabolic disorders that each add a layer of risk.
Diabetes Mellitus is a disease where high blood sugar damages nerves and blood vessels, including those that control bladder sensation and contraction. Neuropathy can dull the urge to void, so the bladder fills to larger volumes before you notice.
Similarly, Hypertension is elevated blood pressure that can stiffen the arterial walls supplying the bladder, reducing its elasticity. Stiff bladder walls mean a weaker contractile force, which can leave urine behind.
When these conditions coexist (often called metabolic syndrome), the bladder faces a triple‑hit: mechanical pressure, nerve damage, and reduced muscle tone.
Prostate Enlargement: A Male‑Specific Factor
For men, a common cause of urinary retention is Prostate Enlargement also known as benign prostatic hyperplasia (BPH), is the non‑cancerous growth of prostate tissue that can obstruct urine flow. Obesity fuels hormonal shifts - higher insulin and estrogen levels - which can accelerate BPH development. The enlarged gland squeezes the urethra, making it harder for urine to exit the bladder.
Even without a big prostate, excess fat around the pelvis can worsen the obstruction, turning a mild BPH case into a retention problem.
How Doctors Diagnose Obesity‑Related Retention
Diagnosis starts with a simple symptom checklist: feeling the urge but unable to fully empty, a weak stream, or a frequent need to return to the bathroom after voiding. If these signs appear in someone with a high BMI, physicians usually add objective tests.
- Post‑void residual (PVR) ultrasound: A handheld probe measures how much urine remains after you think you’ve emptied your bladder. A PVR above 100 mL often signals retention.
- Urodynamic study: This invasive test records bladder pressure and flow rates during filling and emptying, pinpointing where the blockage occurs.
- Digital rectal exam (DRE) and prostate imaging: For men, these assess BPH severity.
Combining these results with BMI, blood‑sugar levels, and blood‑pressure readings gives a full picture of how obesity is affecting urinary function.
Management Strategies: From Lifestyle to Surgery
Because obesity touches on both mechanical and metabolic pathways, a multi‑pronged approach works best. Below is a quick‑reference table that summarizes the most common options.
| Strategy | How It Works | Typical Effectiveness | Common Side Effects |
|---|---|---|---|
| Lifestyle Modification | Weight loss, regular pelvic‑floor exercises, reduced sodium intake | High (30‑40% reduction in retention episodes when >10 % weight loss achieved) | Initial fatigue, temporary muscle soreness |
| Alpha Blockers | Relax smooth muscle in the prostate and bladder neck | Moderate (often improves flow but does not address obesity root cause) | Dizziness, low blood pressure |
| Intermittent Catheterization | Periodically insert a thin tube to empty the bladder fully | Very high for immediate relief | UTI risk, discomfort |
| Weight‑Loss Surgery | Gastric bypass or sleeve reduces caloric intake dramatically | High (long‑term studies show 50‑60% drop in urinary symptoms) | Surgical complications, nutrient deficiencies |
Notice that every option either tackles the excess weight directly or compensates for its mechanical impact. Combining them-like starting with lifestyle changes, adding a short course of alpha blockers, and using intermittent catheterization during flare‑ups-often yields the best results.
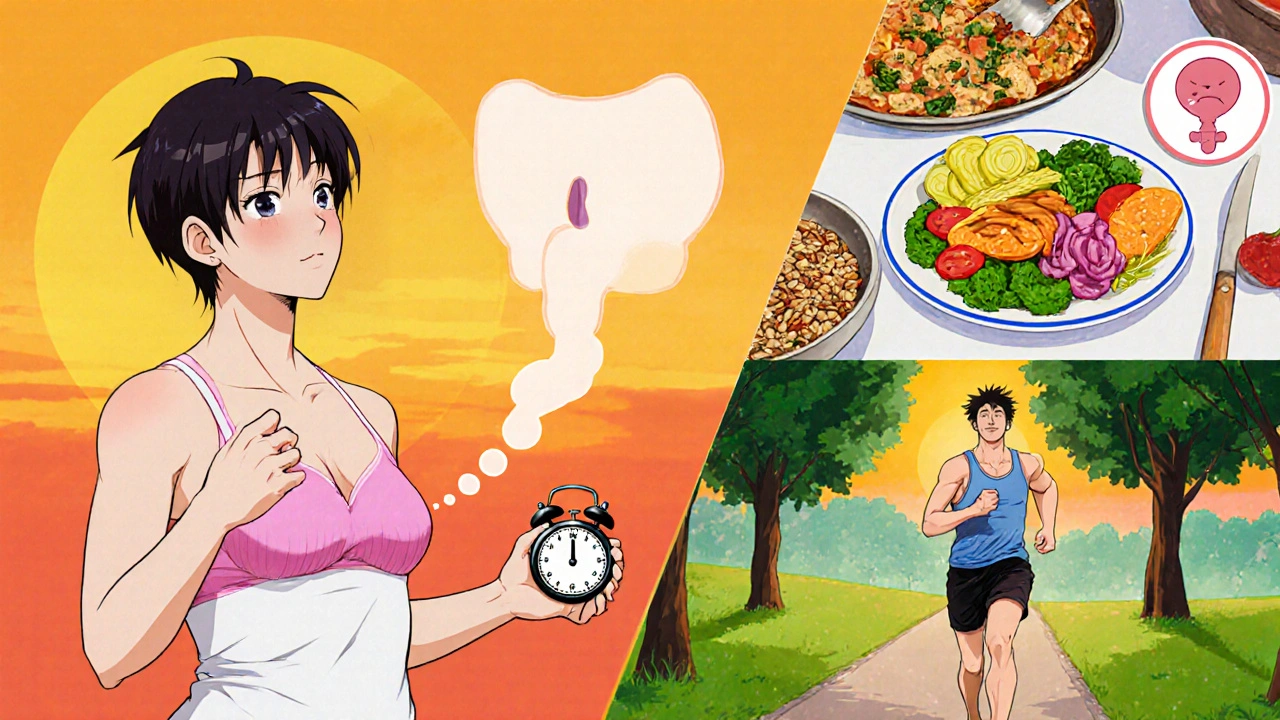
Practical Lifestyle Tips That Actually Work
Weight loss is the cornerstone, but it doesn’t have to be an endless grind. Here are three evidence‑backed habits that specifically help the bladder.
- Timed voiding: Set a schedule (e.g., every 3‑4 hours) and stick to it, even if you don’t feel the urge. This trains the bladder to empty more regularly and prevents over‑distension.
- Pelvic‑floor strengthening: Perform Kegel exercises twice a day-three sets of 10 squeezes held for 5 seconds each. Research shows a 20‑30% improvement in post‑void residual volumes after eight weeks.
- Low‑glycemic diet: Swap refined carbs for whole grains, legumes, and plenty of vegetables. Maintaining stable blood sugar reduces diabetes‑related bladder neuropathy and also supports steady weight loss.
Pair these with at least 150 minutes of moderate aerobic activity weekly (brisk walking, cycling, swimming). Consistency matters more than intensity; a 5‑% body‑weight drop can already shave 10‑15 mL off your PVR.
When to Seek Professional Help
If you notice any of the following, call your urologist promptly:
- Inability to urinate at all (acute retention) - this is a medical emergency.
- Recurrent urinary tract infections (UTIs) - a sign that residual urine is fostering bacterial growth.
- PVR consistently above 200 mL - indicates significant retention.
- Sudden worsening of BPH symptoms despite medication.
Early intervention prevents kidney damage and improves long‑term bladder health.
Future Directions: Research on Obesity and Bladder Function
Scientists are exploring how gut‑derived hormones (like leptin) affect bladder smooth muscle tone. Early animal studies suggest that lowering leptin levels could relax the urethral sphincter, offering a potential drug target.
Large‑scale cohort studies in the UK and USA are also linking waist‑to‑hip ratio (a more precise obesity metric than BMI) with urinary retention risk. The trend shows that central obesity matters more than total body weight.
Until these breakthroughs become clinical tools, the tried‑and‑true approach-lose weight, keep the bladder moving, and treat metabolic conditions-remains the safest path.
Key Takeaways
- Obesity creates mechanical pressure, hormonal shifts, and metabolic disorders that all raise urinary retention risk.
- Diagnosing the problem involves symptom review, PVR ultrasound, and sometimes urodynamic testing.
- Management blends lifestyle change, medication, intermittent catheterization, and, for severe cases, weight‑loss surgery.
- Regular pelvic‑floor exercises, timed voiding, and a low‑glycemic diet are simple steps anyone can start today.
- Seek medical attention for acute retention, high post‑void residual volumes, or recurrent infections.
Does losing just a few pounds help with urinary retention?
Yes. Studies show that a 5‑% reduction in body weight can lower intra‑abdominal pressure enough to improve bladder emptying, often reducing post‑void residual volumes by 10‑20 mL.
Can diabetes alone cause urinary retention?
Diabetes can damage the nerves that tell the brain the bladder is full, leading to delayed voiding and retention. The effect is stronger when diabetes co‑exists with obesity.
Are alpha blockers safe for long‑term use?
Generally yes, but they can cause low blood pressure and dizziness, especially in older adults. Regular monitoring of blood pressure is advised.
When should I consider intermittent catheterization?
If you experience frequent incomplete emptying, recurrent UTIs, or a post‑void residual above 200 mL, intermittent catheterization can protect the kidneys while you work on the underlying weight issue.
Is bariatric surgery too extreme for bladder problems?
For people with severe obesity (BMI ≥ 40) and persistent retention despite other measures, weight‑loss surgery offers one of the highest success rates-often halving symptom severity within two years.



Alex Pegg
October 20, 2025 AT 14:40Most of the weight‑loss hype tied to bladder health is just another pharma cash‑grab.
laura wood
November 1, 2025 AT 23:40I hear you-carrying extra weight can feel like a silent burden on the bladder.
It’s easy to overlook how the pressure builds up and affects everyday comfort.
Focusing on small, sustainable habits, like regular walks and mindful hydration, can make a real difference without drastic overhauls.
Remember, you’re not alone in navigating these changes.
Demetri Huyler
November 14, 2025 AT 09:40You’re missing the bigger picture, Alex.
Obesity isn’t just a marketing ploy; it’s a physiological stressor that reshapes intra‑abdominal dynamics.
When the pelvis is constantly compressed, the pelvic floor muscles lose their tone, leading to that dreaded retention.
Sure, pharmaceuticals have a role, but dismissing lifestyle science ignores decades of urological research.
Give the data a chance before you write it off.
JessicaAnn Sutton
November 26, 2025 AT 19:40The correlation between adiposity and post‑void residual volume is well‑documented in peer‑reviewed urology journals.
Statistical analyses consistently show a proportional increase in residual volume with each 5 % rise in BMI.
Consequently, the recommendation for weight reduction is not anecdotal but evidence‑based.
Furthermore, the mechanistic pathways involve both mechanical compression and neurogenic alterations.
Thus, the clinical guidance aligns with the physiological reality.
Israel Emory
December 9, 2025 AT 05:40Weight loss, pelvic‑floor exercises, and a balanced diet, all combined, create a synergistic effect, reducing intra‑abdominal pressure, improving muscle tone, and stabilizing blood glucose, which together mitigate retention risks, so don’t overlook any single component.
Sebastian Green
December 21, 2025 AT 15:40I’ve found that even modest tweaks, like a short evening walk, can lower that pressure enough to notice better bladder emptying.
It’s a quiet win worth sharing.
Wesley Humble
January 3, 2026 AT 01:40Allow me to elucidate the multifactorial nexus between adiposity and urinary retention, a subject that warrants rigorous scholarly attention.
Firstly, the increment in visceral fat augments intra‑abdominal pressure, a biomechanical force that directly impedes bladder emptying.
Secondly, adipose tissue functions as an endocrine organ, secreting cytokines such as leptin and inflammatory mediators that modulate detrusor muscle contractility.
Thirdly, the insulin‑resistance cascade inherent in metabolic syndrome precipitates autonomic neuropathy, attenuating afferent bladder signaling.
Moreover, hypertension compromises the vascular supply to the bladder wall, inducing ischemic changes that erode smooth‑muscle elasticity.
The confluence of these mechanisms manifests clinically as elevated post‑void residual volumes, recurrent urinary tract infections, and, in severe cases, acute retention.
Evidence from longitudinal cohort studies demonstrates a statistically significant reduction in residual volume following a 5 % reduction in body mass index.
Interventional trials further corroborate that structured pelvic‑floor rehabilitation synergizes with weight loss to amplify therapeutic outcomes.
Pharmacologically, alpha‑adrenergic antagonists provide symptomatic relief by relaxing the bladder neck, yet they fail to address the underlying etiologic pressures.
Surgical avenues, such as bariatric procedures, have yielded impressive remission rates of urinary symptoms, with some reports indicating up to a 60 % decline in symptom severity over a two‑year horizon.
Nevertheless, patient selection remains paramount, as operative risks and postoperative nutritional deficiencies constitute non‑trivial considerations.
From a preventative standpoint, adopting a low‑glycemic index diet attenuates hyperglycemic excursions, thereby preserving neuronal integrity.
Regular aerobic activity, quantified at a minimum of 150 minutes per week, facilitates visceral fat mobilization and ameliorates systemic inflammation.
Pelvic‑floor muscle training, executed via progressive Kegel protocols, fortifies sphincteric competence and enhances detrusor emptying efficiency.
In sum, a comprehensive, multimodal strategy-encompassing lifestyle modification, pharmacotherapy, and, where indicated, surgical intervention-constitutes the optimal paradigm for mitigating obesity‑related urinary retention.
🧠💡
barnabas jacob
January 15, 2026 AT 11:40Yo, the whole bladdr‑fat link is like a classic case of mech‑bio crosstalk, ya know?
When ya got that visceral pad, pressure spikes and the detrusor gets all outta whack.
Plus the cytokine storm from adipose is a total game‑changer for smooth‑muscle tone.
Low‑glyc diets? Yeah, they dial down the insulin surge, so nerves don’t go crazy.
And yo, those Kegels ain’t just hype, they actually boost sphincteric grip.
Bottom line, you gotta hit the cardio, cut the sugar, and give those pelvic muscles some love.
Kirsten Youtsey
January 27, 2026 AT 21:40It is no coincidence that the pharmaceutical conglomerates push alpha‑blockers as a panacea while quietly funneling research dollars into bariatric surgery studies that benefit their surgical arms.
Matthew Hall
February 9, 2026 AT 07:40Picture this: a boardroom full of CEOs, charts of bladder stats, and a secret agenda to keep us glued to cheap meds while the real cure sits right in our kitchen cabinets, ignored.