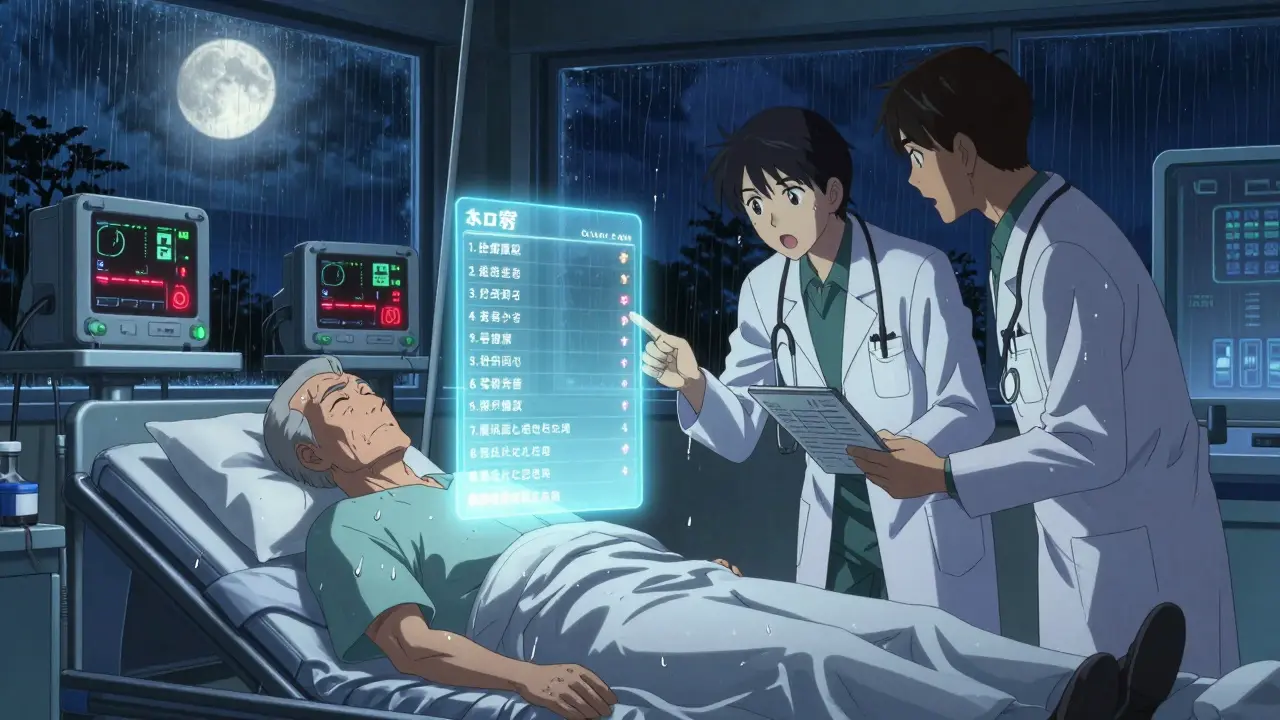
Every year, thousands of older adults end up in the emergency room because they took two pills that did the same thing-without knowing it. It’s not a mistake they made on purpose. It’s a system gap. A cardiologist prescribes metoprolol for high blood pressure. A month later, the primary care doctor prescribes another beta-blocker, unaware the first one was already filled. The patient feels dizzy. Their heart rate drops too low. They end up in the hospital. This isn’t rare. It’s common. And it’s preventable.
Why Duplicate Medications Happen
Specialists focus on one part of your health. A neurologist looks at your tremors. A rheumatologist treats your arthritis. A cardiologist manages your heart rhythm. But none of them see the full picture. They don’t know what your primary care doctor prescribed last week. They don’t know about the over-the-counter painkiller you’ve been taking for years. And they rarely check your pharmacy history unless you tell them.This is called therapeutic duplication. It happens when two or more drugs from the same class are prescribed for the same condition. For example:
- Two different ACE inhibitors for high blood pressure
- Two NSAIDs like ibuprofen and naproxen for joint pain
- Two SSRIs for depression
- Two blood thinners like warfarin and aspirin
Each of these combinations can lead to serious side effects: low blood pressure, kidney damage, internal bleeding, or even a stroke. The risk goes up with every extra pill you take. According to the Journal of the American Medical Informatics Association, pharmacists see about 20 duplicate medication alerts for every 100 prescriptions filled. And in nearly one in five of those cases, the duplication was dangerous.
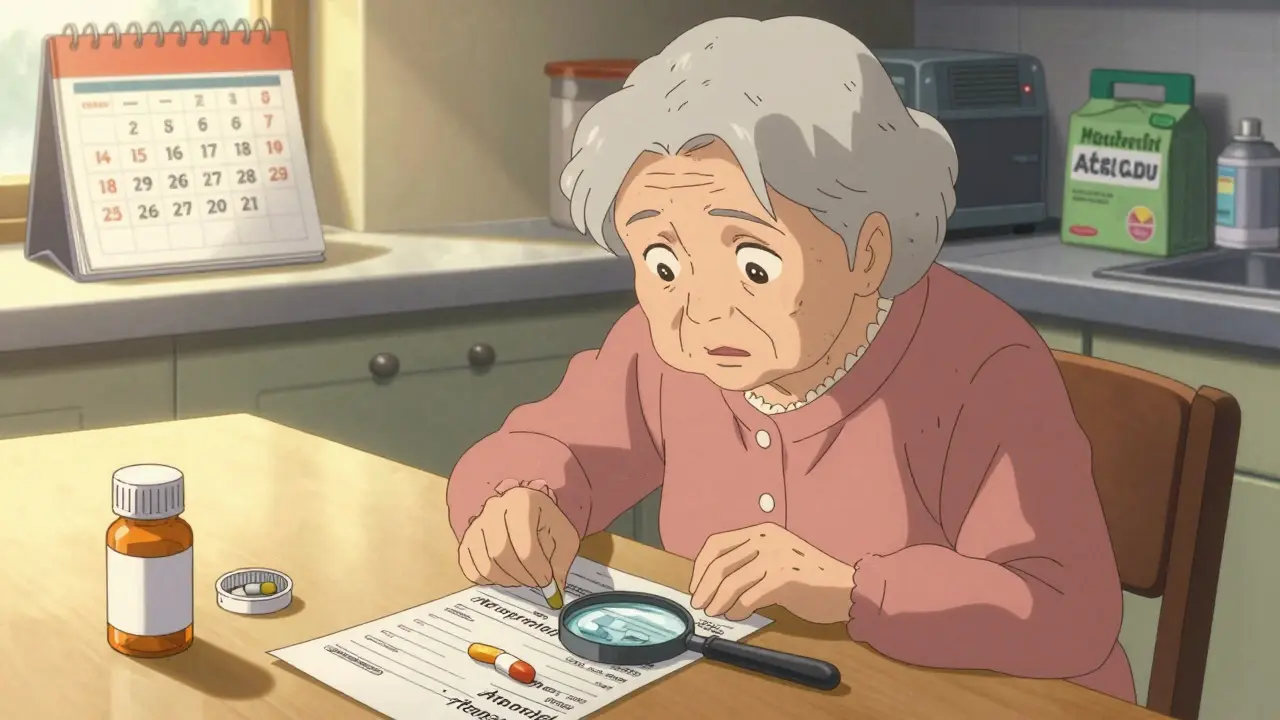
How to Spot Duplicate Medications Yourself
You don’t need to be a doctor to catch this. You just need to know what’s in your medicine cabinet.Start by making a complete list of everything you take. Not just prescriptions. Include:
- Over-the-counter pain relievers
- Antacids and stomach meds
- Vitamins and minerals
- Herbal supplements like St. John’s wort or ginkgo
- Eye drops, creams, and patches
Write down the name, dose, and why you take it. Example: “Lisinopril 10 mg daily for high blood pressure.” Don’t guess. If you’re not sure, bring your pill bottles to your next appointment. Pharmacists say this is the single most effective step patients can take.
Now, look for red flags:
- Two pills with similar-sounding names (e.g., simvastatin and atorvastatin)
- Two drugs with the same purpose (e.g., two different antihistamines for allergies)
- Prescriptions from different doctors that seem to treat the same symptom
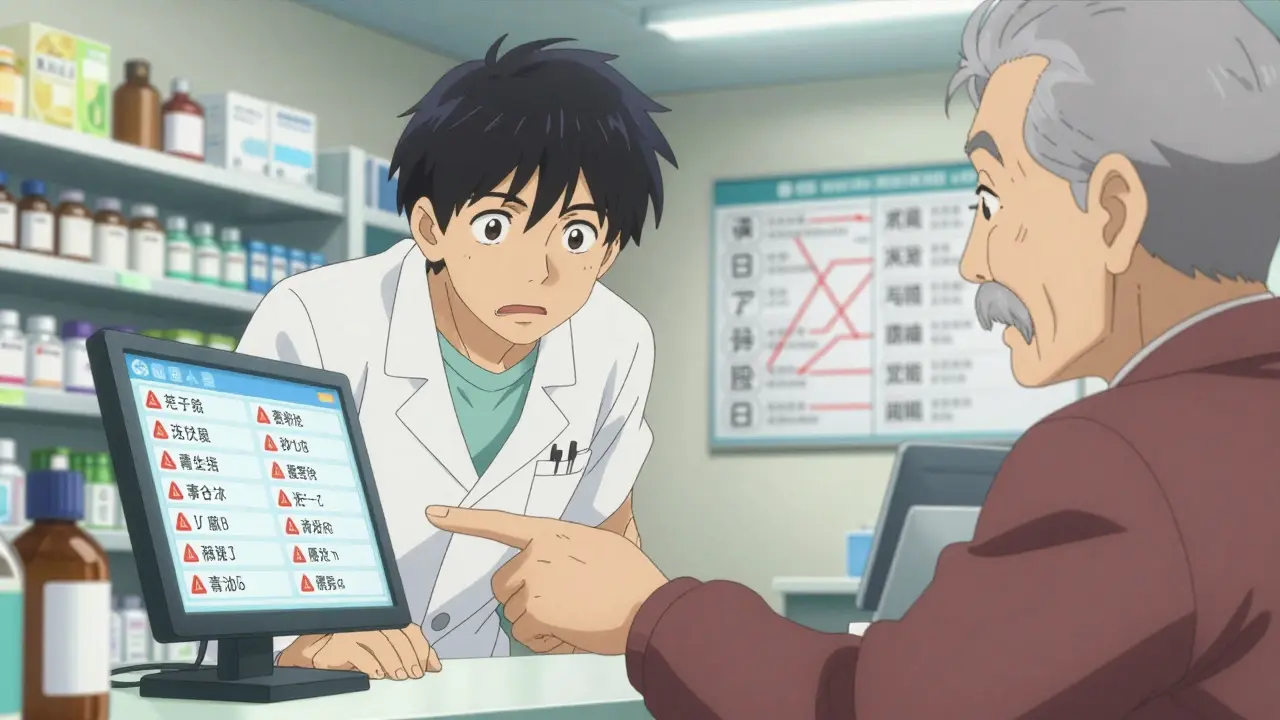
If you see something that looks repeated, ask your pharmacist. They’re trained to catch this. In fact, 68% of pharmacists report spotting a duplicate medication at least once a week.
Use One Pharmacy Only
This is one of the simplest, most powerful things you can do. If you use multiple pharmacies, your medication history gets split up. One pharmacy sees your heart meds. Another sees your diabetes pills. Neither sees the full list. That’s how duplicates slip through.Stick to one pharmacy. Even if it’s a bit farther away. The pharmacist there will build a complete record of everything you’ve filled over the years. They’ll see when you get a new prescription for the same type of drug and flag it before you even take it.
Some pharmacies even offer free medication reviews. Ask for one every six months. They’ll go through your list with you, check for overlaps, and call your doctors if something doesn’t add up.
Ask the Right Questions at Every Visit
Don’t assume your doctor knows your full list. Even if you gave them a paper list last time, things change. New prescriptions come in. Old ones get stopped. You might have started a new supplement.At every appointment-whether it’s with your primary care doctor or a specialist-ask these three questions:
- “Why am I taking this medication?” If you can’t explain the reason, you shouldn’t be taking it.
- “Is this new drug replacing something I’m already on?” Sometimes doctors add a new pill without stopping the old one.
- “Do I still need all of these?” Especially if you’ve seen multiple specialists, some meds may no longer be needed.
Doctors are busy. But they’ll respect you for being informed. And if they don’t, it’s a sign you need to find someone who will.
Get Your Medication List Updated After Every Change
Every time a new prescription is added-or an old one stopped-update your list. Don’t wait until your next appointment. Do it the same day.Keep a physical copy in your wallet. Save a digital copy on your phone. Share it with your main caregiver. If you’re hospitalized, give it to the nurse before they start any new meds.
Some people use apps like MyTherapy or Medisafe to scan pill bottles and track everything automatically. Others use a simple Google Doc. The tool doesn’t matter. What matters is that it’s current and accessible.
Don’t Let Alerts Be Overridden
Pharmacies and electronic health records have systems that warn doctors and pharmacists about possible duplicates. But those alerts aren’t foolproof. In fact, studies show that providers override them up to 32% of the time.Why? Because they’re overwhelmed. They’re rushed. Or they think the patient “must know what they’re doing.” But you’re not the one who should be catching this.
When you pick up a new prescription, ask the pharmacist: “Did your system flag anything about my other meds?” If they say no, say: “Can you double-check? I’m on several medications and want to make sure nothing’s duplicated.”
Most pharmacists will happily do it. They’re trained for this. And if they say they can’t, ask to speak with the pharmacy manager. This is a patient safety issue-not a convenience.
What to Do If You’ve Already Taken Duplicate Medications
If you realize you’ve been taking two drugs that do the same thing, don’t stop either one on your own. That can be just as dangerous.Call your primary care doctor right away. Bring your updated medication list. Say: “I think I might be taking two medications that do the same thing. Can we review them together?”
They may decide to:
- Stop one of the drugs
- Switch you to a different class of medication
- Adjust the dose to avoid side effects
Some people worry their doctor will be upset. But the truth? Doctors are relieved when patients catch these errors. It means they’re working as a team.
Technology Is Helping-But You Still Need to Be Involved
New tools are emerging. Mayo Clinic is testing AI systems that scan patient records and catch duplicate prescriptions with 143% more accuracy than before. Kaiser Permanente reduced duplicate prescriptions by 37% by requiring doctors to write the reason for each drug on the prescription.But none of these systems work unless you’re part of the loop. AI can’t know about the ginkgo supplement you started last month. An electronic record can’t tell if you stopped taking a pill because it made you sick. Only you know those details.
Technology helps. But your awareness saves your life.
Final Checklist: Your Action Plan
Here’s what to do today:- Make a full list of every medication, supplement, and OTC drug you take. Include doses and reasons.
- Bring your pill bottles to your next doctor visit-even if you think you already gave them your list.
- Use one pharmacy for all your prescriptions.
- Ask your pharmacist to review your list every six months.
- Ask your doctor at every visit: “Is this new drug replacing something?”
- Update your list the same day you start or stop any medication.
- Share your list with your main caregiver or family member.
Medication safety isn’t about trusting the system. It’s about being part of it. You’re not just a patient. You’re the most important link in the chain.






Bryan Woods
December 28, 2025 AT 07:57It’s staggering how often this happens-especially with older patients who see multiple specialists. I’ve seen it in my own family. One doctor prescribes a new med, another doesn’t know it’s already been filled, and suddenly someone’s on two beta-blockers. The system isn’t broken; it’s just fragmented. We need better communication, not just more alerts.
It’s not just about pills. It’s about trust. Patients need to feel empowered to ask, not just comply.
Ryan Cheng
December 28, 2025 AT 12:01One pharmacy. That’s it. That’s the whole game.
My grandma switched to CVS after juggling three different pharmacies for years. Within a month, they caught a duplicate statin and a hidden NSAID she was taking for back pain. She didn’t even know she was doubling up. Pharmacist flagged it before she left the counter. Simple. Effective. Why isn’t this mandatory?
wendy parrales fong
December 28, 2025 AT 20:45I love how this post doesn’t blame anyone. It just shows how the pieces don’t fit-and how we can fix it. I used to think doctors knew everything. Turns out, they’re just humans with too many patients and too little time.
Now I keep a little notebook in my purse. Every time I get a new script, I write it down. My daughter helps me update it on my phone. We don’t need fancy apps. We just need to remember we’re the ones holding the map.
And yeah, asking questions feels weird at first. But once you do it, it feels like you’re finally being heard.
Jeanette Jeffrey
December 30, 2025 AT 19:46Oh please. Another ‘just ask your doctor’ pep talk. Like that’s gonna fix a broken system. Doctors don’t care. Pharmacies are overworked. And patients? They’re too tired, confused, or scared to speak up.
Meanwhile, Big Pharma keeps pushing new drugs with overlapping effects because they’re profitable. You think they want you to ‘catch duplicates’? Nah. They want you to keep buying.
This isn’t about awareness. It’s about power. And you’re not gonna fix it with a Google Doc.
Shreyash Gupta
December 31, 2025 AT 13:16lol i use 3 pharmacies because one has better prices on my insulin 😅
but also my aunt died from a drug combo like this 💔
why do we even have ehr if they can’t talk to each other 🤡
also i take ashwagandha now is that a problem? 🤔
Ellie Stretshberry
January 2, 2026 AT 11:28i never thought about over the counter stuff being dangerous like that
my mom takes ibuprofen every day for her knees and then got prescribed naproxen and didn’t even realize they were the same kind of thing
she just trusted the doctor
now i help her keep a list on her phone
it’s not perfect but it’s better than nothing
Angela Spagnolo
January 3, 2026 AT 21:31…I’ve been doing this for years…
…every time…
…they look at me like I’m being difficult…
…but I’m not asking for special treatment…
…I’m asking them not to kill me…
…I have a list…
…printed…
…in triplicate…
…in my purse…
…on my fridge…
…on my tablet…
…and still…
…someone…
…always…
…misses…
…something…
david jackson
January 3, 2026 AT 23:02Let’s be real here-this isn’t just about medication duplication. This is about the entire healthcare system being designed like a Rube Goldberg machine built by someone who hates patients.
Specialists operate in silos like they’re playing a game of medical monopoly where each one owns a property and refuses to trade. The primary care doctor? They’re the guy who gets stuck with the ‘Go to Jail’ card every time. Meanwhile, the patient is the pawn who gets tossed between them like a hot potato.
And don’t get me started on the electronic health records. They’re supposed to be the hero of this story, right? Nope. They’re the guy who shows up late to the party, forgets half the guests’ names, and then blames everyone else for the chaos.
AI tools? Great. But they can’t read between the lines of a 78-year-old woman who says, ‘I take that green pill for my heart… and that blue one… I think it’s for the same thing?’
Only the patient knows that. Only the patient remembers that the doctor said ‘stop the blue one’ three months ago… but she didn’t throw it away because ‘maybe I’ll need it again.’
And let’s not forget the supplements. Ginkgo. St. John’s Wort. Turmeric. People think ‘natural’ means ‘safe.’ No. Natural doesn’t mean ‘non-interacting.’ It just means ‘not regulated.’
So yes-use one pharmacy. Make a list. Ask questions. But also… demand better systems. Because no amount of personal vigilance should be required to keep someone from dying because two doctors didn’t talk.
And if your doctor rolls their eyes when you bring a list? Find a new one. Your life isn’t a suggestion box.
Jody Kennedy
January 4, 2026 AT 02:51This is the kind of post that makes me want to hug every pharmacist in America.
They’re the unsung heroes who catch these mistakes while you’re distracted by your phone or your anxiety.
I used to think ‘pharmacist’ meant ‘person who hands you pills.’ Now I know they’re the last line of defense.
And if you’re reading this and you’re scared to ask questions? Just say this: ‘I don’t want to end up in the ER because someone forgot to check my meds.’
Trust me-it works.
And if they don’t take you seriously? That’s not your problem. That’s theirs.
Joanne Smith
January 5, 2026 AT 14:42Oh wow. So the solution to a multi-billion-dollar healthcare failure… is to make patients into unpaid pharmacists?
Brilliant.
Let’s just add ‘medication detective’ to the list of unpaid labor we expect from seniors: grocery shopping, tech support, family therapist, and now, drug-interaction auditor.
Meanwhile, the system that created this mess? Still collecting co-pays like nothing’s wrong.
At least the author had the decency to say ‘you’re the most important link.’
Too bad no one’s paying you for that link.
Prasanthi Kontemukkala
January 6, 2026 AT 08:27I’ve been a caregiver for my mother for five years now, and this post hits home in ways I can’t even explain.
She’s 82. Takes 14 meds. Uses three pharmacies. Doesn’t remember half of what she’s on.
We started keeping a color-coded list-green for heart, blue for blood pressure, red for pain. We printed it, laminated it, put it on the fridge.
And then we asked the pharmacist for a free review. He spent 45 minutes with us. Found two duplicates. Called her cardiologist. Changed one prescription.
She hasn’t felt this clear-headed in years.
It’s not about being perfect. It’s about being consistent.
You don’t need to be a doctor. You just need to care enough to write it down.
And if you’re reading this and thinking ‘I don’t have time’-you already do. Just one extra minute a day.
That’s all it takes to save a life.
Zina Constantin
January 7, 2026 AT 03:26As someone who grew up in a country where you get one doctor and one pharmacy and everyone knows your name-this feels both shocking and heartbreaking.
In my village, the pharmacist knew my grandmother’s meds better than her doctor did. He knew when she stopped taking her diuretic because she didn’t like the side effects. He knew when her daughter moved away and she forgot to refill.
Here? You’re a number. A barcode. A claim.
But you’re still human.
So carry your list. Speak up. Use one pharmacy. And if someone tells you ‘it’s not your job’-smile and say, ‘Then whose job is it?’
Because if it’s not yours… it’s mine.
And I don’t want to lose anyone else to a pill I didn’t know existed.
Bryan Woods
January 9, 2026 AT 01:06That’s the thing no one says out loud: this isn’t just about pills. It’s about dignity.
When you’re old, you’re told to be quiet. To trust the experts. To not ‘bother’ them.
But asking questions? That’s not being a burden. That’s being human.
I’ve seen too many people die quietly because they were too polite to speak up.
Don’t be polite. Be alive.