Multiple System Atrophy (MSA) isn’t just another form of Parkinson’s disease. It’s a far more aggressive, less predictable, and far deadlier condition that steals movement, balance, and even the body’s ability to regulate basic functions like blood pressure and bladder control. While it shares some symptoms with Parkinson’s - slow movement, stiffness, tremors - the differences are not subtle. They’re life-altering. And the prognosis? It’s grim.
What Makes MSA-P Different from Parkinson’s?
MSA comes in two main forms: MSA-P (parkinsonian) and MSA-C (cerebellar). MSA-P makes up about two-thirds of all cases. At first glance, it looks like Parkinson’s: stiff muscles, trouble starting to walk, a soft or shaky voice. But the similarities end there.
In Parkinson’s, tremors usually happen when you’re resting - like when your hand shakes while sitting still. In MSA-P, tremors are jerky and appear mostly when you’re trying to hold your arm out or move it. The stiffness doesn’t improve much with movement. And unlike Parkinson’s, where levodopa can bring back mobility for years, MSA-P barely responds to it. Only 15 to 30% of patients get any real benefit, and even then, it fades within a year or two.
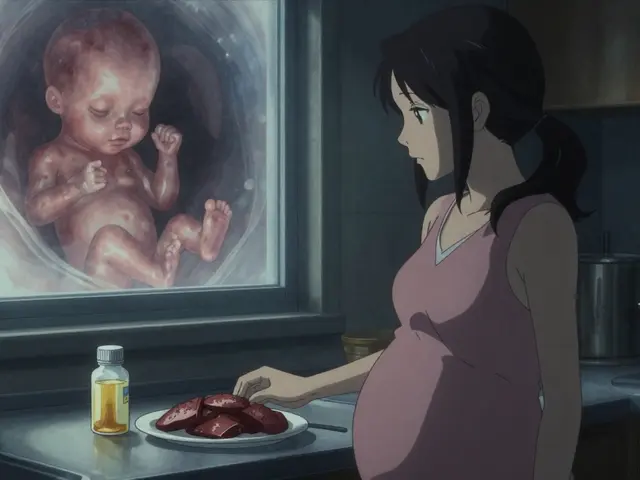
What really sets MSA-P apart is how early and how badly the autonomic nervous system fails. This is the part of your brain that controls things you don’t think about - heart rate, digestion, blood pressure, bladder function. In MSA-P, these systems start breaking down before motor symptoms even show up. Some men develop erectile dysfunction five years before they start stumbling or speaking softly. Others pass out when they stand up because their blood pressure crashes. That’s not normal aging. That’s MSA.
The Silent Collapse of Autonomic Function
Imagine waking up every morning with your body refusing to do the basics. You stand up - and everything goes dark. Your vision blurs. You feel like you’re falling, even if you’re not. That’s orthostatic hypotension, and it affects 90% of people with MSA-P. Blood pressure drops so fast, your brain doesn’t get enough oxygen. Fainting isn’t rare - it’s expected.
Then there’s the bladder. Eighty-five to ninety percent of patients lose control. Urgency. Incontinence. Nighttime accidents. It’s not just inconvenient - it’s isolating. Many stop going out. They stop seeing friends. The shame is real.
Sleep is another battlefield. Eighty to ninety percent of people with MSA-P act out their dreams. They kick, punch, yell in their sleep. Sometimes they fall out of bed. And half of them also have sleep apnea - stopping breathing dozens of times a night. No one sleeps well. No one feels rested.
Temperature control? Gone. Some lose the ability to sweat on their legs while still sweating on their face. They get too hot or too cold without warning. And swallowing? By the time it becomes a problem, it’s already dangerous. Food or saliva can slip into the lungs, causing pneumonia - the leading cause of death in MSA.
How Fast Does It Progress?
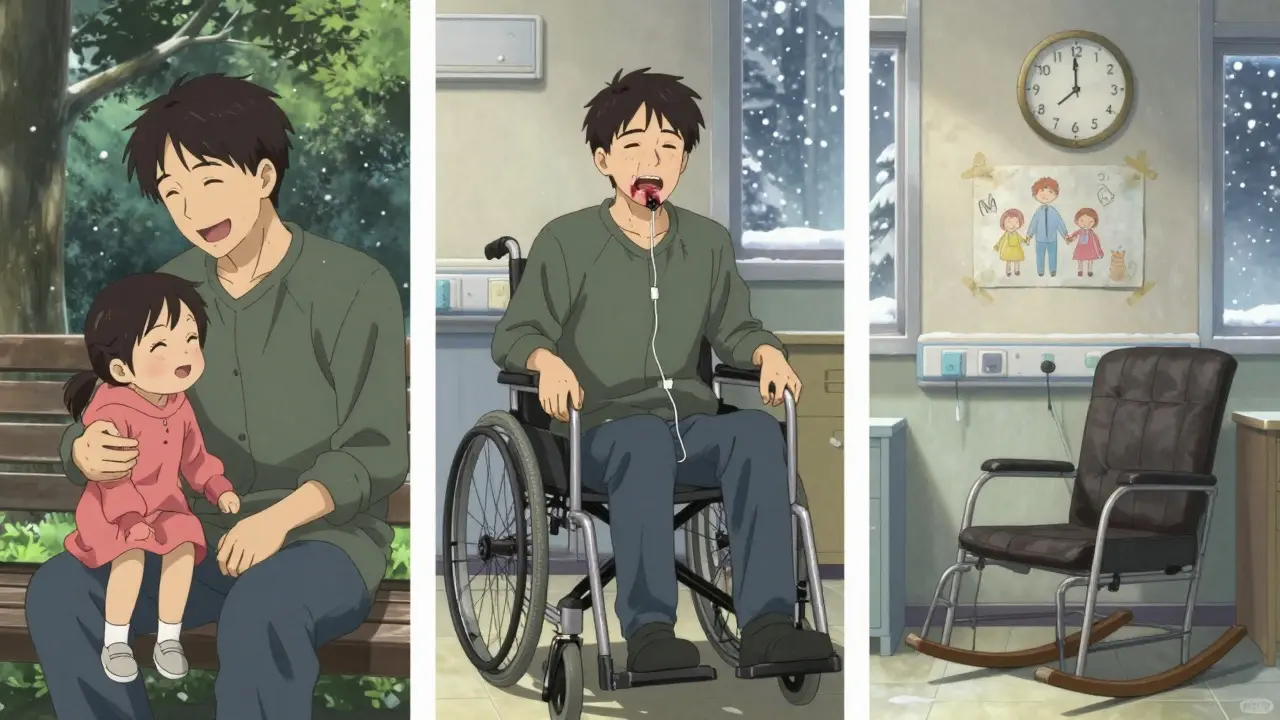
MSA doesn’t wait. It doesn’t give you time to adjust. Most people are diagnosed in their early 50s. Within 18 months, many need a cane. By three years, a walker. By four, a wheelchair. The median time to needing a wheelchair? Just over five years. Five years from when the first symptom appeared.
Within five years, half of all MSA-P patients have lost most of their motor function. They can’t stand without help. They can’t feed themselves. They can’t speak clearly. The progression is faster than almost any other neurodegenerative disease.
Life expectancy? Median survival is 6 to 10 years from symptom onset. That means half of people with MSA-P are gone within a decade. The 5-year survival rate? Just over 50%. By 10 years, only 9 to 23% are still alive. Compare that to Parkinson’s, where many live 15 to 20 years after diagnosis.
And the causes of death? Respiratory infections make up 45% - often from choking or aspiration. Sudden cardiac death? 20%. Swallowing problems leading to pneumonia? Another 15%. These aren’t complications. They’re inevitable outcomes.
Why Is Diagnosis So Hard?
Doctors often mistake MSA-P for Parkinson’s - especially in the first year. The symptoms overlap too much. Even neurologists can’t tell the difference until the autonomic symptoms become severe. That’s why diagnostic accuracy only reaches 85 to 90% after 3 to 5 years.
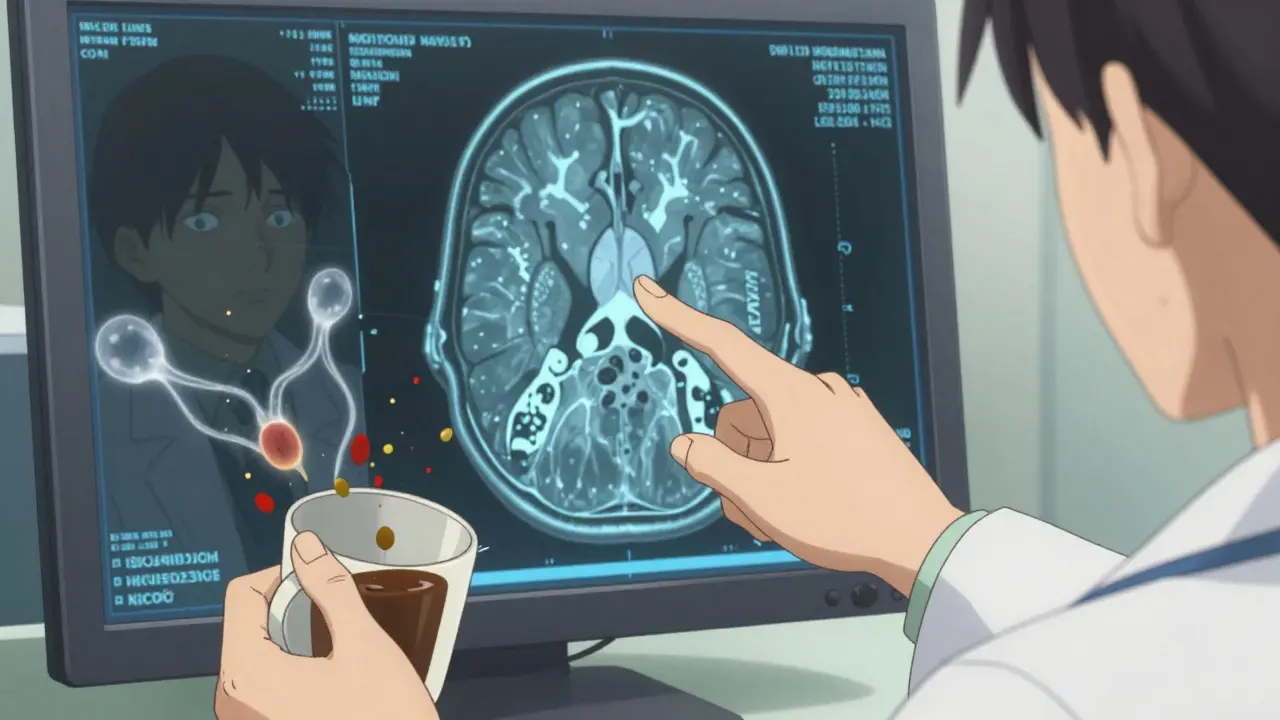
There are clues. The hot cross bun sign on an MRI - a cross-shaped pattern in the brainstem - appears in up to 80% of MSA-C cases and sometimes in MSA-P. Putaminal shrinkage on MRI is another red flag. Blood tests for neurofilament light chain - a protein released when brain cells die - are elevated three to five times higher in MSA than in Parkinson’s. These aren’t perfect, but they’re getting better.
The biggest clue? Autonomic failure within three years of motor symptoms. That’s the hallmark. If you’re 55, starting to shuffle your feet, and your blood pressure crashes when you stand up - it’s not Parkinson’s. It’s MSA.
What Treatments Are Available?
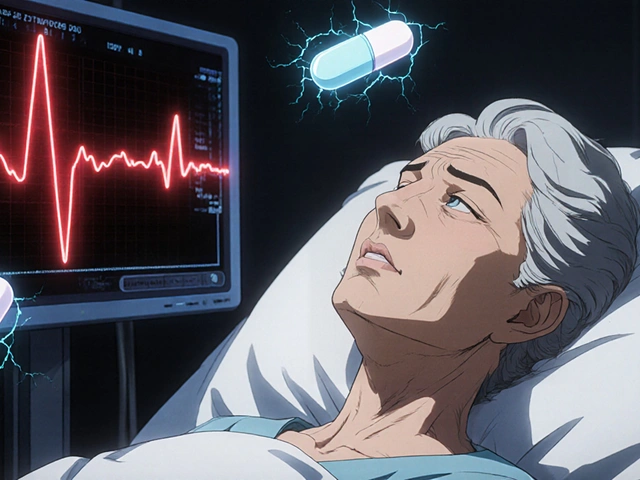
There is no cure. No drug stops MSA from progressing. Everything now is about managing symptoms and trying to keep people comfortable as long as possible.
For low blood pressure, doctors prescribe fludrocortisone, midodrine, or droxidopa. These help you stand without fainting - but they don’t fix the root problem. They just patch the leak.
Levodopa is still tried, even though it rarely works. Doctors give high doses for up to six months. If there’s no improvement, they stop. It’s not worth the side effects.
Physical therapy helps maintain mobility longer. Speech therapy teaches safer swallowing techniques. Bladder catheters, absorbent products, and medications for overactive bladder are standard. Sleep studies and CPAP machines help with apnea. Feeding tubes may be needed when swallowing becomes too risky.
But here’s the truth: none of this changes the outcome. It just changes how you get there.
The Future: Hope on the Horizon?
Research is slow. Very slow. As of late 2023, there are only three active clinical trials worldwide targeting the root cause of MSA. One major trial tested an immunotherapy designed to clear alpha-synuclein - the toxic protein that builds up in MSA brains. The results? A 1.2-point slower decline on a rating scale over 18 months. That’s barely noticeable.
Scientists are now working on a biomarker panel - combining MRI scans, blood tests, and autonomic function tests - to diagnose MSA within the first year. That’s critical. By the time symptoms appear, half to two-thirds of the brain cells that control movement and autonomic function are already dead. If we could catch it earlier, maybe treatments could actually help.
But the reality? Experts agree: without a breakthrough in understanding how MSA starts and spreads, survival won’t improve much in the next decade. The median life expectancy will likely stay around 6 to 10 years.
What It Feels Like to Live With MSA-P
One patient, diagnosed at 52, wrote on a support forum: "Within 18 months, I needed a cane. By three years, I was on a walker. By four, I was in a wheelchair. I can’t hold my coffee cup anymore. I can’t kiss my daughter without choking on my own saliva. I don’t know if I’ll see my grandson’s first steps. I just know I won’t see his fifth birthday."
Another, 55, said: "My neurologist said most of us don’t live beyond eight years. I thought I had time. I was wrong. Every day feels like counting down."
Seventy-eight percent of MSA patients rate their quality of life as poor or very poor within four years of diagnosis. That’s nearly four times higher than Parkinson’s patients at the same stage.
There’s no sugarcoating it. MSA-P is brutal. It doesn’t just take your mobility - it takes your dignity, your independence, your ability to be present for the people you love. And it does it fast.
Right now, the best we can do is recognize the signs early, manage symptoms with care, and give people the support they need - not just medically, but emotionally. Because for those living with MSA-P, time isn’t just limited. It’s ticking louder than ever.
Is Multiple System Atrophy the same as Parkinson’s disease?
No, MSA is not the same as Parkinson’s disease. While both cause movement problems like stiffness and slowness, MSA is more aggressive and involves widespread damage to brain regions controlling autonomic functions - like blood pressure, bladder control, and breathing. Unlike Parkinson’s, MSA responds poorly to levodopa, and autonomic symptoms often appear before motor issues. Survival time is also much shorter - typically 6 to 10 years after symptoms begin.
Can MSA be cured?
There is no cure for MSA. No medication has been shown to stop or reverse the progression of the disease. Current treatments focus on managing symptoms - such as low blood pressure, bladder problems, and sleep disturbances - to improve comfort and quality of life. Research into disease-modifying therapies is ongoing, but no breakthrough has been confirmed yet.
How quickly does MSA-P progress compared to Parkinson’s?
MSA-P progresses much faster than Parkinson’s. Most people with MSA-P need a walker within 3 to 4 years and a wheelchair by 5 years. In contrast, many Parkinson’s patients remain independent for 10 to 15 years or longer. The median survival for MSA-P is 6 to 10 years, while Parkinson’s patients often live 15 to 20 years after diagnosis.
Why do people with MSA have such severe autonomic symptoms?
MSA damages nerve cells in the brainstem and other areas that control the autonomic nervous system - the part of the brain that regulates heart rate, blood pressure, digestion, and bladder function. This damage happens early and spreads quickly. As a result, symptoms like fainting, urinary incontinence, erectile dysfunction, and sleep apnea are common and often appear before movement problems.
What are the main causes of death in MSA-P?
The leading causes of death in MSA-P are respiratory infections (45%), especially aspiration pneumonia from swallowing difficulties; sudden cardiac death (20%); and complications from choking or breathing problems during sleep (15%). These outcomes are directly linked to the progressive loss of control over autonomic and motor functions.
Are there any new treatments being tested for MSA?
Yes, but progress is slow. As of 2024, there are only three active clinical trials worldwide targeting MSA’s root cause. One major trial tested an immunotherapy designed to clear alpha-synuclein protein buildup - the hallmark of MSA. Results showed only a minor slowing of decline. Researchers are now focusing on early diagnosis using biomarkers like blood tests and advanced MRI scans to catch the disease before major brain damage occurs.
How is MSA diagnosed?
MSA is diagnosed based on clinical symptoms, MRI findings (like the "hot cross bun" sign in the brainstem), and autonomic testing. Blood tests for neurofilament light chain - a marker of nerve damage - are increasingly used. A diagnosis becomes more certain after 3 to 5 years, when autonomic failure is clearly present alongside motor symptoms. Early diagnosis remains challenging, with accuracy improving only after symptoms have progressed.





TiM Vince
January 12, 2026 AT 19:51My uncle had MSA. He was 54 when they diagnosed him. By 57, he couldn’t stand without help. The worst part wasn’t the shaking or the falling-it was the silence. He stopped talking because he was scared he’d choke. We’d sit there for hours just holding his hand. No one talks about how lonely it is to watch someone fade like that.
Sona Chandra
January 13, 2026 AT 07:29Ugh this is why I hate how doctors just call everything Parkinson’s. My cousin got misdiagnosed for 2 years. They gave her levodopa like it was magic. She kept falling. She kept peeing herself. They didn’t even check her blood pressure until she passed out in the grocery store. Then they said ‘oh maybe it’s MSA’ like it was an afterthought. Fuck that. They need to test for autonomic failure FIRST.
Jennifer Phelps
January 14, 2026 AT 03:20So if you have low BP and trouble walking at 50 you’re basically toast? Like there’s no gray area? What about people who get better with physical therapy or diet changes? I feel like this post makes it sound like it’s a death sentence the second you get a tremor. I get it’s bad but is it always this hopeless? 🤔
beth cordell
January 15, 2026 AT 09:37This broke me. 😔 My dad’s neurologist said ‘it’s probably Parkinson’s’ and we were relieved. Turns out it wasn’t. He didn’t make it past 60. I wish someone had told us earlier. I wish I’d known what to look for. I wish I’d held his hand more before he couldn’t hold mine back. 💔
Daniel Pate
January 17, 2026 AT 01:09The real tragedy isn’t just the biological collapse-it’s the societal one. We treat neurodegenerative diseases like personal failures rather than systemic failures of medical infrastructure. Why are there only three clinical trials globally for a disease that kills half its patients in under a decade? Where’s the funding? Where’s the urgency? We throw billions at cancer research while MSA patients die in silence because their symptoms don’t fit the narrative. This isn’t just medical-it’s moral.
Amanda Eichstaedt
January 18, 2026 AT 18:02I work in hospice care. I’ve seen Parkinson’s. I’ve seen ALS. I’ve seen MSA. The difference? With Parkinson’s, people still laugh. They still go to grandkids’ soccer games. With MSA? By year three, they’re just waiting. Not because they’re giving up. Because their bodies won’t let them do anything else. The dignity goes first. Then the voice. Then the breath. And no one talks about how quiet the room gets when the last laugh fades.
Jose Mecanico
January 20, 2026 AT 02:29I’m a PT. We do everything we can-balance training, swallow therapy, adaptive equipment. But with MSA, it’s like trying to hold back the tide with a spoon. We can delay the fall, but not stop it. I’ve had patients cry because they could still hold a cup… for one more week. That’s the fight. Not for recovery. Just for one more moment of normal.
Abner San Diego
January 21, 2026 AT 12:58Let’s be real. This is what happens when you let Big Pharma ignore rare diseases. They don’t make money on MSA. No big market. No patent goldmine. So they don’t care. The ‘hot cross bun’ sign? Found in 80% of cases. But we still wait 3-5 years to diagnose it? That’s not medicine. That’s negligence dressed in white coats. Someone should sue every neurologist who misses this for a year.
Eileen Reilly
January 23, 2026 AT 11:36im so tired of people acting like msa is some mystery disease. its just parkinsons but worse and no one wants to admit it because then they’d have to face how broken our healthcare system is. also why do you keep saying ‘median survival’ like its some kind of stat you can win? its just a number for people who are dying. stop being clinical and start being human.