If you're taking warfarin or an SSRI, and you love grapefruit, you might be wondering: is this combo safe? It’s not just a myth or a vague warning on a pill bottle. The interaction between grapefruit and certain medications is real, measurable, and sometimes dangerous. This isn’t about occasional juice - it’s about how your body breaks down drugs, and what happens when grapefruit throws a wrench in the system.
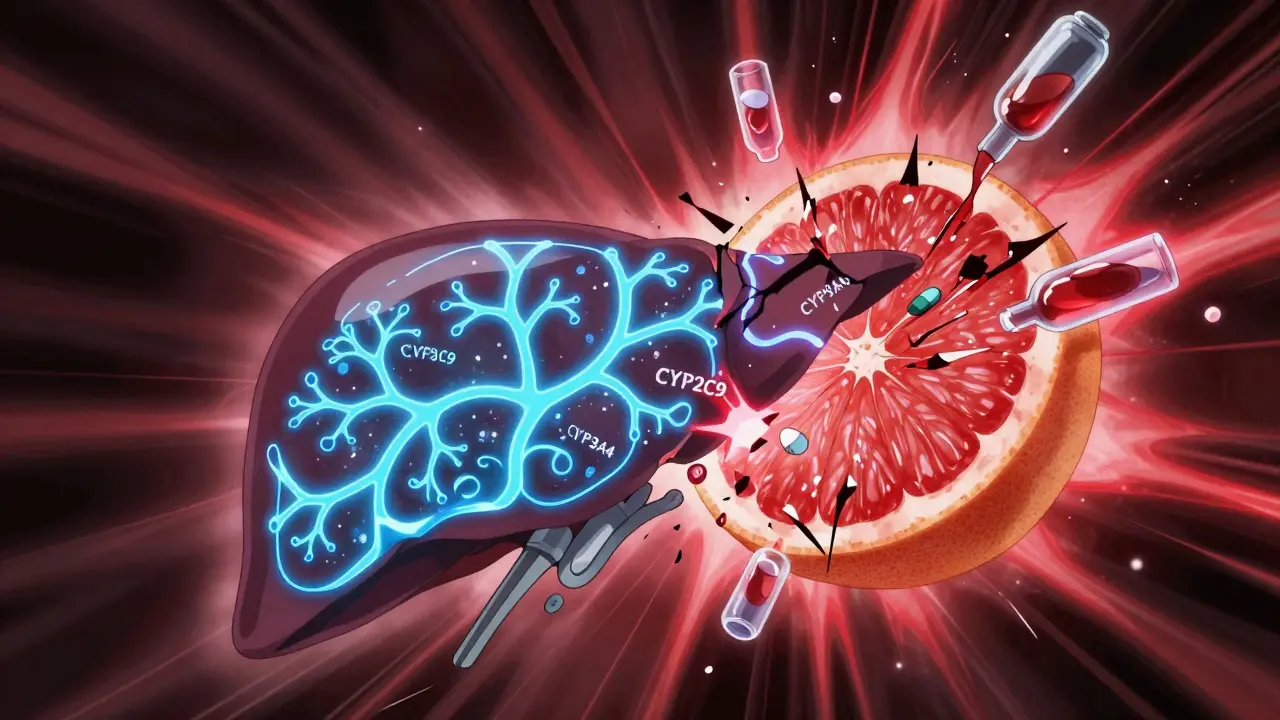
What Is CYP450, and Why Does It Matter?
Your liver and intestines are home to a family of enzymes called cytochrome P450 (CYP450). These enzymes act like molecular scissors, cutting up drugs so your body can get rid of them. About 75% of all prescription medications rely on these enzymes to be processed. Three key players here are CYP3A4, CYP2C9, and CYP2D6. Each one handles different drugs. If one of them gets blocked, those drugs build up in your blood - and that can lead to serious side effects.
Take warfarin, for example. It’s a blood thinner used to prevent clots. Too little, and you risk clots. Too much, and you could bleed internally. That’s why it has a narrow therapeutic index - the difference between a safe dose and a dangerous one is razor-thin. About 80-90% of warfarin is broken down by CYP2C9. The rest goes through CYP3A4. Now, here’s the problem: grapefruit doesn’t just mess with CYP3A4. It also quietly inhibits CYP2C9.
Grapefruit: The Silent Enzyme Killer
Grapefruit isn’t just a fruity snack. It’s packed with chemicals called furanocoumarins - mainly bergamottin and DHB. These compounds don’t just temporarily block CYP enzymes. They permanently damage them. Once they bind to the enzyme, the cell destroys the whole thing. It’s not like a traffic jam that clears up. It’s more like smashing a factory machine. Your body has to build new enzymes from scratch, which takes days.
Research from Dresser et al. (1998) showed that a single glass of grapefruit juice can knock out 47% of intestinal CYP3A4 for up to 72 hours. That means even if you take your medication at night and drink juice in the morning, you’re still at risk. The effect isn’t about timing - it’s about lasting damage. And it’s not just grapefruit juice. Whole grapefruit, pomelos, and even some hybrid citrus like ‘Oroblanco’ and ‘Sweetie’ can be worse. The FDA warned in 2023 that these newer varieties can have up to 300% more furanocoumarins than traditional grapefruit.
Warfarin and Grapefruit: The Real Risk
You’ll hear conflicting things about warfarin and grapefruit. Some doctors say avoid it completely. Others say the risk is low. The truth? It’s complicated. Clinical studies show inconsistent results. Why? Because warfarin doesn’t rely on just one enzyme. It’s also affected by your genes - specifically, variations in the VKORC1 gene and CYP2C9 polymorphisms like *2 and *3. People with these variants break down warfarin much slower. Add grapefruit into the mix, and their levels can spike dangerously.
A 2021 guideline from the Clinical Pharmacogenetics Implementation Consortium (CPIC) recommends avoiding grapefruit entirely for patients with CYP2C9*2 or *3 variants. In one study, patients with these variants saw INR levels rise 15-25% after consuming grapefruit. That’s enough to push someone from a safe range into bleeding territory. Yet, many patients don’t know their genetic status. Genetic testing for CYP2C9 costs $250-$400, and it’s not routinely done. So unless you’ve been tested, you’re flying blind.
Real-world data from Drugs.com shows 8.7% of warfarin users specifically avoid grapefruit. But only 18% of warfarin prescriptions include a warning about it. That gap between awareness and action is dangerous.

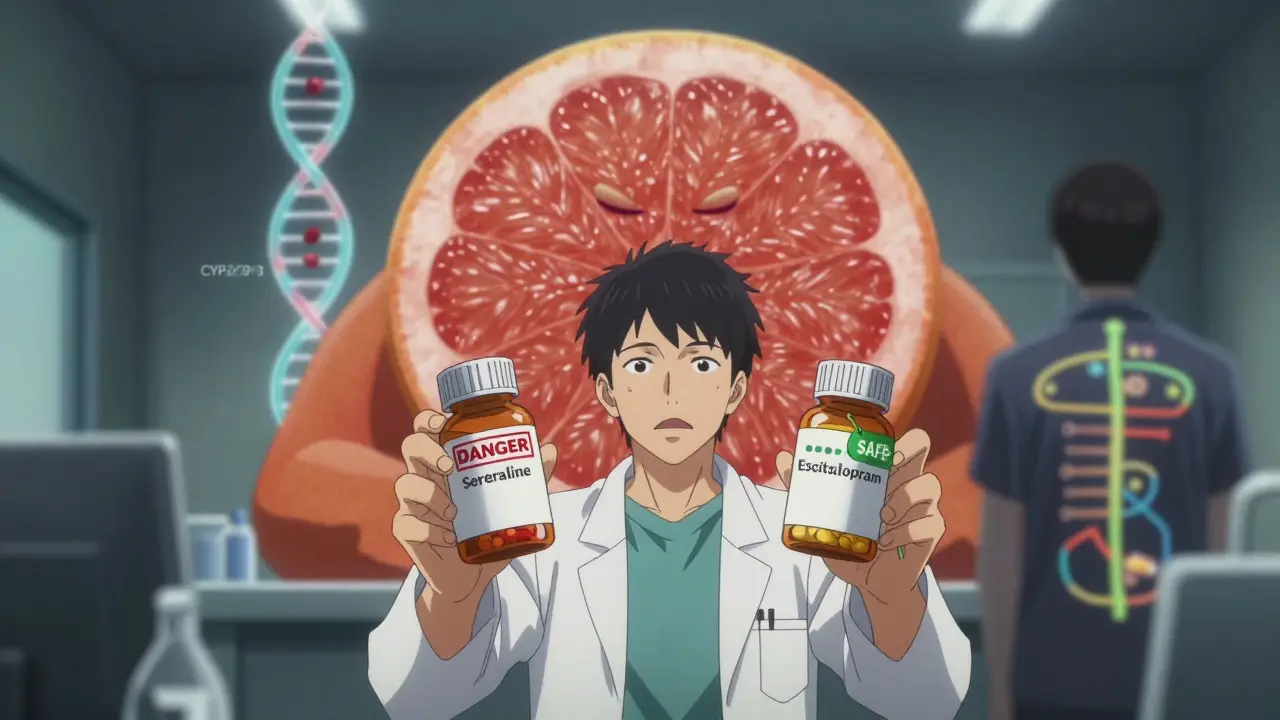
SSRIs and Grapefruit: Not All Are Equal
SSRIs are a whole different story. Not every SSRI interacts with grapefruit - and the ones that do, do it differently. Here’s the breakdown:
- Fluoxetine and paroxetine: Metabolized mainly by CYP2D6. Grapefruit has minimal effect on this enzyme. So, low risk.
- Citalopram and escitalopram: Broken down by CYP2C19 and CYP3A4. A March 2024 study in Clinical Pharmacology & Therapeutics found no significant interaction between escitalopram and grapefruit juice in healthy volunteers.
- Sertraline: This one’s the red flag. It’s metabolized by CYP2C9, CYP2C19, and CYP3A4. That triple pathway means grapefruit can hit it from multiple angles. A 2015 case series found sertraline blood levels rose 27-39% in people who drank grapefruit juice daily. Symptoms? Nausea, dizziness, increased drowsiness - classic signs of SSRI toxicity.
- Trazodone and vilazodone: Also on the FDA’s list of drugs with serious grapefruit interactions. They’re less common, but still worth noting.
So if you’re on sertraline, avoid grapefruit. If you’re on escitalopram, you’re probably fine. But don’t assume. Talk to your pharmacist. Ask: “Which enzyme does my drug use?”
Why Some People Are More at Risk
Not everyone reacts the same way. Your risk depends on three things:
- Your genetics: Do you have slow-metabolizer variants in CYP2C9 or CYP2D6? That’s fixed - you’re born with it.
- Your gut health: The CYP3A4 enzyme is most concentrated in your small intestine. People with higher baseline levels get hit harder.
- Your age and liver function: Older adults and those with liver disease process drugs slower. Grapefruit makes it worse.
And here’s the kicker: grapefruit doesn’t just affect oral drugs. It can change how much of a drug gets into your bloodstream before it even reaches your liver. That’s why drugs with low bioavailability - like sertraline (44%) or some statins - are especially vulnerable. A small change in absorption can mean a big change in effect.
What Should You Do?
Here’s the practical advice - no guesswork:
- If you’re on warfarin: Avoid grapefruit entirely unless you’ve had genetic testing and your doctor says it’s safe. Even then, monitor INR closely.
- If you’re on sertraline: Skip grapefruit. It’s not worth the risk. Switch to orange juice or another citrus that doesn’t contain furanocoumarins.
- If you’re on escitalopram, citalopram, fluoxetine, or paroxetine: The risk is low. Still, if you drink grapefruit juice daily, watch for side effects like nausea, dizziness, or unusual fatigue. Talk to your doctor.
- Don’t rely on “I take it 12 hours apart.” That doesn’t work. The enzyme damage lasts days.
- Check your other meds too. Statins like simvastatin, blood pressure drugs like amlodipine, and even some anti-anxiety pills like buspirone also interact. Grapefruit doesn’t just play with one drug - it plays with your whole regimen.
Pharmacists at Mayo Clinic spend an average of 3.2 minutes per patient counseling on grapefruit interactions. Most of that time is spent on warfarin. But with 4.7 million Americans on SSRIs and 1.2 million on warfarin, this is a massive public health blind spot. Only 8% of SSRI prescriptions mention grapefruit. That’s not enough.
The Bigger Picture
More people are eating grapefruit. USDA data shows consumption rose 17% from 2019 to 2023. At the same time, older adults - who take more meds - are growing in number. The European Medicines Agency predicts a 22% increase in grapefruit-drug interactions by 2030. We’re heading for a wave of avoidable side effects.
The FDA is starting to respond. Their 2024 draft guidance now requires drug manufacturers to test for CYP inhibition early in development. That means future drugs might come with clearer labels. But for now? You’re on your own.
Bottom line: Know your meds. Know your juice. Don’t assume it’s safe. If you’re unsure, ask your pharmacist. Bring your pill bottle. Point to the grapefruit on the label. Ask: “Is this one dangerous?” Most will say yes - and save you a trip to the ER.
Can I just eat grapefruit a few hours after taking my medication?
No. Grapefruit doesn’t just block enzymes temporarily - it destroys them. Once the enzymes are damaged, your body needs days to make new ones. Even if you take your medication at night and drink grapefruit juice in the morning, you’re still at risk. The effect lasts 24 to 72 hours. Timing doesn’t fix it.
Is orange juice safe if I’m on warfarin or an SSRI?
Yes. Regular orange juice doesn’t contain furanocoumarins, the chemicals in grapefruit that cause interactions. But be careful with some ‘orange’-flavored juices or blends - some add grapefruit juice or pomelo. Always check the ingredient list. Stick to plain orange juice if you’re unsure.
Do all SSRIs interact with grapefruit?
No. Only SSRIs that are metabolized by CYP3A4 or CYP2C9 are at risk. Sertraline is the main one. Escitalopram and citalopram have low risk based on recent studies. Fluoxetine and paroxetine are mostly handled by CYP2D6, which grapefruit barely affects. So it’s not about the drug class - it’s about the specific metabolic pathway.
Should I get tested for CYP2C9 gene variants if I’m on warfarin?
It’s not required, but it’s smart. If you’ve had unexplained INR swings, or if you’re planning long-term warfarin use, genetic testing can tell you if you’re a slow metabolizer. That changes your risk with grapefruit and other drugs. The test costs $250-$400 and is covered by some insurance. Talk to your doctor or a pharmacogenetics specialist.
What if I accidentally ate grapefruit while on warfarin?
Don’t panic. One small amount is unlikely to cause harm. But if you regularly consume grapefruit and you’re on warfarin, get your INR checked within 3-5 days. Watch for signs of bleeding - unusual bruising, nosebleeds, dark stools, or headaches. If you notice any, call your doctor. Prevention is better than reaction.

Brad Ralph
February 14, 2026 AT 02:59christian jon
February 14, 2026 AT 11:47Suzette Smith
February 16, 2026 AT 00:35Autumn Frankart
February 16, 2026 AT 23:32Skilken Awe
February 17, 2026 AT 19:58Carla McKinney
February 18, 2026 AT 06:44Ojus Save
February 18, 2026 AT 14:04Jack Havard
February 20, 2026 AT 00:51Luke Trouten
February 21, 2026 AT 22:05Gabriella Adams
February 23, 2026 AT 01:10Vamsi Krishna
February 23, 2026 AT 05:15Steve DESTIVELLE
February 25, 2026 AT 02:40