Ever stared at your prescription bottle and thought, Wait, what does this actually mean? You’re not alone. Millions of people in the U.S. take multiple medications every day, and unclear instructions are one of the most common reasons people take them wrong-sometimes with dangerous results.
The FDA says over 200 high-risk drugs, like opioids, isotretinoin, and birth control pills, come with mandatory Medication Guides. But what about the rest? Most prescriptions don’t come with printed guides, and even when they do, the language can be confusing. Terms like "take as needed," "BID," or "q.d." aren’t just vague-they’re dangerous. The Institute for Safe Medication Practices (ISMP) estimates that unclear instructions contribute to more than 1.5 million medication-related injuries each year in the U.S. That’s not a small number. It’s a public health problem.
What Makes Medication Instructions Confusing?
It’s not just poor handwriting on a paper script. The problem runs deeper. Many prescriptions use outdated abbreviations that look harmless but can cause serious mistakes. For example:
- "q.d." means "daily," but it can be mistaken for "q.i.d." (four times a day)
- "IN" might stand for intranasal, but someone could read it as IV (intravenous)
- "d" in "mg/kg/d" could mean "day" or "dose"-and mixing those up changes everything
The ISMP banned these abbreviations in 2019 for good reason. But not every prescriber follows the rules. Some still write "twice daily" as "BID," or use Roman numerals like "V" instead of "5." And then there’s the issue of manufacturer differences. The same drug-say, a generic version of Depakote-might come with different dosing instructions depending on which company made it. One says "take with food," another says "take on an empty stomach." Who do you believe?
Even timing matters. If your doctor says "take twice daily," does that mean 8 a.m. and 8 p.m.? Or 7 a.m. and 7 p.m.? MD Anderson Cancer Center says the goal is to space doses as close to 12 hours apart as possible. But if you’re taking a cholesterol pill, Harvard Health says bedtime is best-because your liver makes more cholesterol at night. Without clear context, you’re guessing.
What You Should Do When Instructions Are Unclear
You don’t have to accept vague directions. Here’s what to do next time you’re unsure:
- Don’t guess. If you don’t understand how to take it, don’t assume. Even if you’ve taken it before, things change. Dosages shift. New side effects emerge.
- Call your pharmacist. Pharmacists are trained to decode prescriptions. They see hundreds of these every day. Ask: "What exactly does this mean?" and "Is there a chance this could be confused with something else?"
- Ask about timing. "Should I take this with food? At night? Right after waking up?" Timing affects how well the drug works-and whether it causes side effects.
- Clarify "as needed" drugs. This phrase is one of the most dangerous. "Take as needed for pain" sounds simple-but how many pills? How often? What’s the max per day? A pharmacist at Massachusetts General Hospital says you need to know the intent: "Is this for occasional use or daily relief?"
- Compare manufacturer labels. If you refill your prescription and the instructions changed, check the new bottle. If it’s different from last time, ask why. The NIH says this kind of inconsistency is real-and it can affect your health.
Don’t wait until you feel sick or get a side effect. Ask before you take the first pill.

How Providers Should Handle Confusing Instructions
It’s not just on you. Doctors, nurses, and pharmacists have responsibilities too.
In outpatient settings-like your local pharmacy-the FDA requires that Medication Guides be handed to you every time you pick up a high-risk drug. But in hospitals or nursing homes, those guides aren’t required. Instead, staff are supposed to explain the medication to you directly. But how often does that actually happen?
The National Coordinating Council for Medication Error Prevention and Reporting (NCC MERP) says healthcare providers must discuss three things with patients: the name of the drug, its purpose, and what effects to expect. That’s not optional. It’s a safety standard.
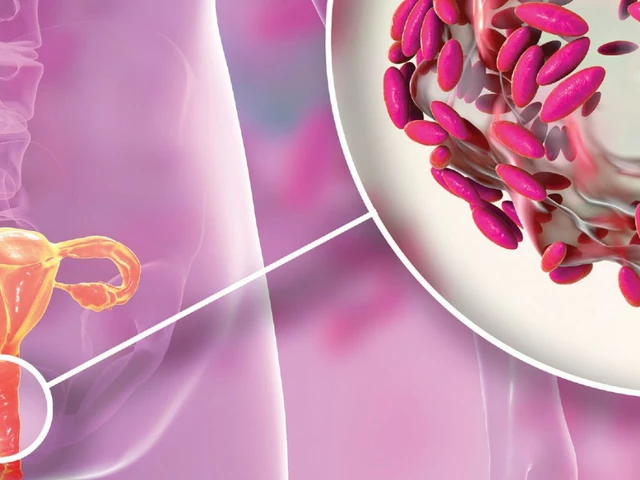
And here’s something many people don’t know: if you’re prescribed a generic drug, your pharmacist should tell you if the manufacturer’s instructions differ from the brand name. The NIH recommends that prescribers review instructions from all manufacturers and explain any differences. That’s not happening in most places. Patients are left to figure it out themselves.
That’s why some clinics now use electronic systems that pull in all manufacturer instructions and flag conflicts. The NIH says this is the future-but right now, it’s rare.
What to Say When You Ask for Clarification
You don’t need to be an expert to ask the right questions. Here are simple, direct phrases that work:
- "Can you write this out in plain words? I don’t understand what ‘BID’ means."
- "Is this supposed to be taken with food or without?"
- "What happens if I take it at 6 a.m. instead of 8 a.m.?"
- "Is there a maximum number of doses I can take in one day?"
- "I got this from a different pharmacy last time-why are the instructions different?"
Pharmacists and doctors hear these questions all the time. They expect them. In fact, Harvard Health says: "If you’re unsure exactly how to take a medication, even if it was already explained to you, ask for clarification." That’s not just advice-it’s a safety rule.

Tools That Help You Keep Track
Memory fails. Stress clouds judgment. That’s why tools matter.
The CDC recommends setting phone alarms or using pill organizers for complex schedules. If you’re taking five different pills at different times, write it down. Use a simple chart: one column for the drug name, one for the dose, one for the time, and one for notes (like "with food" or "avoid alcohol").
Some pharmacies offer free apps that send reminders and explain dosing in plain language. Ask yours if they have one. Even a printed calendar taped to your fridge can prevent a mistake.
And always double-check what you pick up at the pharmacy against your prescription. The Montana Department of Public Health says this step is critical. If the pill looks different, the dose is different, or the instructions changed-stop. Ask.
Why This Matters More Than You Think
Medication errors aren’t just about forgetting a pill. They’re about taking too much, too little, at the wrong time, or with the wrong food. The result? Hospital visits, organ damage, even death.
Four out of five American adults take at least one prescription drug. One in four take three or more. That’s a lot of chances for something to go wrong. And when instructions are unclear, the burden falls on the patient to figure it out.
But you don’t have to be the one solving a puzzle that should’ve been solved before it got to you. You have the right to clear, simple, consistent instructions. And the people who write those prescriptions have the responsibility to make them that way.
Clear medication instructions aren’t a luxury. They’re a requirement for safe care.
What should I do if my prescription instructions changed when I refilled my medication?
Don’t assume the change is intentional. Compare the new bottle’s instructions to the old one. If they differ-especially in dosage, timing, or food requirements-call your pharmacist or doctor. The same drug from different manufacturers can have different directions. Your provider should explain why the change happened and whether it affects your treatment.
Can I ask my pharmacist to explain my medication even if I didn’t have a question?
Yes, absolutely. Pharmacists are trained to counsel patients on medications, and they’re required to do so for high-risk drugs. Even for routine prescriptions, you have the right to ask: "How do I take this? What should I watch out for?" Most pharmacists will gladly walk you through it. Don’t feel like you’re bothering them-they’re there to help you avoid mistakes.
What’s the difference between a Medication Guide and regular prescription instructions?
A Medication Guide is a printed handout required by the FDA for certain high-risk drugs-like opioids, birth control, or isotretinoin-that can cause serious side effects. It’s written in plain language and must be given to you each time you fill the prescription. Regular prescription instructions are just what’s written on the label or in the script, and they’re not always clear. Not every drug comes with a Medication Guide, so you still need to ask questions even if you didn’t get one.
Are abbreviations like "BID" or "q.d." still allowed on prescriptions?
They shouldn’t be. The Institute for Safe Medication Practices banned these abbreviations in 2019 because they cause dangerous errors. But not all prescribers follow the guidelines. If you see "BID," "q.d.", or "IN," ask for clarification. Request that the instructions be written out fully: "twice daily," "daily," or "intranasal." Your safety matters more than outdated shorthand.
How can I tell if my medication is supposed to be taken at night?
Some medications, like cholesterol-lowering statins, are designed to be taken at bedtime because your body makes more cholesterol overnight. Others, like corticosteroids, are taken in the morning to match your body’s natural hormone cycle. If the label doesn’t say, ask your pharmacist or doctor. Don’t guess-timing affects how well the drug works and whether you’ll experience side effects.





Adrienne Dagg
December 19, 2025 AT 02:51OMG YES 🙌 I took my blood pressure med wrong for WEEKS because I thought 'BID' meant 'before breakfast'... my pharmacist facepalmed so hard I thought she'd collapse. Don't be like me. Just ask. It's not dumb, it's smart.
Ryan van Leent
December 19, 2025 AT 04:17Why are we even talking about this like it's a new problem? Pharmacists have been yelling about this since the 90s and nobody listens until someone dies. People just want their pills and don't wanna think. That's not ignorance, that's laziness. And now we're surprised when people overdose on Tylenol because they thought 'every 6 hours' meant 'every time I wake up'?
Stop acting like this is a system failure. It's a human failure.
Kinnaird Lynsey
December 20, 2025 AT 01:22I used to be the person who just swallowed pills without reading anything. Then my grandma had a bad reaction to a generic version of her heart med because the new bottle said 'take with food' and the old one said 'take on empty stomach.' She ended up in the ER. Now I compare every bottle like it's a treasure map. Turns out, being paranoid saves lives.
Also, pharmacists are way more helpful than doctors. Go talk to them. They're not there to sell you stuff. They're there to stop you from killing yourself.
shivam seo
December 21, 2025 AT 07:44Typical American medical chaos. In Australia, we have standardized electronic prescriptions with plain-language instructions built in. No abbreviations. No guesswork. No 'q.d.' nonsense. You think your system is advanced? It's a joke. We don't let people die because someone can't read cursive. We fix the system. You guys just yell at patients to 'ask more questions.' Like that's the solution.
Stop blaming the victim. Fix the damn software.
benchidelle rivera
December 21, 2025 AT 22:09As a nurse who’s seen patients collapse from misread scripts, I cannot stress this enough: YOU HAVE THE RIGHT TO CLARITY. If your pharmacist gives you a blank stare when you ask what 'BID' means, they’re not doing their job. Demand a printed sheet with full sentences. Write it down. Tape it to your mirror. This isn’t optional. It’s your body on the line.
And if your doctor uses Roman numerals? Tell them to use a keyboard. You’re not paying them to play Scrabble with your life.
Andrew Kelly
December 22, 2025 AT 07:38Let me guess - this is part of the Big Pharma agenda to make you dependent on pharmacists. Why do you think they banned abbreviations? So you’d have to go back to them every time you refill? So they can upsell you on 'medication counseling' packages? The real danger isn't 'q.d.' - it's the system turning you into a customer who needs constant hand-holding just to take a pill.
My grandpa took warfarin for 20 years with zero instructions. He lived to 94. Maybe we don’t need all this over-explaining. Maybe we need less fear-mongering.
Anna Sedervay
December 22, 2025 AT 11:45It is profoundly disconcerting that the American healthcare infrastructure has devolved into a labyrinthine quagmire wherein the onus of interpretative labor is unilaterally imposed upon the lay patient, who, by virtue of their non-specialist status, is epistemologically ill-equipped to discern the semantic nuances of archaic medical nomenclature. The proliferation of non-standardized abbreviations constitutes not merely negligence, but a systemic violation of the principle of informed consent.
Moreover, the fact that generic manufacturers are permitted to disseminate divergent dosing protocols-without mandatory cross-referential disclosure-is not only legally indefensible, but morally reprehensible. One must ask: if a pharmaceutical entity cannot guarantee lexical consistency across its product lines, why should it be granted regulatory licensure at all?
Forgive me for being blunt, but this is not a 'patient education' issue. This is a catastrophic failure of governance.
Matt Davies
December 24, 2025 AT 05:03I used to think meds were just pills you popped like M&Ms. Then I got prescribed something for my thyroid and my pharmacist sat me down with a whiteboard and drew me a timeline with little suns and moons for morning/night doses. I cried. Not because I was sad - because someone finally treated me like a human, not a barcode.
Don’t let anyone make you feel silly for asking. The right people? They’ll high-five you for it.
Dev Sawner
December 24, 2025 AT 18:42The root cause of this issue is the absence of a centralized, federally mandated pharmaceutical lexicon. In India, we have the National Formulary of India (NFI), which standardizes all prescription nomenclature across all manufacturers and prescribers. No ambiguity. No variations. No 'take with food' vs 'take without.' The system is rigid, yes - but it prevents error. The United States prioritizes corporate flexibility over patient safety. That is not innovation. That is recklessness.
Until the FDA enforces a single, legally binding language standard for all prescriptions - including generics - this problem will persist. And no amount of patient advocacy will fix a broken architecture.
Moses Odumbe
December 26, 2025 AT 13:08Y'all are overcomplicating this. Just use the Medisafe app. It tells you what to take, when, and even shows you a picture of the pill. Also, if your script says 'BID' - just screenshot it and paste it into Google. Boom. Instant translation. 🤖💊
Stop treating this like a crisis. It's a tech problem. And we have tech.
Kelly Mulder
December 27, 2025 AT 09:50This is why I refuse to take anything prescribed. I’ve seen too many people die from 'misinterpretation.' I rely on herbal supplements now. They’re not regulated either, but at least they don’t use Latin abbreviations to confuse you. And honestly? My blood pressure is better. Coincidence? I think not.