Multidisciplinary Treatment Plan Builder
Build Your Patient's Treatment Plan
Enter the patient's condition and symptoms to see which specialists should be part of the team and how they'll work together.
Recommended Team
Neurologist
Diagnoses underlying neural causes
Physical Therapist
Restores movement and strength
Occupational Therapist
Helps with daily functional tasks
How They Work Together
This team approach ensures comprehensive care by combining expertise in diagnosis, movement restoration, and real-world function. Each specialist contributes to creating an integrated treatment plan that addresses:
Neurologist identifies root causes through imaging and electrophysiology
Biomechanist maps movement patterns using motion capture
Occupational therapist creates personalized daily-life activities
Key Insight
The most effective treatment plans include all three core disciplines: neurological diagnosis, movement restoration, and functional application. The article emphasizes that this integrated approach addresses the complex nature of poor muscle control better than any single discipline alone.
Ever wonder why some patients bounce back from shaky movements while others stay stuck? The answer often lies in the team behind them, not just a single therapist. When muscle control is weak, throwing a single discipline at the problem is like using a hammer to fix a watch. A multidisciplinary approach brings together the right tools, perspectives, and timing to restore smooth, coordinated movement.
What "Poor Muscle Control" Really Means
Poor muscle control is a condition where the nerves and muscles fail to coordinate effectively, leading to tremors, weakness, or clumsy movements. It shows up in stroke survivors, athletes with overuse injuries, and even kids with developmental disorders. The root causes can be neural (damage to brain pathways), muscular (weak fibers), or biomechanical (poor joint alignment).
Why One-Size-Fits-All Won’t Cut It
Imagine trying to fix a leaky pipe by only tightening the bolts. You might stop the drip temporarily, but the underlying corrosion stays. Similarly, a single therapist can address a symptom-like stretching tight muscles-but may miss the nervous-system signal that’s driving the problem. That’s why integrating expertise from several fields is crucial.
Core Disciplines in the Team
- Physical therapy is a hands‑on practice focused on restoring movement, strength, and balance through exercises and manual techniques.
- Occupational therapy is a client‑centered approach that helps people perform daily tasks despite motor limitations.
- Neurology is the medical specialty that diagnoses and treats disorders of the nervous system, providing insight into the brain‑muscle link.
- Biomechanics is the study of forces acting on the body, informing optimal movement patterns and injury prevention.
- Neurorehabilitation is a specialized field that combines neuroscience and therapy to retrain the brain after injury.
- Motor learning is the process by which the nervous system acquires and refines movement skills through practice.
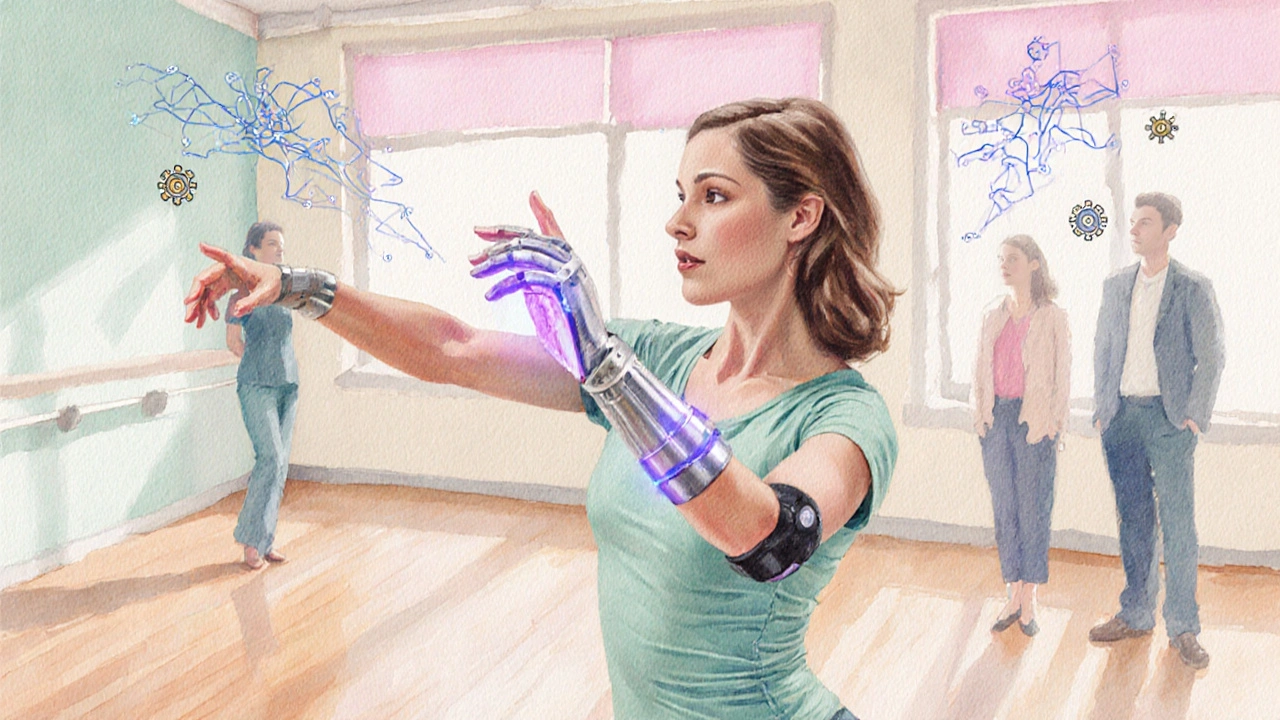
- Assistive technology is devices such as exoskeletons or biofeedback tools that augment or replace lost motor function.

How the Pieces Fit Together: A Step‑by‑Step Blueprint
- Identify the underlying cause. Neurologists run imaging and electrophysiology tests to pinpoint whether the issue is cortical, spinal, or peripheral.
- Map the movement deficits. Biomechanists use motion‑capture or simple video analysis to see where the gait or limb trajectory breaks down.
- Design a personalized therapy plan. Physical and occupational therapists translate that data into targeted exercises, functional tasks, and adaptive strategies.
- Integrate technology. Rehabilitation engineers introduce biofeedback, robotic assistance, or virtual‑reality drills that reinforce correct patterns.
- Teach motor‑learning principles. Therapists embed spaced repetition, variable practice, and mental rehearsal to solidify new pathways.
- Monitor and adjust. Regular check‑ins with the neurologist and biomechanist ensure the plan evolves as the nervous system rewires.
Comparison of Key Professionals
| Profession | Primary Focus | Typical Interventions | Key Outcome |
|---|---|---|---|
| Physical Therapist | Strength, balance, and movement mechanics | Progressive resistance, gait training, manual therapy | Improved force generation and stability |
| Occupational Therapist | Functional independence in daily life | Task‑specific drills, adaptive equipment, ADL coaching | Greater ability to dress, eat, and work |
| Neurologist | Diagnosing and managing nervous‑system pathology | Medication, nerve stimulation, referral coordination | Reduced neural inflammation, optimized signaling |
| Rehabilitation Engineer | Technology‑enhanced movement support | Exoskeletons, EMG biofeedback, VR environments | Accelerated neural plasticity and patient engagement |
Practical Checklist for Building Your Team
- Confirm a neurologist has reviewed the patient’s imaging and nerve studies.
- Schedule a biomechanical assessment to capture baseline movement patterns.
- Choose a physical therapist experienced with the specific condition (e.g., post‑stroke).
- Include an occupational therapist early to address daily‑life goals.
- Explore assistive‑technology options; ask about loaner programs.
- Set weekly case‑review meetings so every professional shares progress.
- Document motor‑learning milestones-number of successful repetitions, error rates, and confidence scores.
Common Pitfalls and How to Avoid Them
Pitfall 1: Over‑reliance on one discipline. If a physical therapist prescribes the same set of exercises for weeks, the brain may stop adapting. Counter it by rotating tasks, adding cognitive challenges, and bringing in a motor‑learning specialist.
Pitfall 2: Poor communication. Without a shared progress log, therapists may duplicate work or miss regression signs. Use a shared digital platform where each professional logs notes, EMG readings, and patient feedback.
Pitfall 3: Ignoring patient goals. Technical improvement means little if the patient can’t return to gardening or typing. Involve occupational therapists early to align the plan with real‑world tasks.
Success Story: From Tremor to Tap‑Dance
Laura, a 52‑year‑old accountant, suffered a minor cerebellar stroke that left her with shaky hands. Her neurologist ordered an MRI and referred her to a multidisciplinary clinic. A biomechanist mapped her hand trajectory, revealing excessive wrist flexion. The physical therapist introduced graduated resistance bands, while the occupational therapist practiced pouring water into a glass-a functional task Laura loved. A rehabilitation engineer fitted her with a lightweight EMG‑triggered glove that gave gentle vibration when she produced the correct grip force. Within three months, Laura could sign contracts without tremor and even joined a beginner tap‑dance class. Her story illustrates how each discipline filled a gap, creating a seamless path from diagnosis to daily life.
Future Trends: What’s on the Horizon?
Artificial‑intelligence‑driven gait analysis platforms are already feeding real‑time data to therapists, allowing on‑the‑fly adjustments. Wearable neurostimulators that deliver targeted pulses during specific movement phases are entering clinical trials. As these tools mature, the need for coordinated interpretation will only grow-making a multidisciplinary mindset the new standard of care.
Frequently Asked Questions
What exactly is "poor muscle control"?
It refers to the inability of the nervous system and muscles to work together smoothly. Symptoms can include tremors, weakness, clumsiness, or loss of coordination. Causes range from brain injuries and neurodegenerative diseases to musculoskeletal imbalances.
Why can’t a single therapist fix the problem?
Because the issue lives at the intersection of nerve signaling, muscle strength, joint mechanics, and functional tasks. One professional may address only one slice-like strength-but miss the neural timing or the daily‑life context.
How do I find the right team?
Start with a neurologist for a proper diagnosis. From there, ask for referrals to a physical therapist and occupational therapist with experience in neurorehabilitation. Check if the clinic has a biomechanics or rehabilitation‑engineering specialist, or if they partner with a university lab.
What role does technology play?
Assistive tech can amplify weak signals (e.g., EMG‑triggered gloves) or provide real‑time feedback (e.g., wearable motion sensors). Virtual‑reality simulations let patients practice tasks safely and repeatedly, accelerating motor learning.
How long does recovery usually take?
Recovery timelines vary widely. Mild weakness may improve in weeks with focused therapy, while post‑stroke re‑education can span months or years. The key is regular monitoring and adjusting the plan as the nervous system adapts.


Jean Tredoux
October 13, 2025 AT 13:51All these “multidisciplinary” buzzwords are just a cover for pharma's profit scheme.
cedric Gicquiaud
October 15, 2025 AT 21:25Look, the brain‑muscle loop is complex, and you can’t just throw PTs at it and hope for miracles; you need a neurologist to pinpoint the exact pathways that are misfiring, then a biomechanist to map the faulty kinetics, and finally a therapist to retrain the signals. Skipping any link in that chain is a recipe for wasted effort.
Lee Llewellyn
October 18, 2025 AT 04:58Oh sure, the magic wand of “multidisciplinary care” will instantly fix everything, right? Let’s pretend that every neurologist, PT, OT, and engineer can just hop on a Zoom call and solve centuries‑old neural deficits. In reality, the brain isn’t a Lego set you can rebuild by adding a few extra pieces. You need precise diagnostics, not just a generic “team meeting.” Even the most seasoned neurorehabilitation specialist will tell you that plasticity takes time, repetition, and motivation. Throwing more professionals into the mix doesn’t magically accelerate synaptic rewiring. It can actually create confusion if the communication channels are weak. Patients often end up with conflicting homework assignments, which leads to non‑adherence. Moreover, insurance companies love the multidisciplinary label because it justifies higher billing. That’s why you see a surge of “integrated clinics” popping up, each promising miracles. The truth is, every additional specialist adds a layer of logistics, paperwork, and coordination cost. If you cannot afford those extra sessions, the whole plan collapses. Also, technology like EMG‑feedback is great, but only when the therapist knows how to interpret the data. Otherwise it’s just flashy data that sits on a screen. The best outcomes still come from focused, evidence‑based protocols, not from a “more is better” mindset. So before you chant the multidisciplinary mantra, ask yourself if the team truly collaborates or just co‑exists under the same roof. If it’s the latter, you’re probably paying for a fancy label. Bottom line: multidisciplinary care works when each discipline is essential and well‑coordinated, not when it’s a marketing ploy.
Drew Chislett
October 20, 2025 AT 12:31Really love how the article breaks down each step – it makes it easier for patients to see where they fit in the puzzle. Getting the neurologist’s insight early on sets a solid foundation, and then layering PT and OT interventions tailors the rehab to real‑world goals.
Roger Bernat Escolà
October 22, 2025 AT 20:05Imagine the drama of a patient finally grasping a mug after weeks of trembling – it’s like watching a sunrise after a storm. The synergy between the brain and the muscles is poetic when the right experts conduct the orchestra.
william smith
October 24, 2025 AT 13:45It’s vital to have the neurologist confirm the diagnosis before the PT designs the exercises; otherwise you risk targeting the wrong pathways.
Kay Yang
October 26, 2025 AT 06:25That sarcastic take on multidisciplinary teams actually highlights the need for clear communication – without it, patients can feel lost.
Sadie Viner
October 28, 2025 AT 00:05From a clinical perspective, integrating functional tasks early on, as described, aligns therapy goals with patients’ daily lives, which improves adherence.
Debra Laurence-Perras
October 29, 2025 AT 17:45Agreed – the occupational therapist’s role in bridging therapy to real‑world activities can’t be overstated; it’s what makes the progress sustainable.
dAISY foto
October 31, 2025 AT 11:25Wow, when you think about it, the whole team is like a band, each instrument playing its part – the rhythm of recovery becomes a beautiful symphony.
And when that harmony hits, it’s truly life‑changing.
Ian Howard
November 2, 2025 AT 05:05The inclusion of rehabilitation engineers brings a cutting‑edge twist; wearable tech can give patients that extra edge when traditional methods plateau.
Chelsea Wilmer
November 3, 2025 AT 22:45Philosophically speaking, the notion of “poor muscle control” mirrors the broader human struggle between chaos and order; the multidisciplinary approach is our societal attempt to impose structure on that inherent disorder, echoing ancient debates about the balance of mind and body. By weaving together neurology, biomechanics, and functional therapy, we construct a narrative that transcends simple symptom management and ventures into the realm of personal identity reshaping.
David Stout
November 5, 2025 AT 16:25Great point about tech – but remember it’s only as good as the therapist who can interpret the data and adjust the plan.
Pooja Arya
November 7, 2025 AT 10:05While the article is thorough, it could have stressed more the ethical responsibility of clinicians to avoid over‑medicalizing normal variations in motor skill.
Sam Franza
November 9, 2025 AT 03:45Team meetings help keep everyone on the same page and reduce duplicated efforts.
Raja Asif
November 10, 2025 AT 21:25Only when the nation prioritizes funding for integrated rehab centers will patients truly benefit from these multidisciplinary models.
Cynthia Sanford
November 12, 2025 AT 15:05Loved the part about future AI gait analysis – it’s going to make personalized rehab a lot more accessible.
Yassin Hammachi
November 14, 2025 AT 08:45Balancing all these perspectives does sound challenging, but it also reflects the complexity of human movement, which is ultimately a collaborative dance between brain, muscle, and environment.