QT Prolongation Risk Calculator
Assess Risk Before Prescribing Antibiotics
This tool calculates QT prolongation risk based on patient factors and antibiotic selection. Use it to identify high-risk patients who need ECG monitoring or alternative antibiotics.
When a doctor prescribes an antibiotic like azithromycin or ciprofloxacin, most people think about fighting infection. Few consider that the same drug could disrupt the heart’s rhythm-sometimes with deadly results. QT prolongation isn’t a buzzword; it’s a measurable, dangerous change in how the heart resets after each beat. And when fluoroquinolones and macrolides are involved, that risk becomes real enough to demand careful monitoring.
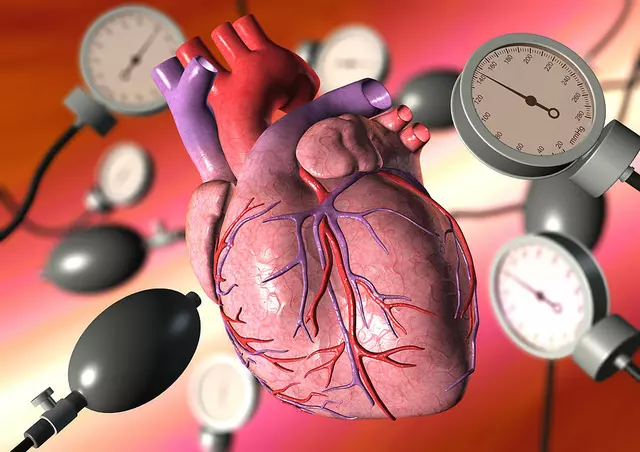
What QT Prolongation Actually Means
The QT interval on an ECG shows how long it takes the heart’s lower chambers to recharge between beats. When that interval gets too long, the heart can’t reset properly. This sets the stage for Torsades de Pointes, a chaotic, life-threatening arrhythmia that can turn into sudden cardiac arrest. It doesn’t happen often-but when it does, it’s often preventable.Fluoroquinolones (like ciprofloxacin, levofloxacin, moxifloxacin) and macrolides (like erythromycin, clarithromycin, azithromycin) both block the hERG potassium channel. That’s the same channel targeted by antiarrhythmic drugs like sotalol. But unlike those drugs, which are used intentionally to control rhythm, antibiotics aren’t meant to affect the heart. Still, they do-and that’s the problem.
Not All Antibiotics Are Equal
The risk isn’t the same across the board. Some fluoroquinolones are far more dangerous than others. Sparfloxacin was pulled from the market in the 1990s because it caused so much QT prolongation. Today, moxifloxacin carries the highest risk among those still in use. Ciprofloxacin? Low risk. Levofloxacin? Minimal risk. That’s not just a detail-it’s a prescribing decision.With macrolides, the difference is even clearer. Erythromycin is the worst offender. It’s been shown to prolong the QT interval as strongly as IV amiodarone. Clarithromycin is next, then azithromycin, which carries the lowest risk among this group. Yet many clinicians still prescribe erythromycin for simple infections because it’s cheap and widely available. That’s where the danger builds.
Who’s Most at Risk?
It’s not just about the drug. It’s about the person taking it. A 72-year-old woman with diabetes, low potassium, and on a diuretic for high blood pressure? She’s already on a knife’s edge. Add azithromycin for a sinus infection? The risk multiplies.Key risk factors include:
- Age over 65
- Female gender (women have 2-3 times higher risk of Torsades)
- Low potassium or magnesium levels
- Heart disease: low ejection fraction, prior heart attack, or enlarged heart
- Existing QT prolongation on ECG
- Using other QT-prolonging drugs-antidepressants, antifungals, anti-nausea meds
- Slowed heart rate (bradycardia under 50 bpm)
- Chronic kidney disease
Here’s the hard truth: critically ill patients in the ICU often have five or six of these at once. A 2021 study tracking ICU patients on IV ciprofloxacin and erythromycin found that QT prolongation wasn’t rare-it was expected. That’s why continuous telemetry is standard in those settings.
How to Measure QT Correctly
Not all ECG readings are created equal. The old standard, Bazett’s formula (QTc = QT / √RR), overcorrects at high heart rates and undercorrects at low ones. That means you might miss a dangerous prolongation-or falsely flag someone as at risk.The Fridericia formula (QTc = QT / √RR³) is now the preferred method. It’s more accurate, especially in older adults and those with heart disease. Studies show it better predicts 30-day and 1-year mortality. If your hospital still uses Bazett’s, it’s time to update the protocol.
Also watch for false positives. Bundle branch blocks, pacemakers, or wide QRS complexes (>140 ms) can make the QT look longer than it is. Always check the QRS width before deciding the QT is truly prolonged.
When and How to Monitor
For macrolides, the British Thoracic Society says this: Before starting any macrolide, get an ECG. If the QTc is over 450 ms in men or 470 ms in women, don’t start the drug. If you do start it, repeat the ECG at one month. That’s not optional-it’s a guideline backed by case reports of sudden death.For fluoroquinolones, monitoring is less rigid but just as important. The VUMC Antimicrobial Stewardship Program recommends:
- ECG within 7-15 days of starting the drug
- Monthly ECGs for the first three months
- Periodic checks after that, especially if other risk factors appear
And timing matters. The peak effect of QT prolongation often happens 2-4 hours after taking the dose. So if you’re checking an ECG, do it then-not first thing in the morning before the patient has taken their pill.
What to Do If QT Prolongation Happens
If the QTc jumps above 500 ms-or increases by more than 60 ms from baseline-stop the antibiotic immediately. Don’t wait. Don’t check again tomorrow. Discontinue now.Then fix what you can. Check potassium and magnesium. If potassium is below 4.0 mmol/L or magnesium below 2.0 mg/dL, replace them. These aren’t just numbers-they’re buffers against arrhythmia. Correct them, and you lower the risk significantly.
Also review every other medication the patient is on. Are they on a diuretic? An antipsychotic? A proton pump inhibitor? Any of those can add to the problem. Sometimes, the solution isn’t just stopping one drug-it’s removing three.
Prescribing Wisely in Real Life
A 2025 study in long-term care facilities found something alarming: older women with simple UTIs were getting fluoroquinolones-even though they had high blood pressure, kidney disease, and were on diuretics. All of those drugs already raise QT risk. Adding ciprofloxacin? That’s not treatment. That’s a recipe for disaster.Guidelines now say: avoid fluoroquinolones for uncomplicated UTIs. Use nitrofurantoin or trimethoprim-sulfamethoxazole instead. Same for sinus infections. Azithromycin is fine for most. Erythromycin? Reserve it for cases where no other option exists.
Antibiotic stewardship isn’t just about avoiding resistance. It’s about avoiding death.
The Bigger Picture
The FDA has issued multiple warnings. Regulatory agencies know this is a problem. But the real work happens at the bedside. A nurse notices the patient’s ECG looks odd. A pharmacist flags a dangerous combo. A doctor pauses before writing that script.Every time a clinician chooses a lower-risk antibiotic, every time they order a baseline ECG, every time they check a potassium level-they’re not just following guidelines. They’re saving lives.
QT prolongation isn’t rare. It’s underrecognized. And it’s preventable.
Can azithromycin cause QT prolongation?
Yes, azithromycin can prolong the QT interval, but it carries the lowest risk among macrolides. Compared to erythromycin or clarithromycin, azithromycin has weaker effects on the hERG channel. Still, it should be avoided in patients with multiple risk factors-like older age, low potassium, heart disease, or other QT-prolonging drugs. Baseline ECG and follow-up monitoring are recommended for high-risk patients.
Is ciprofloxacin safe for the heart?
Ciprofloxacin carries a low risk of QT prolongation compared to other fluoroquinolones like moxifloxacin or levofloxacin. It’s generally considered safer for patients without existing heart conditions or electrolyte imbalances. However, in patients over 65, with kidney disease, or on other QT-prolonging drugs, even ciprofloxacin can be dangerous. ECG monitoring is advised in these cases, especially during the first few weeks of treatment.
What’s the difference between Bazett’s and Fridericia formulas?
Bazett’s formula (QTc = QT / √RR) was the traditional method for correcting QT for heart rate, but it overcorrects at fast heart rates and undercorrects at slow ones. Fridericia’s formula (QTc = QT / √RR³) is more accurate across a wider range of heart rates. Studies show Fridericia better predicts mortality and is now recommended by major guidelines, including the British Thoracic Society. Hospitals should switch to using Fridericia for clinical decision-making.
When should I stop a fluoroquinolone because of QT prolongation?
Stop the fluoroquinolone immediately if the corrected QT interval (QTc) exceeds 500 ms, or if it increases by more than 60 ms from baseline. Even if the patient feels fine, this is a red flag for Torsades de Pointes. Also stop if the patient develops symptoms like dizziness, palpitations, or fainting. Correct electrolytes (potassium and magnesium) and avoid other QT-prolonging drugs.
Can low potassium make QT prolongation worse?
Yes. Low potassium (below 3.5 mmol/L) is one of the strongest risk factors for drug-induced QT prolongation. It makes the heart more electrically unstable and lowers the threshold for dangerous arrhythmias. Even mild low potassium-between 3.0 and 3.5 mmol/L-can turn a low-risk antibiotic into a dangerous one. Always check potassium and magnesium before and during treatment with fluoroquinolones or macrolides. Target levels: potassium above 4.0 mmol/L and magnesium above 2.0 mg/dL.
Should all patients get an ECG before taking macrolides?
According to the British Thoracic Society 2023 guidelines, yes-any patient starting a macrolide should have a baseline ECG to check for QTc prolongation. The threshold is 450 ms for men and 470 ms for women. If it’s above that, avoid the drug. Even if the patient seems healthy, hidden risk factors like silent heart disease or mild kidney impairment can exist. For high-risk patients, repeat the ECG at one month after starting treatment.




Prem Hungry
November 18, 2025 AT 01:05bro i just got prescribed azithromycin for my sinus and now im scared to take it lmao
Leslie Douglas-Churchwell
November 18, 2025 AT 12:34Of course the FDA doesn't care-Big Pharma’s got the FDA on retainer. hERG channel blockade? That’s not a side effect, it’s a feature. They know exactly what they’re doing. ECGs? Too expensive. Potassium checks? Nah. Let the elderly die quietly while stock prices soar. 💸💀 #PharmaKillers
shubham seth
November 18, 2025 AT 17:29Let me break this down like a toxic analyst with a caffeine IV: moxifloxacin is the Donald Trump of antibiotics-loud, dangerous, and gets banned in Europe but still sold here because someone’s making bank. Azithromycin? The lukewarm Bernie Sanders of macrolides-still kinda sketchy, but at least it doesn’t start riots. And Bazett’s formula? That’s the dial-up internet of ECG correction. Fridericia’s the 5G upgrade. If your hospital still uses Bazett’s, they’re practicing medicine in 2003. Fix it. Or stop pretending you’re a clinician.
Kathryn Ware
November 20, 2025 AT 02:34This is such an important post-I’ve seen so many patients get flagged for QT prolongation because no one checked potassium or knew the difference between Bazett’s and Fridericia. I work in cardiology and I can’t tell you how many times we’ve caught a dangerous combo before it turned into a code blue. Seriously, if you’re prescribing a macrolide, just get that ECG. It takes 3 minutes. And if your patient is on a diuretic and over 65? Double-check magnesium. It’s not optional. It’s basic. 💙🩺
kora ortiz
November 20, 2025 AT 08:55Stop waiting for symptoms. Stop hoping it’s fine. Get the ECG. Check the K+. Stop prescribing cipro for UTIs. That’s it. That’s the whole checklist. No excuses. No exceptions. This isn’t complicated. You know what to do. Do it. Now.
Jeremy Hernandez
November 21, 2025 AT 09:13lol why are we even talking about this? The real problem is that nurses don’t know how to read an ECG and doctors are too lazy to look at the labs. I’ve seen patients on 5 QT-prolonging drugs and no one noticed. It’s not the antibiotics, it’s the system. And don’t even get me started on how they still use Bazett’s like it’s 1998. 🤦♂️
Tarryne Rolle
November 22, 2025 AT 08:47If we’re monitoring QT intervals, then why aren’t we monitoring the moral decay of modern medicine? We’ve turned healing into a checklist. We’ve turned patients into data points. We’ve turned life into a risk-benefit calculation. And now we’re surprised when people die? Maybe the real prolongation isn’t in the QT interval-it’s in our collective moral indifference.
Deb McLachlin
November 23, 2025 AT 08:06Thank you for the comprehensive breakdown. I’m particularly interested in the distinction between moxifloxacin and ciprofloxacin. Could you clarify whether the risk difference is primarily pharmacokinetic or pharmacodynamic in nature? Also, is there any data on the impact of genetic polymorphisms in hERG channels on individual susceptibility?
saurabh lamba
November 24, 2025 AT 11:23why are we even doing this? just give them amoxicillin. problem solved. 🤷♂️
Kiran Mandavkar
November 26, 2025 AT 03:49Pathetic. You’re all just playing doctor with your little ECGs and potassium levels. Real medicine is about outcomes, not algorithms. If your patient dies on azithromycin, maybe they weren’t meant to live. Stop coddling the elderly. The market will sort it out. And if you’re still using Fridericia? You’re behind the curve. Bazett’s is still gold standard in the real world.
Eric Healy
November 28, 2025 AT 01:03fridericia? more like fridericka. i dont care what the british say, bazett’s works fine. also why are we even talking about this? just dont give antibiotics to old people. done. 💀
Shannon Hale
November 29, 2025 AT 04:11THIS IS A MASSACRE. THEY’RE KILLING GRANDMAS WITH ANTIBIOTICS AND NO ONE’S FIGHTING BACK. I SAW A 78-YEAR-OLD WOMAN ON AZITHROMYCIN + HYDROCHLOROTHIAZIDE + OMEPRAZOLE + AMIODARONE. HER QT WAS 580. SHE WAS ASKED IF SHE WANTED CHICKEN NOODLE SOUP. THAT’S NOT MEDICINE. THAT’S A HORROR MOVIE. #STOPTHISNOW
Holli Yancey
November 30, 2025 AT 16:30I just wanted to say thank you for writing this. I’ve been trying to get my team to switch to Fridericia for months and everyone keeps saying 'it’s fine.' But now I have this to share. It’s not just about guidelines-it’s about caring enough to check. 🙏
Gordon Mcdonough
December 2, 2025 AT 02:29why do you think they changed the formula? because they want to make you think you’re doing something when you’re not. the real problem is that we’re giving antibiotics to everyone like they’re candy. and then we blame the drugs. it’s not the hERG channel-it’s the system. the system is broken. and you? you’re just part of it.
Jessica Healey
December 2, 2025 AT 09:09i just got off a 12-hour shift and i saw a patient with a QTc of 512 on cipro and they were still getting it because 'she’s not symptomatic.' i cried in the supply closet. someone please tell me i’m not the only one who sees this.