Medication Timing Calculator for Night Shift Workers
Medication Timing Calculator
Results
Key Information
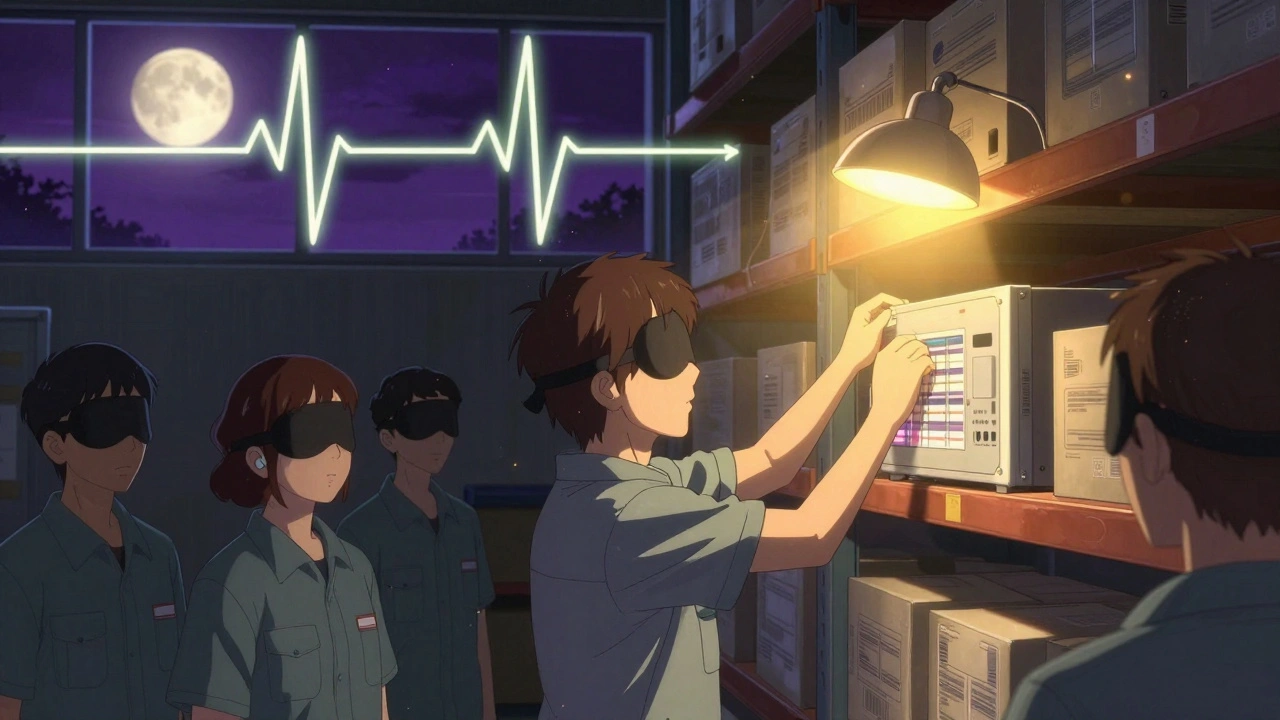
Working nights is hard on your body
When you work nights, your body fights you. Your brain is wired to sleep when it’s dark and be awake when it’s light. But if you’re on the night shift, you’re asking it to do the opposite - every single day. This mismatch is called shift work disorder. It’s not just feeling tired. It’s your internal clock out of sync with the world around you. And when you’re tired, mistakes happen. Accidents happen. People get hurt.
According to the CDC, about 10 million Americans work nights. That’s nurses, truck drivers, factory workers, emergency responders - people who keep things running when everyone else is asleep. But fatigue makes them 70% more likely to have a workplace accident. And if they’re driving home after a shift? The risk of a crash goes up even more.
Why people turn to sleep meds - and why it’s risky
Most night shift workers try to sleep during the day. But sunlight, noise, and family obligations make that hard. So they turn to sleep medications: Ambien, Lunesta, Sonata. These drugs help them fall asleep faster. But they don’t fix the root problem. They just mask it.
The FDA issued a strong warning in 2023: these drugs can cause people to do things while half-asleep - like driving, eating, or even leaving the house - without remembering it later. There were 66 reported cases of serious injuries from sleepwalking between 2019 and 2022. One nurse took zolpidem before her daytime nap, drove 15 miles in her sleep, and crashed into a fence. She had no memory of it.
And it gets worse. These medications stick around. Zolpidem can still affect you 8 hours after you take it. That means if you take it at 7 a.m. to sleep before your 11 p.m. shift, you might still be groggy at work. A 2022 study found 40% of people using zolpidem showed signs of next-shift impairment. That’s not just risky - it’s dangerous.
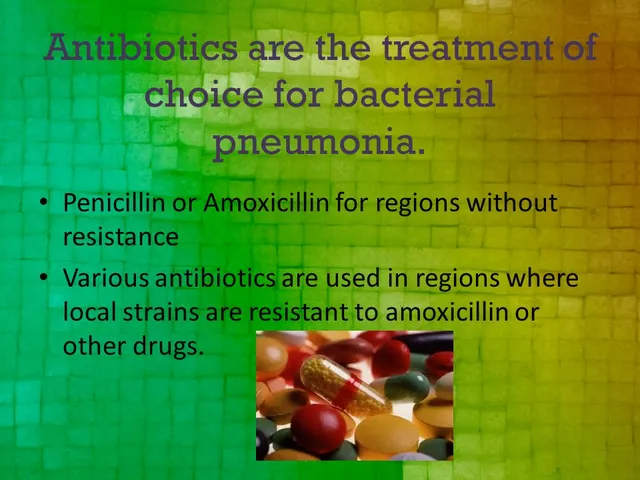
Wakefulness drugs aren’t magic either
Then there are the wakefulness-promoting drugs like modafinil and armodafinil. These are prescribed to help night shift workers stay alert. Modafinil is the most common. It’s used in hospitals, air traffic control, and long-haul trucking. Studies show it improves alertness by 34% compared to placebo. That sounds great - until you realize it still doesn’t bring you back to full daytime performance.
Modafinil lasts 12 to 15 hours. That means if you take it at 10 p.m. for your shift, it’s still in your system when you try to sleep at 7 a.m. You might fall asleep, but your sleep quality suffers. You don’t get deep, restorative sleep. You get fragmented, shallow rest. And over time, the effect fades. Truck drivers on forums report diminishing results after 3 to 4 weeks of daily use.
And here’s the catch: modafinil doesn’t fix your circadian rhythm. It just keeps you awake while your body screams for sleep. The American Academy of Sleep Medicine says no drug can fully restore your natural clock. That’s biology, not bad medicine.

Melatonin isn’t the miracle cure
Melatonin gets marketed as a natural sleep aid. It’s sold in every drugstore. But it’s not a sleeping pill. It’s a signal. Your body makes it naturally at night to tell you it’s time to sleep. Taking it as a supplement can help nudge your internal clock - if you take it at the right time.
Studies show melatonin works best when taken 3 to 4 hours before you want to sleep. So if you’re trying to sleep from 7 a.m. to 3 p.m., take it at 3 a.m. That’s not intuitive. Most people take it at bedtime - which is useless if your bedtime is 7 a.m. in the middle of the day.
And the data is mixed. The American Academy of Sleep Medicine says melatonin can help night workers sleep. But a 2022 Cochrane Review found the evidence was low-quality. It might help you fall asleep faster, but it doesn’t improve sleep quality or make you more alert at work. And it’s not regulated like prescription drugs. One bottle might have 1 mg. Another might have 5 mg. You don’t know what you’re really getting.
What you shouldn’t do
There are dangerous habits that seem harmless - until they aren’t.
- Don’t mix sleep meds with alcohol. The FDA says this can cause life-threatening breathing problems. Yet 15% of night shift workers admit to drinking while on sleep meds.
- Don’t take benzodiazepines long-term. Drugs like Xanax or Valium can become addictive after just 4 to 6 weeks. One in four users develops dependence.
- Don’t rely on OTC antihistamines. Diphenhydramine (Benadryl) and doxylamine (Unisom) are common. They cause drowsiness - but they also cause next-day grogginess, confusion, and memory problems. The FDA says 18% of users feel impaired the next day.
- Don’t skip the medication guide. Every prescription comes with a guide. Read it. Every time. The FDA requires it for a reason.
What actually works - without pills
The best solutions aren’t pills. They’re habits.
Darkness matters. Use blackout curtains. Wear blue-light-blocking glasses before bed. Cover your phone screen. Even small amounts of light can trick your brain into thinking it’s daytime. A 2023 study found night workers who used blackout shades slept 47 minutes longer on average.
Consistency matters. Try to sleep and wake at the same time every day - even on days off. Your body craves routine. If you sleep 8 a.m. to 4 p.m. on workdays but sleep midnight to 8 a.m. on weekends, your clock never stabilizes.
Light exposure helps. Get bright light during your night shift. Sunlight or special light therapy lamps can help reset your internal clock. Many hospitals now give workers portable light boxes. Some employers are starting to offer them as part of wellness programs.
Plan your meals. Don’t eat heavy meals right before sleep. Avoid caffeine 4 hours before your sleep window. Eat protein-rich snacks during your shift to stay alert, not sugar.
When to talk to your doctor
If you’re relying on sleep or wakefulness meds for more than a few weeks, it’s time to have a real conversation with your doctor. Tell them your exact schedule. Not “I work nights.” Say: “I work 11 p.m. to 7 a.m., three days a week. I take Ambien at 8 a.m. and feel groggy by 2 p.m.”
Doctors need this detail. A 2022 study found medical residents received less than 5 hours of formal training on sleep medication safety during their entire residency. Many don’t know the half-lives of these drugs. They prescribe based on habit, not science.
Ask your doctor:
- Is this medication right for my schedule?
- What’s the half-life? When will it wear off?
- Are there non-drug options I haven’t tried?
- Could this interact with other meds I take?
And if you’re already dependent - if you can’t sleep without it - say so. There are specialists in circadian rhythm disorders. They can help you wean off safely.
Real safety starts with planning
There’s no quick fix. But there’s a better way.
Companies with 24/7 operations are starting to implement fatigue management programs. That means scheduled naps, light therapy, and education - not just prescriptions. Sixty-eight percent of large hospitals now have formal safety protocols for shift workers. That’s up from 42% in 2020.
But if you’re on your own - whether you’re a nurse, a delivery driver, or a warehouse worker - you need to be your own advocate. Track your sleep. Note how you feel at work. If you’re nodding off at the wheel or making mistakes on the job, that’s not normal. It’s not weakness. It’s biology.
Medications can help in the short term. But they’re not a long-term solution. The real fix is aligning your life with your body’s rhythm - not fighting it with pills.
Start small. Block out your sleep time. Get the dark. Get the light. Talk to your doctor. And remember: staying safe isn’t about taking more drugs. It’s about understanding your body - and giving it what it really needs.



sagar bhute
December 3, 2025 AT 00:58Cindy Lopez
December 4, 2025 AT 12:03James Kerr
December 5, 2025 AT 07:49shalini vaishnav
December 6, 2025 AT 10:20bobby chandra
December 7, 2025 AT 17:14Archie singh
December 8, 2025 AT 20:52Albert Essel
December 9, 2025 AT 08:20Charles Moore
December 9, 2025 AT 15:25Gavin Boyne
December 10, 2025 AT 21:44