Dealing with bladder issues or urinary incontinence can be a huge hassle, but did you know physical therapy might just be your new best friend? It's all about using targeted exercises to get those pelvic muscles back into shape. We're talking about simple, non-invasive tricks to help you regain control.
Imagine this: being able to go through your day without constantly worrying about finding the nearest bathroom. Sounds pretty great, right? Physical therapy offers that kind of freedom. By focusing on strengthening the muscles supporting your bladder, it helps you manage those annoying leaks and urges.
So, why not give it a shot? After all, there’s nothing to lose and so much confidence to gain. It's time to explore how a few lifestyle tweaks and some guided exercises can make a real difference in your everyday life.
- Understanding Urinary Incontinence
- How Physical Therapy Can Help
- Exercises to Strengthen Pelvic Muscles
- Lifestyle Modifications for Better Bladder Control
- Success Stories and Real-Life Benefits
- Getting Started with Physical Therapy
Understanding Urinary Incontinence
Urinary incontinence is more common than you might think, affecting millions worldwide, and it's not just an issue for older adults. It's basically when you're unable to control your bladder, which can lead to leaks at the most inconvenient times. And let's be real, no one wants that added stress.
Types of Urinary Incontinence
First off, there are several types of urinary incontinence:
- Stress Incontinence: This happens during activities like coughing, sneezing, or exercising, when extra pressure is put on the bladder.
- Urge Incontinence: If you experience a sudden, intense urge to urinate followed by an involuntary loss of urine, that's urge incontinence. It's like your bladder doesn't give you enough warning.
- Overflow Incontinence: This is when the bladder doesn't empty completely, leading to a constant dribble of urine.
- Functional Incontinence: Physical or mental impairments can prevent reaching the toilet in time.
It's essential to recognize which type you might be dealing with, as it helps tailor the right treatment and physical therapy plan.
Causes and Risk Factors
The causes can vary widely. There could be weak pelvic floor muscles, nerve damage, certain medications, or even lifestyle factors like diet and weight that contribute to the problem. Pregnancy, aging, and menopause also play significant roles.
Want a quick snapshot? Here's a stat that's eye-opening: A study showed that around 1 in 3 women experience some form of urinary incontinence at some point. While less common, men struggle with it too, especially after prostate surgery.
The Impact on Daily Life
Beyond the physical struggle, it's equally about the emotional toll. It can be embarrassing, making social activities and even exercise sessions nerve-wracking. The fear of leaks can hold people back from living life to the fullest.
But hey, here's the good news—knowing the problem is the first step to solving it. With the right guidance and targeted physical therapy, it's entirely possible to manage and even overcome urinary incontinence substantially.
How Physical Therapy Can Help
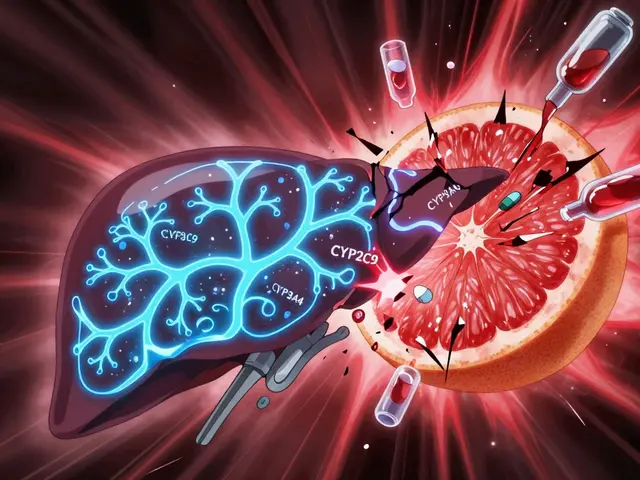
Physical therapy tackles urinary incontinence by working directly on the muscles responsible for bladder control. It's all about strengthening and retraining your pelvic muscles to do their job efficiently. Think of it like getting your body just a bit more aligned with its natural rhythm.
But how exactly does it work? Well, the core idea is to use targeted exercises that focus on the pelvic floor muscles. These exercises can help improve your bladder's ability to hold urine and reduce those sudden, uncontrollable urges to go. A lot of folks find this approach less daunting compared to medications or surgical options.
“Physical therapy should be the first step for anyone experiencing urinary incontinence. It offers a non-invasive and highly effective solution.” — Dr. Emily Harper, Renowned Urologist.
Why Choose Physical Therapy?
It's not just about strength exercises. Physical therapy involves a personalized approach where a trained therapist guides you through exercises and lifestyle adjustments. Techniques may include:
- Kegel exercises: These are the bread and butter of pelvic health. Basically, they involve tightening and relaxing the muscles you use to stop urination.
- Biofeedback: This helps you learn better control of those muscles. Think of it like watching your progress live; it’s pretty motivating!
- Bladder training: This strategy teaches your bladder to hold urine for longer periods, helping extend the time between bathroom visits.
A randomized study pointed out that nearly 70% of women experienced significant improvement in symptoms through a structured physical therapy program. That's a compelling reason to give it a go!
Seeing Real Improvements
Another cool thing? People not only see physical benefits, but there's often a boost in confidence too. Catching wind of exercise routines and therapy might not seem exciting at first, but reclaiming control over your bladder is empowering. Many people find that after a couple of months, their day-to-day life changes for the better.
Exercises to Strengthen Pelvic Muscles
When it comes to improving bladder health and tackling urinary incontinence, pelvic floor exercises, also known as Kegels, are a game changer. They’re simple, can be done almost anywhere, and make a big difference for many.
Getting Started with Kegels
First things first, you need to find the right muscles. An easy way to do this is to stop urination mid-flow. Those are the pelvic floor muscles. If you've found them, you're on the right path!
- Contract: Tighten those muscles for about 5 seconds.
- Release: Relax them for another 5 seconds. Congratulations, that's a basic Kegel exercise!
- Repeat: Try for 3 sets of 10 repetitions daily.
It's important to breathe normally and try not to tighten your abdomen, thighs, or buttocks. Focus on just the pelvic muscles.
Advanced Techniques
Once you're comfy with the basics, you can up the ante a bit:
- Increasing Time: Gradually increase the hold time to 10 seconds.
- Quick Clenches: Rapidly squeeze and release the muscles for 20 repetitions.
- Pilates or Yoga: Integrate these exercises, which often include pelvic floor strengthening, for an added boost.
Staying Consistent
Consistency is key. Mark your calendar or set an alarm as a daily reminder. Persistence with these exercises can significantly improve your bladder control over time.
Did you know studies suggest that up to 70% of people show improvements with regular Kegel exercises? That's right! No special equipment needed, just a bit of dedication and consistency, and you might notice a big change in how you handle bladder issues every day.

Lifestyle Modifications for Better Bladder Control
Sometimes, small tweaks in our daily routine can make a massive difference in managing urinary incontinence. Let’s dive into some lifestyle changes that could help you regain that much-needed control over your bladder.
Watch Your Fluid Intake
While it might seem logical to cut down on drinks if you're frequently rushing to the restroom, that's not always the best approach. Instead, aim for a steady intake of fluids spread throughout the day. This prevents your bladder from getting too full too quickly.
"Drinking the right amount of water keeps the urine diluted and scatters the risk of bladder irritation," says Dr. Emily Chambers, a urologist with over 20 years of experience.
Mind Your Diet
Your eating habits can impact bladder health too. Certain foods and drinks like caffeine, alcohol, spicy dishes, and citrus can trigger the bladder. Try cutting back on these to see if your symptoms improve.
Stay Active
Regular physical activity, even something as simple as daily walks, helps maintain a healthy weight and can reduce pressure on the bladder.
- Include a variety of exercises in your routine to support all-around bladder health.
- Pelvic floor exercises also known as Kegels, are essential to strengthen the muscles that support the bladder.
Set a Bathroom Schedule
Try to use the restroom at regular intervals instead of waiting until the last minute. This trains your bladder to get used to a routine and may decrease emergency trips.
Consider Professional Help
If you're still struggling, a consultation with a physical therapist could offer more personalized lifestyle recommendations.
Most importantly, don’t stress if these changes take time to work; consistency is key. You’re making genuine strides towards taking charge of your bladder health.
Success Stories and Real-Life Benefits
Let's face it, dealing with urinary incontinence isn't exactly battle gear for your confidence. But, what's undeniably true is the way physical therapy has turned lives around.
From Frustration to Freedom
Take Lisa, a 45-year-old from Manchester, who spent years planning her days around bathroom locations. After starting a physical therapy program, she found her quality of life took a noticeable turn for the better. Her therapist introduced her to specific pelvic floor exercises, and in just six weeks, she reported an 80% reduction in symptoms.
"I wish I'd started sooner. It's empowering to have control over my bladder again!" – Dr. Sarah Evans, specializing in physiotherapy, noted for her work with patients dealing with urinary incontinence.
Transformative Techniques
Many folks are surprised by how effective this approach really is. Strengthening pelvic muscles can often prevent leaks more successfully than just about anything else. Additionally, therapists often make small tweaks to drinking habits and lifestyle routines that pack a huge punch in managing symptoms.
- Tailored Exercise Programs
- Personalized Lifestyle Advice
- Regular Progress Tracking
Got stats? In a study carried out by the Royal College of Physicians in 2023, around 70% of participants reported significant improvement in their symptoms after a 12-week course of physical therapy.
A Brighter Outlook
The real gift here isn't just physical comfort. It's about restoring independence and dignity. So if you've been hesitating, think of those who've rediscovered their life sans constant bladder checks. They did it. You can too.
Getting Started with Physical Therapy
Taking the plunge into physical therapy for urinary incontinence can feel like a big step, but it’s really about piecing together a plan that fits your lifestyle and needs. The first move is to find a qualified therapist who specializes in pelvic health. You'll want someone who knows their stuff well enough to guide you effectively. A great place to start is checking out local clinics and reading reviews – people love sharing their experiences online.
Initial Consultation
Your first session is all about understanding what's going on and setting some goals. The therapist will chat with you about your symptoms, habits, and any exercises you’ve already tried. This is when you dig deep into the nitty-gritty of your bladder health. They'll likely assess your pelvic muscles to see how things are working down there.
Building a Personalized Plan
Once the therapist has a clear picture, they’ll whip up a customized plan. This plan usually includes exercises tailored to target specific muscles and improve your bladder control. Commonly, you'll practice Kegel exercises, which are pretty legendary for strengthening pelvic floors. These exercises involve squeezing and holding the same muscles you'd use to stop the flow of urine.
Regular Check-ins and Progress
Don’t expect overnight miracles; it’s about gradual progress. Regular sessions are key – most folks see their therapist once or twice a week to keep things moving along. These check-ins allow your therapist to track progress, tweak your routine if needed, and celebrate your wins with you.
- Consistency: Daily practice of assigned exercises is crucial. Treat it like brushing your teeth!
- Listen to Your Body: If something doesn’t feel right, tell your therapist. Adjustments can always be made.
- Stay Positive: Progress might be slow, but improvements will come.
So there you have it. With some commitment and a bit of patience, physical therapy can make a big difference. Before you know it, those annoying bladder issues will be a thing of the past, leaving you free to focus on what really matters – living your best life!




Naresh Sehgal
February 22, 2025 AT 21:42Stop letting bladder leaks dictate your life-grab the power of pelvic floor training now!
Commit to a daily routine and watch those embarrassing moments disappear.
Poppy Johnston
February 23, 2025 AT 08:49Hey Naresh, totally feel you-consistency is key, and it’s amazing how a few minutes a day can boost confidence big time.
Johnny VonGriz
February 23, 2025 AT 19:55Exactly, Poppy! The beauty of Kegel exercises lies in their simplicity and adaptability. Start with a set of 10 squeezes, holding each for five seconds, then rest for the same duration. Gradually increase both the count and hold time as your muscles strengthen. Remember to breathe normally and avoid engaging your abs or glutes-that ensures you target the correct muscles. Over a few weeks, many report a noticeable reduction in urgency and leakage.
Real Strategy PR
February 24, 2025 AT 07:02Let's be clear: ignoring pelvic health is a neglect of personal responsibility, and society shouldn't tolerate the excuse of "it's just aging". Take charge now, or you contribute to a culture of complacency.
Doug Clayton
February 24, 2025 AT 18:09I get it many people feel embarrassed about incontinence but the truth is it's more common than we think and you’re not alone
Michelle Zhao
February 25, 2025 AT 05:15Whilst the prevalence of urinary incontinence is indeed notable, one must question the incessant promotion of physical therapy as a panacea; perhaps alternative modalities merit equal consideration.
Eric Parsons
February 25, 2025 AT 16:22From a physiological standpoint, the pelvic floor functions as a supportive sling, and its integrity is crucial for bladder control. Engaging in targeted strengthening not only addresses symptoms but also fosters neuromuscular coordination, leading to lasting improvements.
Mary Magdalen
February 26, 2025 AT 03:29Don't be fooled by bland science-this is a battle for personal freedom, and embracing pelvic workouts is like arming yourself against the tyranny of leaks.
Dhakad rahul
February 26, 2025 AT 14:35आइए समझें कि शरीर का यह भाग केवल "इंस्ट्रक्टेड एक्सरसाइज़" नहीं, बल्कि एक राष्ट्रीय गर्व है-इसे सही ढंग से न समझना हमारे स्वास्थ्य की बेइज्जती है। 😤
William Dizon
February 27, 2025 AT 01:42Absolutely, Dhakad. Approaching pelvic health with both cultural respect and scientific rigor ensures we provide inclusive, effective guidance for everyone.
Jenae Bauer
February 27, 2025 AT 12:49Some say the whole pelvic floor craze is just a pharma ploy to sell gizmos, but maybe the truth lies somewhere between hype and genuine benefit.
vijay sainath
February 27, 2025 AT 23:55Look, Jenae, the data's out there-studies show 70% improvement rates, so stop feeding the nonsense and try the exercises.
Daisy canales
February 28, 2025 AT 11:02Sure, because doing nothing has always solved bladder problems in history
keyul prajapati
February 28, 2025 AT 22:09The relationship between lifestyle habits and pelvic floor health is often underestimated.
Research indicates that regular aerobic activity not only supports weight management but also reduces intra-abdominal pressure that can strain the bladder.
Incorporating mindful breathing techniques during exercise helps maintain proper core engagement without overactivating the pelvic muscles.
Hydration patterns play a pivotal role; consuming moderate amounts of water throughout the day prevents the bladder from becoming overdistended.
Conversely, excessive caffeine and alcohol intake can act as diuretics, prompting more frequent urges and potential leakage.
Dietary fiber is another silent ally, as it prevents constipation that can indirectly weaken pelvic floor support.
Simple adjustments, such as scheduling bathroom breaks every two to three hours, can train the bladder's capacity and reduce urgency.
Biofeedback devices offer real-time visual cues, enabling individuals to correct form and monitor progress effectively.
Consistency remains the cornerstone-performing a set of ten slow squeezes, holding for ten seconds, followed by a brief relaxation, twice daily yields measurable gains.
Over time, users often report enhanced confidence, allowing participation in social events without anxiety.
Moreover, the psychological uplift associated with regained control can improve overall quality of life.
It is essential to note that while pelvic exercises are beneficial, they should complement, not replace, medical evaluation when underlying pathologies exist.
Collaboration with a certified pelvic health therapist ensures personalized program design and safe progression.
Patients are encouraged to maintain a symptom journal, documenting triggers, fluid intake, and exercise adherence, to facilitate tailored adjustments.
In summary, a holistic approach that blends physical therapy, lifestyle modification, and ongoing monitoring offers the best odds for sustainable bladder mastery.
Embracing these strategies empowers individuals to reclaim autonomy over their bodies and daily routines.
Alice L
March 1, 2025 AT 09:15In consideration of cross‑cultural perspectives on pelvic health, it is incumbent upon clinicians to integrate both evidence‑based modalities and culturally sensitive communication to optimize patient adherence.
Seth Angel Chi
March 1, 2025 AT 20:22While formality impresses, the true measure lies in outcomes not ivory‑tower verbiage.