When you’re taking an SSRI for depression or anxiety and an NSAID for arthritis or a bad back, you might not think twice about combining them. After all, both are common, over-the-counter or prescription meds that millions use every day. But here’s the truth most people don’t know: SSRIs and NSAIDs together can double your risk of a dangerous gastrointestinal bleed - and it’s not just a small chance. It’s a real, measurable, and often overlooked danger.
Why This Combination Is So Dangerous
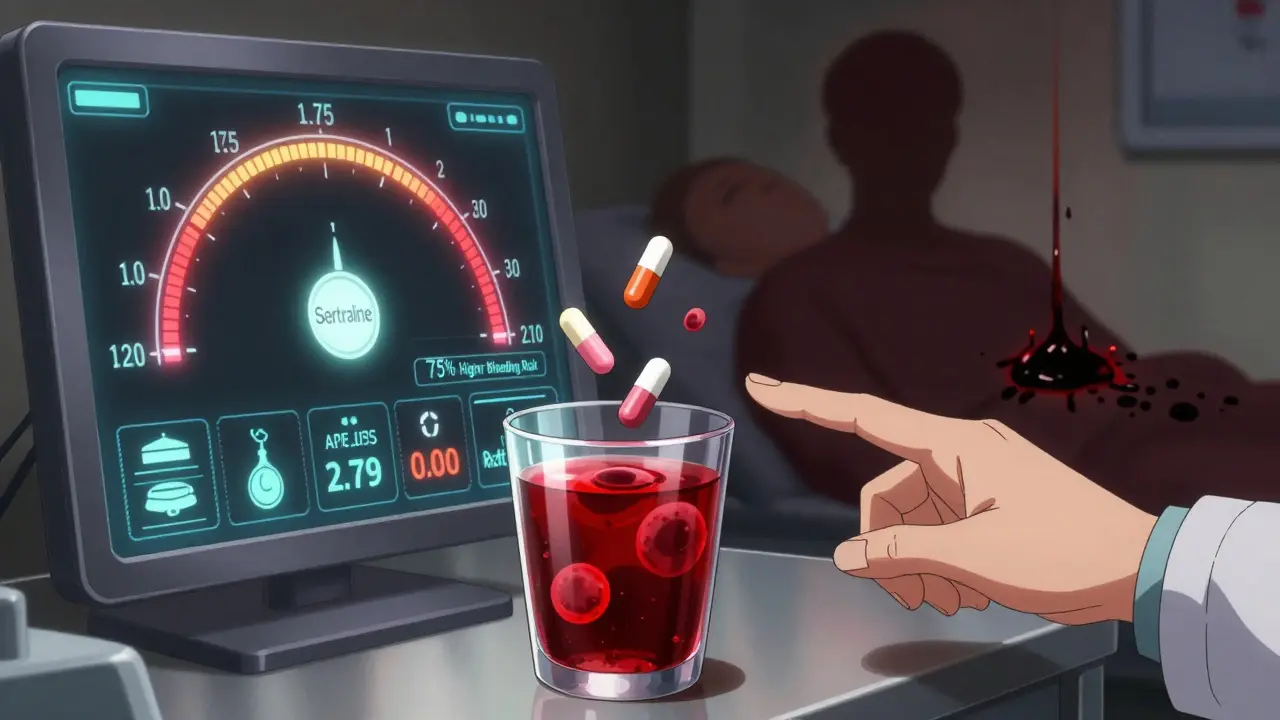
SSRIs - like sertraline, fluoxetine, and citalopram - work by boosting serotonin in your brain to improve mood. But serotonin isn’t just a brain chemical. It’s also critical for platelets, the blood cells that help stop bleeding. When SSRIs block serotonin reuptake into platelets, those cells can’t clump together properly when you get a cut or an ulcer starts to bleed. Your body’s first-line defense is weakened. NSAIDs - think ibuprofen, naproxen, diclofenac - hurt your stomach lining in a different way. They block COX-1, an enzyme that makes prostaglandins. Those prostaglandins are like a protective coating for your stomach and intestines. Without them, your gut lining gets thin, dry, and vulnerable. Acid eats away at it. Small ulcers form. And if your platelets aren’t working right because of the SSRI? That ulcer doesn’t heal. It bleeds. Put them together, and it’s not just 1 + 1 = 2. It’s more like 1 × 2.75. A 2023 meta-analysis in Digestive Diseases and Sciences confirmed what earlier studies found: using both drugs at the same time raises your risk of upper GI bleeding by 75%. That’s not a typo. That’s odds ratio 1.75. For someone over 65 with a history of ulcers, that could mean going from a 1% annual risk to over 2.5% - a huge jump for a problem that can land you in the ER with black, tarry stools or vomiting blood.Not All SSRIs or NSAIDs Are Created Equal
You might assume all SSRIs carry the same risk. They mostly do - because they all interfere with platelet serotonin. But some data suggests escitalopram might be slightly less risky than fluvoxamine or paroxetine. Still, the difference is small enough that you shouldn’t assume one is “safe.” NSAIDs? Big differences here. Ibuprofen has the lowest GI bleeding risk among non-selective NSAIDs. Naproxen and diclofenac? Much worse. And then there’s celecoxib - a COX-2 inhibitor. It doesn’t mess with the protective prostaglandins in your stomach the same way. Studies show its bleeding risk is close to baseline - odds ratio of just 1.16. For someone who needs long-term pain relief and is on an SSRI, celecoxib is often the smarter pick. But here’s the catch: celecoxib isn’t perfect. It’s more expensive. And if you have heart disease, it might not be the right choice. That’s why the decision isn’t just about picking the “safest” drug - it’s about matching the right drug to the right person.Who’s at the Highest Risk?
Not everyone who takes both drugs will bleed. But some people are sitting on a ticking clock:- People over 65 - stomach lining thins with age, healing slows, and kidney function drops, making NSAIDs harder to clear.
- Those with a past ulcer or GI bleed - once you’ve had one, your risk jumps again.
- People on blood thinners like warfarin or aspirin - adding SSRIs and NSAIDs on top? That’s a triple threat.
- Those with H. pylori infection - this bacteria causes ulcers. If it’s still active, NSAIDs and SSRIs turn it into a bleeding hotspot.
- Heavy drinkers or smokers - alcohol and tobacco further damage the gut lining.
What You Can Do - Step by Step
You don’t have to choose between pain relief and mental health. But you do need a plan.- Ask if you really need both. Can you switch from NSAIDs to acetaminophen (Tylenol)? It doesn’t hurt your stomach. For depression, is bupropion (Wellbutrin) an option? It doesn’t affect platelets. That’s a game-changer.
- If you need both, get a PPI. Proton pump inhibitors - like omeprazole, esomeprazole, or pantoprazole - are the gold standard for protection. Studies show they cut the extra bleeding risk from SSRIs and NSAIDs by about 70%. Take 20mg daily. Not just when you feel pain. Daily. Like a shield.
- Test for H. pylori. If you’ve had an ulcer before or are over 50, ask for a breath or stool test. Eradicate the infection before starting long-term therapy. It’s simple, cheap, and prevents future problems.
- Use the lowest dose for the shortest time. No need to take 800mg of ibuprofen three times a day if 400mg once a day works. Don’t keep NSAIDs on your nightstand “just in case.”
- Know the warning signs. Black, sticky stools. Vomiting blood or coffee-ground-looking material. Dizziness, weakness, rapid heartbeat. These aren’t “just indigestion.” Call your doctor or go to urgent care immediately.
Real Stories - What Happens When No One Warns You
On Reddit, someone wrote: “Took sertraline and ibuprofen for months. Started having black stools. Thought it was my diet. Three days later, I passed out in the bathroom. They found a bleeding ulcer. I was in the hospital for a week.” Another user on Drugs.com shared: “Switched from naproxen to celecoxib, added omeprazole, kept sertraline. No issues for 18 months. My doctor didn’t even mention the risk - I read it online myself.” A 2022 Medscape survey found 68% of patients weren’t warned about this interaction. That’s not negligence - it’s ignorance. And it’s preventable.
What’s Changing - And What’s Coming
Hospitals like Cleveland Clinic started adding automated alerts in their electronic records in 2019. Since then, GI bleed admissions in dual-therapy patients dropped 42%. That’s proof systems work. The FDA and EMA added warnings to SSRI labels years ago. But warnings on a pill bottle don’t help if your doctor doesn’t know. New research is pointing to personalized solutions. Some people have genetic variants (CYP2C19) that make PPIs less effective. Others have genes that make them metabolize SSRIs slower. Soon, a simple genetic test could tell your doctor exactly how much protection you need. And new drugs are coming. One company is testing a pill that combines ibuprofen with omeprazole in a single capsule - timed release, so the protective agent kicks in before the NSAID hits your stomach. Phase III trials are promising.The Bottom Line
You don’t have to suffer in pain. And you don’t have to feel depressed. But you can’t ignore the risk when you take both SSRIs and NSAIDs. The science is clear. The tools to prevent bleeding are proven. The problem isn’t the meds - it’s the lack of awareness. If you’re on both, talk to your doctor. Ask: “Do I need both? Can I switch to something safer? Should I be on a PPI?” Don’t wait for black stools. Don’t assume it’s just heartburn. This isn’t a rare side effect. It’s a common, preventable emergency. Your stomach doesn’t scream before it bleeds. But your doctor can help you hear the warning - if you ask.Can I take ibuprofen with an SSRI like sertraline?
You can, but it’s risky. Combining ibuprofen with an SSRI increases your chance of upper GI bleeding by about 75%. If you need pain relief, talk to your doctor about switching to acetaminophen or using celecoxib instead. If you must take both, always take a proton pump inhibitor (PPI) like omeprazole daily to protect your stomach lining.
Are all SSRIs equally risky for GI bleeding?
Most SSRIs carry similar risk because they all interfere with platelet serotonin. Some studies suggest escitalopram may be slightly less risky than fluvoxamine or paroxetine, but the difference is small. Don’t assume one SSRI is safe just because it’s newer or marketed as “gentler.” All SSRIs affect platelet function.
What’s the safest NSAID to take with an SSRI?
Celecoxib (Celebrex) is the safest NSAID option for people on SSRIs. It doesn’t block COX-1 in the stomach like traditional NSAIDs do, so it doesn’t reduce protective prostaglandins. Its GI bleeding risk is close to normal - odds ratio of 1.16. Ibuprofen is the least risky among non-selective NSAIDs, but still carries higher risk than celecoxib.
Do I need a proton pump inhibitor if I’m on both drugs?
Yes - if you’re taking both an SSRI and an NSAID long-term, you should be on a PPI. Studies show PPIs reduce the extra bleeding risk by about 70%. Omeprazole 20mg daily is standard. Don’t wait for symptoms. Prevention is far safer than treating a bleed.
Can I stop my SSRI to avoid the risk?
Never stop an SSRI suddenly. That can cause withdrawal symptoms or worsen depression. Instead, talk to your doctor about alternatives. Bupropion (Wellbutrin) is an antidepressant that doesn’t affect platelets and may be a better fit if you need long-term NSAID use. Switching medications should always be done under medical supervision.
How do I know if I’m having a GI bleed?
Watch for black, tarry, sticky stools (melena), vomiting blood or material that looks like coffee grounds, dizziness, rapid heartbeat, or sudden weakness. These are signs of active bleeding. Don’t wait. Go to urgent care or the ER immediately. GI bleeds can become life-threatening fast.
Is this interaction only a problem in older adults?
No - while older adults (65+) are at highest risk due to thinner stomach lining and slower healing, younger people with ulcers, H. pylori, or other risk factors like smoking or alcohol use can also bleed. Anyone taking both drugs long-term should be evaluated for protection, regardless of age.
Can I use natural remedies instead of NSAIDs?
Some people find relief with turmeric, ginger, or acupuncture for mild pain. But these aren’t proven substitutes for moderate to severe inflammation or chronic conditions like arthritis. If your pain is significant enough to need NSAIDs, natural options likely won’t cut it. Don’t trade one risk for another - talk to your doctor about safer pharmaceutical alternatives instead.







Joy F
January 4, 2026 AT 18:20Okay, but let’s be real - this isn’t just about pharmacology. It’s about how medicine has become a corporate casino where your gut is the house edge. SSRIs and NSAIDs? Two perfectly legal drugs that, when combined, turn your digestive tract into a warzone. And who pays? You. The patient. The one who trusts the system. The one who doesn’t read the tiny print on the pill bottle because they’re too exhausted from surviving capitalism to care. We’re not talking about rare side effects here. We’re talking about systemic negligence dressed up as ‘standard care.’ And no, PPIs aren’t a fix - they’re a Band-Aid on a severed artery.
They’ll sell you omeprazole like it’s holy water while the real problem - profit-driven prescribing - goes unchallenged. Tell me again why we trust doctors who don’t even screen for this interaction? Because they’re busy chasing KPIs, not saving lives.
And don’t even get me started on celecoxib. Sure, it’s ‘safer.’ But it’s also 3x the price. So now your survival depends on your credit score. Brilliant. Just brilliant.
We need to stop treating symptoms and start dismantling the system that turns medicine into a lottery where your intestines are the losing ticket.
Palesa Makuru
January 4, 2026 AT 23:58Y’all in the US are so dramatic. In South Africa, we just take ibuprofen with our antidepressants and pray to ancestors. No PPIs. No fancy tests. Just vibes. If you’re bleeding, maybe you weren’t meant to survive anyway. 🙃
Also, who even has money for celecoxib? My doctor gave me aspirin and told me to ‘drink more water.’ That’s the real healthcare system - no alerts, no guidelines, just survival.
Lori Jackson
January 5, 2026 AT 16:40Oh please. You’re all acting like this is some groundbreaking revelation. This interaction has been documented since the early 2000s. The FDA warned about it in 2006. The British Medical Journal published a meta-analysis in 2011. Yet here we are, 2025, and people are still acting shocked? It’s not ignorance - it’s willful neglect. You want to live in a fantasy world where drugs are harmless? Fine. But don’t act like you’re the victim when your stomach starts hemorrhaging because you refused to read the damn label.
And yes, bupropion is an option. But you’d rather keep your SSRI because ‘it works’ - even if it’s slowly turning your gut into a crater. Priorities.
Sarah Little
January 7, 2026 AT 02:52I’ve been on sertraline for 8 years and naproxen for 5. No PPI. No issues. Maybe I’m just lucky? Or maybe the stats are exaggerated? I don’t know. But I’m not about to start taking omeprazole daily like it’s a vitamin just because some article scared me. My body’s fine. Why fix what isn’t broken?
innocent massawe
January 9, 2026 AT 00:07Thank you for this. In Nigeria, many people don’t even know SSRIs can affect bleeding. We think depression is just ‘bad thoughts.’ I showed this to my cousin - she was on fluoxetine and diclofenac. She’s now seeing a doctor for a PPI. 🙏
Knowledge is power. Even in places with no alerts, we can still save each other.
erica yabut
January 9, 2026 AT 21:33Let me be the ugly truth-teller here: if you’re taking both drugs and not on a PPI, you’re not ‘managing your health’ - you’re gambling with your organs. And if you think ‘I feel fine’ means you’re safe, you’re the kind of person who texts while driving and says ‘I’ve never had an accident.’
Acetaminophen? Sure. But if you’re still clinging to NSAIDs like they’re your emotional support painkiller, you’re not a patient - you’re a walking clinical trial. And your gut? It’s the lab rat.
Stop romanticizing suffering. Your ‘I’m fine’ is just denial with a side of caffeine.
Vincent Sunio
January 11, 2026 AT 10:08While the article presents a compelling clinical narrative, it exhibits a nontrivial degree of rhetorical hyperbole. The odds ratio of 1.75, while statistically significant, does not equate to a ‘skyrocketing’ risk in absolute terms. For a low-risk individual, the absolute increase in bleeding probability remains negligible. Furthermore, the conflation of ‘risk’ with ‘inevitability’ is a logical fallacy frequently employed in medical sensationalism.
Moreover, the recommendation to universally prescribe PPIs to all dual-therapy patients ignores the documented risks of long-term proton pump inhibitor use - including micronutrient deficiencies, increased susceptibility to C. difficile, and potential rebound acid hypersecretion. A risk-benefit analysis is not a checklist. It is a nuanced, individualized clinical judgment - not a one-size-fits-all directive.
Finally, the anecdotal Reddit and Drugs.com testimonials are not evidence. They are anecdata. The scientific method requires controlled studies, not emotional narratives.
Haley Parizo
January 13, 2026 AT 09:22This isn’t just about drugs. It’s about how we’ve turned healing into a transaction. We treat depression like a software bug to be patched with serotonin. We treat chronic pain like a mechanical glitch to be silenced with NSAIDs. And when the system breaks - when your stomach starts bleeding - we hand you a PPI like it’s a free app update.
But your body isn’t a phone. You can’t just reboot it. You can’t just ‘update’ your biology.
We need to stop treating symptoms and start asking why we’re so dependent on these drugs in the first place. Why is chronic pain so common? Why is depression so widespread? Is it just chemical imbalance - or is it a society that’s broken?
Maybe the real prescription isn’t omeprazole. Maybe it’s community. Maybe it’s rest. Maybe it’s not being forced to work 80-hour weeks while your body screams for help.
But no - we’d rather sell you a pill. Again.
Angela Fisher
January 15, 2026 AT 06:55They don’t want you to know this. The pharmaceutical companies, the FDA, the doctors - they’re all in on it. PPIs? They’re not protecting you. They’re keeping you hooked. Omeprazole? It’s a gateway drug to lifelong dependency. And celecoxib? It’s a Trojan horse. They’re pushing it so you’ll stay on the NSAID longer - because the real profit is in the combo. You think they care about your gut? No. They care about your monthly refill. The ‘75% increased risk’? That’s a scare tactic to sell more PPIs. The real danger is the system. They’re turning healthy people into patients. I’ve seen it. My cousin’s doctor gave her 5 different pills for ‘side effects’ of the first pill. Now she’s on 12. And she’s 32. This isn’t medicine. It’s a pyramid scheme with stethoscopes. 🤡💊