Hepatorenal Syndrome: A Clear Overview
When dealing with hepatorenal syndrome, a functional kidney failure that develops in people with advanced liver disease. Also known as HRS, it often signals a critical turning point for patients.
HRS doesn’t appear in isolation. It usually follows liver cirrhosis, the scarring of liver tissue that impairs blood flow and detoxification. In the same breath, clinicians watch for acute kidney injury, a rapid loss of kidney function that can be triggered by many insults, including severe liver disease. The link between these conditions forms a dangerous cascade: as the liver falters, the kidneys receive less blood, and waste builds up.
Key Concepts and Treatment Options
The main driver behind HRS is portal hypertension, elevated pressure in the portal vein caused by scarred liver tissue. This pressure pushes fluid into the abdomen (ascites) and squeezes blood away from the kidneys. The body reacts by tightening blood vessels (vasoconstriction) to keep blood pressure up, but that response harms the kidneys further. In short, hepatorenal syndrome encompasses renal dysfunction caused by liver failure, while portal hypertension fuels the underlying fluid shifts.
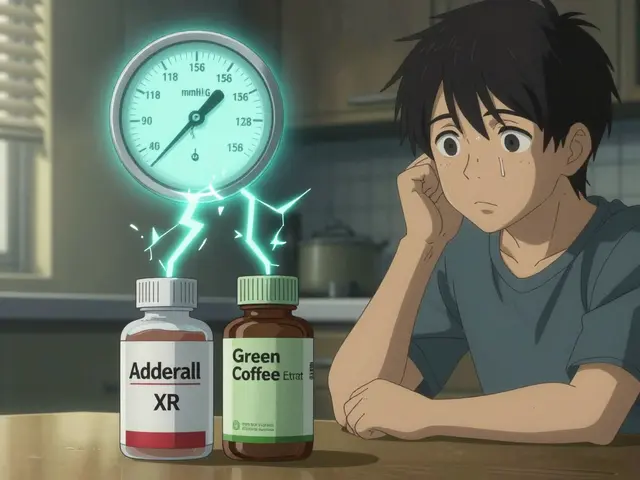
Effective therapy targets both the hemodynamic imbalance and the underlying liver disease. One of the most proven approaches uses a vasoconstrictor called terlipressin, a synthetic analogue of vasopressin that narrows blood vessels in the splanchnic circulation. By reducing portal pressure, terlipressin helps restore kidney perfusion. It’s typically paired with intravenous albumin, which expands blood volume and supports circulation. Together, these agents illustrate how “treatment often requires vasoconstrictor therapy such as terlipressin” (subject‑predicate‑object).
Beyond drugs, managing HRS means addressing the root cause: the liver. Reducing ascites with diuretics, limiting sodium intake, and treating infections promptly (antibiotics like cefaclor or rifaximin) can halt the vicious cycle. When medical therapy fails, renal replacement techniques—dialysis or even liver transplantation—become necessary. Patients and caregivers should monitor urine output, serum creatinine, and blood pressure closely, as early detection of worsening kidney function improves outcomes.
Now that you see how liver cirrhosis, portal hypertension, and acute kidney injury intertwine, you’ll recognize the rationale behind the medication guides and treatment tips in the articles below. Below you’ll find detailed comparisons of antibiotics, diuretics, and vasoconstrictor regimens, all aimed at helping you manage the complex landscape of hepatorenal syndrome.

How Liver Failure Affects the Urinary System - Symptoms, Risks & Management
Explore how liver failure disrupts kidney function and bladder health, recognize warning signs, and learn treatment steps to protect your urinary system.
Detail