Opioid Metabolism: Key Factors & Clinical Insights
When talking about Opioid Metabolism, the process by which the body breaks down opioid compounds. Also called opioid processing, it determines how long a painkiller lasts, how strong its effect is, and how likely side‑effects become. Understanding this pathway is the first step to safer prescribing and better pain control.
The core drivers of opioid metabolism are CYP450 enzymes, a family of liver proteins that chemically modify drugs. Enzymes like CYP3A4, CYP2D6, and CYP2B6 each handle specific opioids, turning them into active metabolites or inactive forms. When one of these enzymes works faster, the drug may wear off quickly; when it works slower, the patient can experience prolonged sedation or respiratory depression. This direct link creates the semantic triple: Opioid metabolism encompasses CYP450 enzyme activity.
But enzymes don’t act in isolation. Liver function, the organ’s overall health and capacity to process chemicals, sets the stage for how efficiently those enzymes operate. Liver disease, hepatitis, or fatty liver can cut enzyme output by half, meaning the same opioid dose can linger in the bloodstream much longer. This relationship forms another triple: Liver function determines the rate of opioid clearance.
Genetic makeup adds a third layer. Genetic polymorphisms, variations in DNA that alter enzyme structure and activity, explain why two patients on the same prescription can have opposite experiences. A person with a CYP2D6 ultra‑rapid metabolizer genotype may convert codeine to morphine very quickly, risking toxicity, while a poor metabolizer sees little pain relief. Here we see the triple: Genetic polymorphisms influence opioid metabolism.
Why Drug Interactions Matter
Beyond the body’s own chemistry, other drugs can hijack the same enzymes. Drug interactions, the way two or more medications affect each other's metabolism, can either boost or block opioid breakdown. For example, a strong CYP3A4 inhibitor like ketoconazole can raise plasma levels of oxycodone, while a CYP3A4 inducer such as carbamazepine can make the same dose feel weak. This creates the triple: Drug interactions alter opioid metabolism.
Clinicians use this knowledge daily. When a patient starts a new antifungal or anticonvulsant, the prescriber checks whether the drug is a known CYP450 inhibitor or inducer before adjusting opioid doses. In practice, this means reviewing medication lists, checking liver function tests, and sometimes ordering pharmacogenetic panels to spot risky polymorphisms. The goal is to keep pain relief effective while avoiding overdose or withdrawal.
Real‑world cases illustrate the impact. A middle‑aged man with chronic back pain on morphine experienced sudden drowsiness after beginning a course of erythromycin; the antibiotic inhibited CYP3A4, slowing morphine clearance. Another patient with severe liver cirrhosis required a lower starting dose of fentanyl because his compromised liver couldn’t support normal enzyme activity. Both scenarios highlight how the three pillars—enzymes, liver health, genetics—interact with external drugs to shape outcomes.
Practical steps for patients and providers include: 1) always share the full medication list, including over‑the‑counter supplements; 2) get routine liver function labs when on long‑term opioids; 3) consider a pharmacogenetic test if dose adjustments feel unpredictable; and 4) monitor for signs of under‑ or over‑medication, such as increased pain, sedation, or respiratory struggles. These actions turn abstract concepts into everyday safety measures.
The collection of articles below dives deeper into each of these topics. You’ll find guides on specific drug‑opioid combos, breakdowns of how different CYP450 enzymes handle each opioid, and tips for managing pain in patients with liver disease or unique genetic profiles. Armed with this background, you’ll be ready to navigate the complexities of opioid metabolism and make informed choices for better health outcomes.
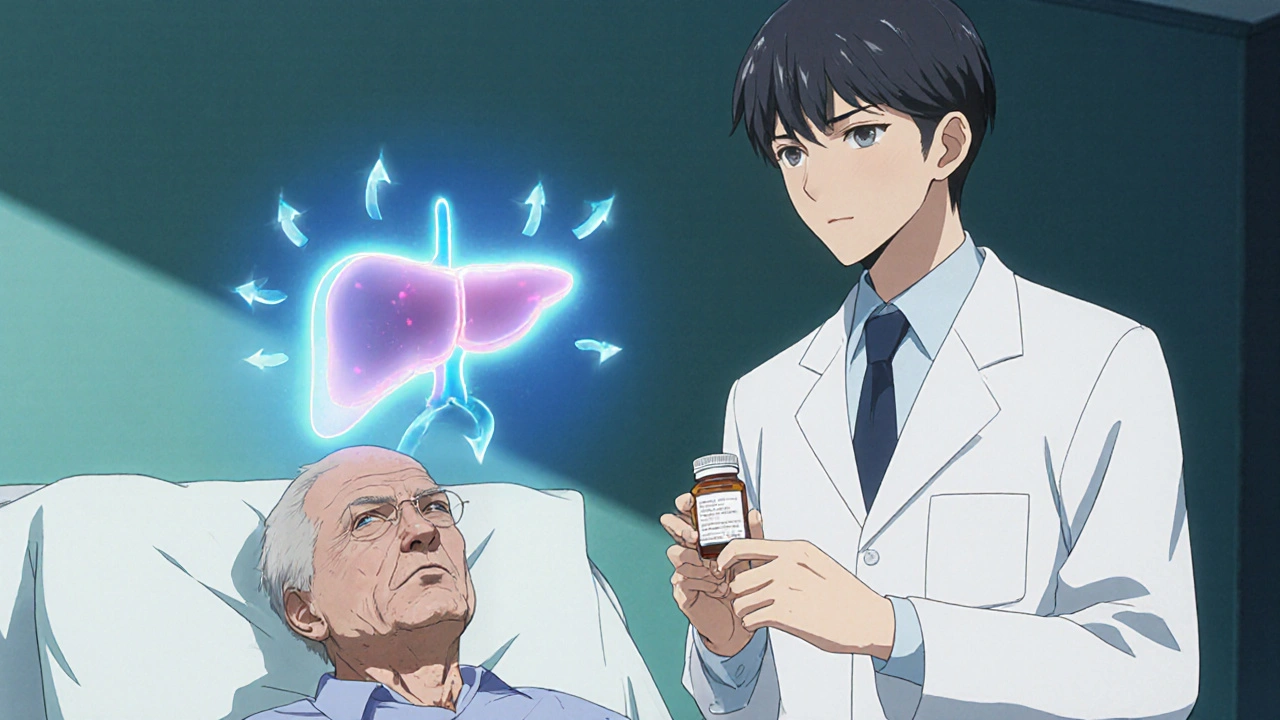
Opioids & Liver Disease: Metabolism, Accumulation, and Side Effects
Learn how liver disease changes opioid metabolism, causes drug accumulation, and heightens side effects. Get dosing tips, safety checklists, and a quick reference table.
Detail