Amiodarone-Digoxin-Warfarin Triad Checker
Check for Dangerous Drug Combination
This tool identifies if you're taking the potentially deadly combination of amiodarone, digoxin, and warfarin - known as the "dangerous drug triad."
Three drugs. One deadly combo. If you’re on amiodarone for an irregular heartbeat, and you’re also taking digoxin to slow your heart rate or warfarin to prevent clots, you’re in a high-risk zone - and most people don’t realize it until it’s too late.
This isn’t theoretical. In 2022, the FDA recorded 387 deaths linked to the combination of amiodarone, digoxin, and warfarin. That’s not a glitch. It’s a pattern. And it’s happening in hospitals, nursing homes, and living rooms across the country - especially in older adults with atrial fibrillation, the most common heart rhythm disorder in people over 65.
Why This Triad Is So Dangerous
Amiodarone doesn’t just sit there. It messes with how your body handles other drugs. It’s like a wrecking ball in your liver and kidneys. When you take amiodarone with digoxin, your digoxin levels can spike by up to 100% within just a few days. That’s not a small bump - that’s the difference between a safe dose and a toxic one.
Digoxin toxicity doesn’t sneak up. It hits hard: nausea, vomiting, blurry yellow vision, dizziness, and worst of all - dangerous heart rhythms like ventricular tachycardia. One study found that 67% of patients on this combo developed nausea, and 22% reported visual disturbances. These aren’t side effects you can ignore. They’re warning signs.
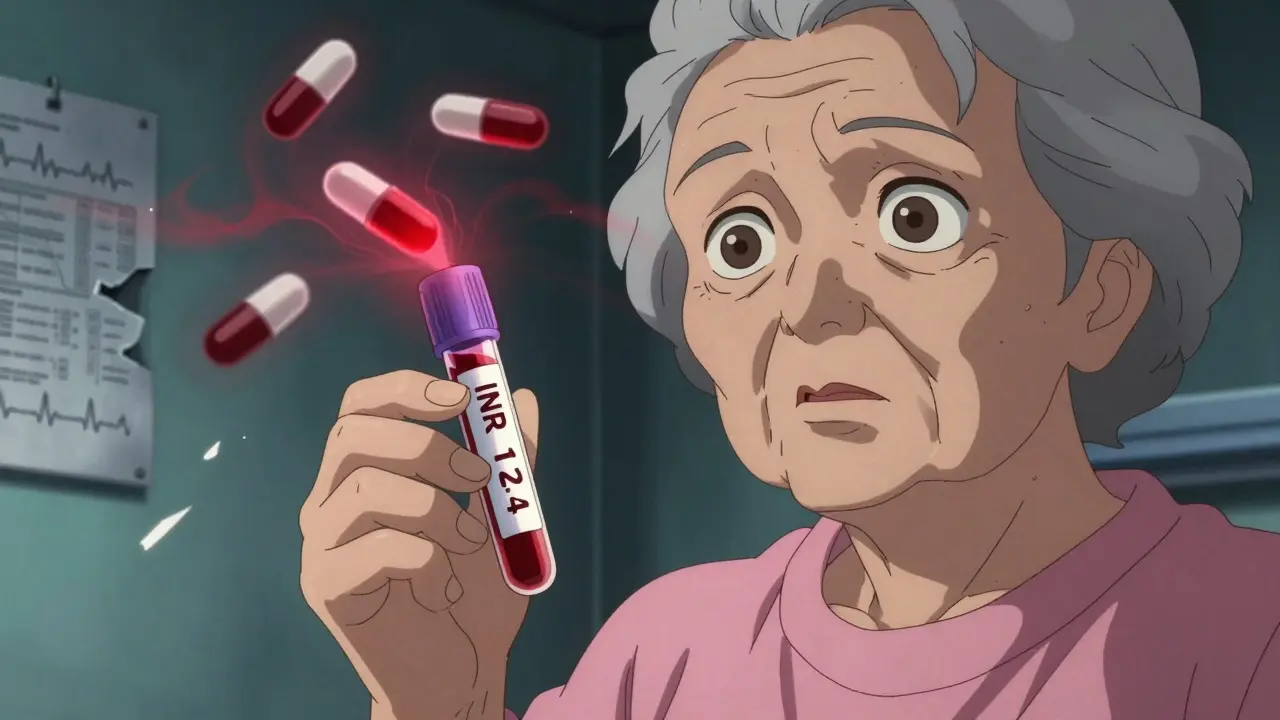
Then there’s warfarin. Amiodarone doesn’t just boost digoxin - it also makes warfarin way more powerful. It blocks the enzymes (CYP2C9 and CYP3A4) that break down warfarin. That means your blood thins way more than expected. INR levels - the measure of how long your blood takes to clot - can jump from a safe 2.5 to over 10 in under two weeks. An INR above 4.0 means bleeding risk skyrockets. Above 6.0? You’re in emergency territory.
And here’s the kicker: this interaction doesn’t go away when you stop amiodarone. Because amiodarone sticks around in your fat and tissues for weeks - sometimes months - your body keeps processing warfarin and digoxin like it’s still getting a full dose. So even if you quit amiodarone, your doctor still needs to monitor you for 4 to 6 weeks.
How the Interaction Actually Works
It’s not magic. It’s biology. Amiodarone is a big, bulky molecule that lingers in your body for up to 100 days. That’s longer than most medications stay around. And it doesn’t just affect one pathway - it hits multiple.
For digoxin: Amiodarone blocks P-glycoprotein, the protein that normally pumps digoxin out of your cells. When that pump gets blocked, digoxin builds up in your blood. Your kidneys can’t clear it fast enough. Even if you’re taking the same dose you’ve been on for years, your body suddenly starts overdosing.
For warfarin: Amiodarone and its metabolite, desethylamiodarone, shut down CYP2C9 - the main enzyme that breaks down the more potent form of warfarin (S-warfarin). That means your body can’t clear warfarin the way it used to. Your INR creeps up. You start bruising easily. Maybe you have a nosebleed that won’t stop. Then comes the real fear: bleeding in the brain.
And it gets worse. Digoxin itself can push warfarin off protein-binding sites in your blood, freeing up even more active warfarin. So it’s not just one interaction - it’s a chain reaction. Three drugs. Two mechanisms. One explosive outcome.
Who’s Most at Risk?
This isn’t just about taking the wrong pills. It’s about who you are.
People over 75 are at the highest risk. Their kidneys don’t clear drugs as well. Their livers slow down. They’re more likely to be on multiple medications. And they’re more sensitive to digoxin - levels above 1.2 ng/mL can be toxic in older adults, while younger people might tolerate up to 2.0 ng/mL.
Women, especially those with low body weight, are more vulnerable. So are people with kidney disease, hypothyroidism, or electrolyte imbalances like low potassium or magnesium - all common in heart failure patients.
And let’s not forget: this combo is still prescribed. Even though direct oral anticoagulants (DOACs) like apixaban and rivaroxaban have replaced warfarin in 82% of new atrial fibrillation cases since 2022, millions of people are still on warfarin. Why? Because they have mechanical heart valves, can’t afford DOACs, or have been on warfarin for decades and their doctor hasn’t switched them.
According to the American Heart Association, 4.3 million Americans will still need this risky trio through 2030. That’s not a small number. That’s a public health blind spot.
What Doctors Should Do - And Often Don’t
There are clear guidelines. The American College of Cardiology says: if you’re starting amiodarone on someone already taking digoxin and warfarin, you must act - immediately.
- Reduce the digoxin dose by 50% before or right when you start amiodarone.
- Check serum digoxin levels 72 hours after starting amiodarone - not in a week, not next month. Three days.
- Lower the warfarin dose by 30-50% before starting amiodarone.
- Check INR every 48-72 hours for the first two weeks. Then weekly until stable.
- Keep checking INR for at least 4 weeks after stopping amiodarone.
Yet a 2022 JAMA Internal Medicine study found that in 68% of cases, these steps weren’t followed. Why? Because many doctors don’t know. Or they assume the patient’s current doses are “fine.” Or they think, “It’s been years since I saw this problem.”
One cardiologist from Massachusetts General Hospital shared a case on Reddit: a 78-year-old man with atrial fibrillation, INR 12.4 after 10 days of amiodarone. He was bleeding internally. Needed 4 units of fresh frozen plasma and IV vitamin K. He survived - barely.
That’s not rare. The FDA’s adverse event database shows 1,842 reports of digoxin toxicity with amiodarone between 2010 and 2022. That’s a 5.3 times higher risk than with digoxin alone.
What You Can Do - Even If You’re Not a Doctor
You don’t need a medical degree to protect yourself or a loved one.
- Know your meds. Write down every pill you take - including over-the-counter and supplements.
- Ask your pharmacist: “Are these drugs safe to take together?” They see this combo all the time.
- Track your symptoms. Nausea? Blurry vision? Unusual bruising? Bleeding gums? Nosebleeds that won’t stop? Tell your doctor immediately.
- Ask for a digoxin blood test and INR check right after starting amiodarone - don’t wait for your next routine visit.
- If your doctor says, “We’ll just watch,” push back. Say: “I’ve read this combo can be deadly. Can we test my levels in 72 hours?”
And if you’re on warfarin and your doctor suggests switching to amiodarone? Ask: “Is there a safer alternative? Could we use a DOAC instead?” Many people don’t realize DOACs don’t interact with amiodarone the same way warfarin does.
The Bigger Picture: Why This Keeps Happening
This isn’t just about three drugs. It’s about how medicine works.
We treat symptoms - not systems. We fix atrial fibrillation with amiodarone. We slow the heart with digoxin. We prevent strokes with warfarin. But we rarely step back and ask: “What happens when all these drugs collide?”
Electronic health records now flag this interaction - and hospitals that use them have cut errors by 65%. But not all clinics do. Not all pharmacies alert patients. Not all doctors get updated training.
And the aging population? It’s only getting worse. More people are living longer with multiple chronic conditions. More polypharmacy. More chances for this triad to slip through.
That’s why this isn’t just a pharmacology lesson. It’s a survival skill.
What’s Changing - And What’s Not
The good news? DOACs are replacing warfarin in most new cases. That means fewer people will face this exact triad going forward.
But here’s the catch: amiodarone still interacts with DOACs like dabigatran. It blocks P-glycoprotein, which helps clear those drugs too. So even if you switch from warfarin, you’re not out of the woods.
And digoxin? Still widely used. Despite newer drugs like ivabradine and beta-blockers being safer for rate control, digoxin remains common - especially in elderly patients with heart failure.
So this triad isn’t going away. Not yet.
What’s changing is awareness. The 2023 FDA Drug Safety Communication upgraded the warning to a “Black Box” - the strongest possible. That means manufacturers must put it on the label in bold letters. But labels don’t save lives. People do.
If you’re on any of these three drugs - or you’re caring for someone who is - don’t assume it’s safe. Don’t wait for symptoms. Ask for tests. Demand answers. Your life might depend on it.
Can I stop taking one of these drugs if I’m worried about the interaction?
Never stop any of these medications without talking to your doctor. Stopping amiodarone suddenly can cause life-threatening arrhythmias. Stopping warfarin increases stroke risk. Stopping digoxin can worsen heart failure. The key isn’t stopping - it’s adjusting doses and monitoring closely under medical supervision.
How long does it take for amiodarone to affect digoxin and warfarin?
Amiodarone starts affecting digoxin within 2-7 days. For warfarin, INR levels can rise significantly within 3-10 days. But because amiodarone stays in your body for weeks to months, the effects continue long after you stop taking it. That’s why monitoring must continue for 4-6 weeks after discontinuation.
Are there safer alternatives to this combination?
Yes. For atrial fibrillation, newer rate-control drugs like beta-blockers (metoprolol) or ivabradine are safer than digoxin. For stroke prevention, DOACs like apixaban or rivaroxaban are preferred over warfarin - and they have fewer interactions with amiodarone. But switching isn’t always possible. Mechanical heart valves require warfarin. Some patients can’t afford DOACs. Always discuss alternatives with your cardiologist.
What symptoms should I watch for with this drug combo?
For digoxin toxicity: nausea, vomiting, loss of appetite, blurry or yellow vision, confusion, fast or irregular heartbeat. For warfarin over-anticoagulation: unusual bruising, nosebleeds, bleeding gums, blood in urine or stool, severe headaches, dizziness, weakness. If you notice any of these, call your doctor immediately - don’t wait.
Should I get blood tests if I’m on all three drugs?
Absolutely. You need a digoxin blood level test 72 hours after starting amiodarone, and then weekly until stable. You also need INR checks every 48-72 hours for the first two weeks, then weekly. These aren’t optional tests - they’re lifesaving. If your doctor doesn’t offer them, ask for them.




jeremy carroll
December 16, 2025 AT 02:38Thomas Anderson
December 16, 2025 AT 13:10Daniel Wevik
December 18, 2025 AT 10:12Dwayne hiers
December 20, 2025 AT 09:24Jonny Moran
December 21, 2025 AT 21:09Sarthak Jain
December 23, 2025 AT 08:02Edward Stevens
December 23, 2025 AT 15:30Rich Robertson
December 23, 2025 AT 17:50Daniel Thompson
December 23, 2025 AT 23:01Rulich Pretorius
December 25, 2025 AT 14:16Alexis Wright
December 25, 2025 AT 14:57Wade Mercer
December 27, 2025 AT 11:18Sinéad Griffin
December 28, 2025 AT 15:18Tim Bartik
December 30, 2025 AT 01:38Natalie Koeber
December 30, 2025 AT 13:32