What Happens When Your Heart Skips a Beat?
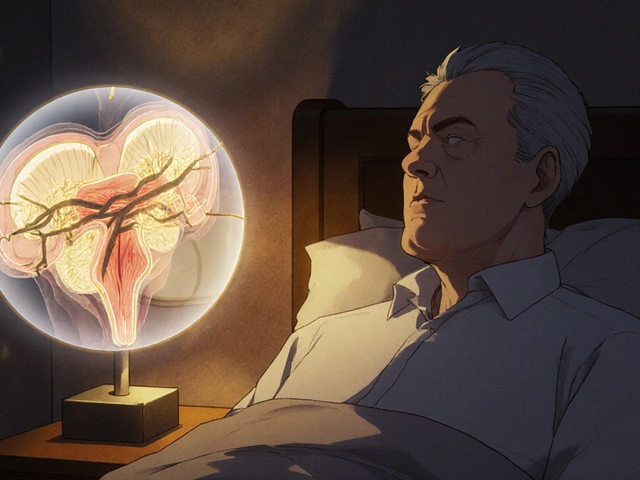
When your heart doesn’t beat in a steady rhythm, it’s not just annoying-it can be dangerous. Arrhythmias like atrial fibrillation (AFib) mean your heart’s electrical signals go haywire, causing it to flutter, race, or skip beats. For many, medications help. But if pills aren’t cutting it, two proven procedures can reset your heart’s rhythm: catheter ablation and device therapy.
Catheter Ablation: Fixing the Wiring Inside Your Heart
Catheter ablation isn’t open-heart surgery. It’s a minimally invasive procedure where thin, flexible tubes (catheters) are threaded through a vein in your groin or neck and guided to your heart. Once in place, the doctor uses energy-either heat (radiofrequency) or extreme cold (cryoablation)-to destroy tiny areas of heart tissue causing the abnormal signals.
For atrial fibrillation, the most common target is the pulmonary veins. These veins often fire off erratic signals that trigger AFib. The goal? Isolate them with a ring of scar tissue-called pulmonary vein isolation (PVI)-so they can’t interfere with your heart’s normal rhythm.
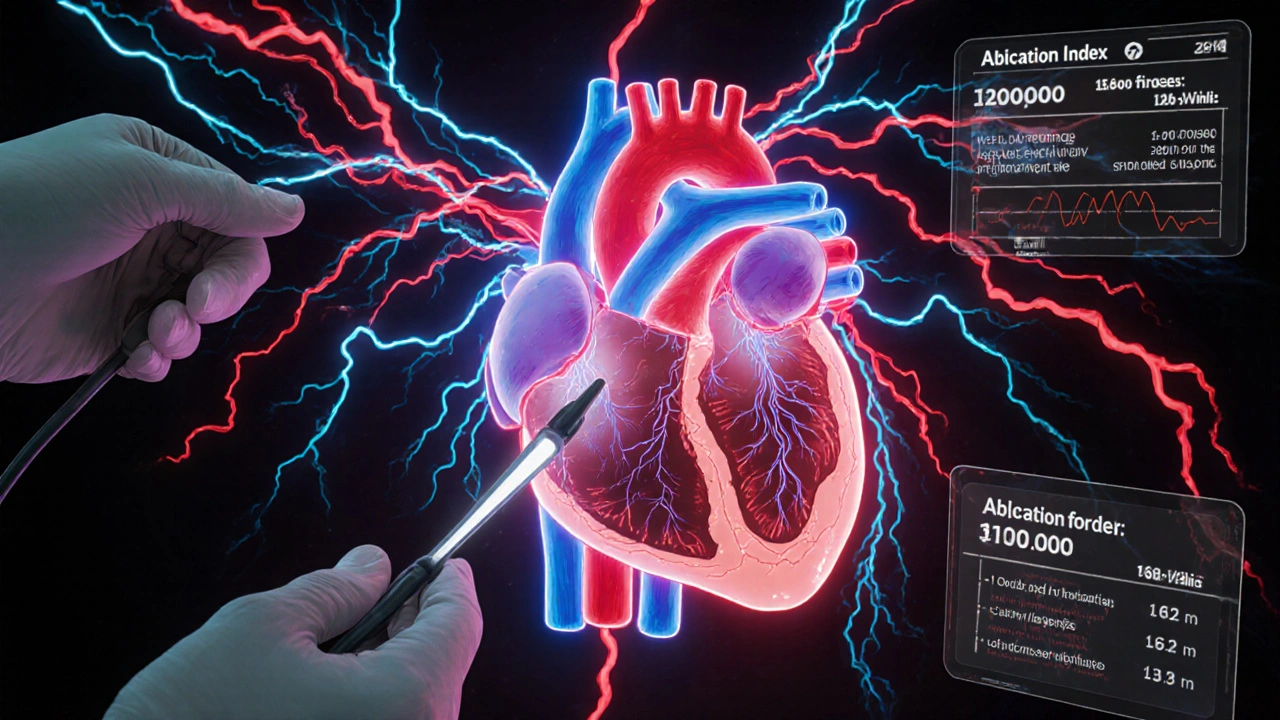
Modern ablation tools have come a long way since the 1990s. Today’s catheters, like the THERMOCOOL SMARTTOUCH a radiofrequency catheter with real-time contact force sensing and Ablation Index technology, measure how firmly the tip touches the heart wall. Too little contact? The lesion won’t stick. Too much? You risk tearing tissue. The Ablation Index combines contact force, power, and time into one number, helping doctors know exactly when they’ve created a lasting scar. Studies show this tech boosts success rates by 12-15% and cuts procedure time by about 25 minutes.
Cryoablation, using the Arctic Front Advance a cryoballoon system from Medtronic that freezes tissue with nitrous oxide, is another option. Instead of a catheter, it uses a balloon inflated at the opening of the pulmonary veins. It freezes tissue all at once, making it faster and easier for some doctors to learn. Procedures take about 90-120 minutes, compared to 150-180 for radiofrequency. But there’s a catch: it can accidentally affect the phrenic nerve, which controls your diaphragm. That’s why doctors monitor nerve function during the procedure.
Even newer is pulsed field ablation (PFA), approved by the FDA in 2023. The Farapulse PFA system a device using short bursts of electrical energy to disrupt heart cells without burning or freezing tissue works differently-it zaps cells with electric pulses, sparing surrounding structures like the esophagus. In trials, it achieved 85.9% freedom from AFib at one year, with procedures lasting just 76 minutes on average. It’s not everywhere yet, but it’s the future.
Device Therapy: Pacemakers and ICDs for When Ablation Isn’t Enough
Not all arrhythmias are caused by rogue electrical signals you can zap away. Some hearts are too weak, too slow, or too prone to dangerous rhythms. That’s where device therapy comes in.
Implantable Cardioverter Defibrillators (ICDs) devices implanted under the skin that monitor heart rhythm and deliver shocks to stop life-threatening arrhythmias are lifesavers for people at risk of sudden cardiac arrest. If your heart goes into ventricular fibrillation, the ICD detects it and zaps it back into rhythm-often before you even feel anything.
Cardiac Resynchronization Therapy (CRT) devices pacemakers that coordinate the pumping of the heart’s lower chambers to improve efficiency in heart failure patients are used when the heart’s left and right ventricles aren’t beating together. This mismatch makes pumping inefficient. CRT devices send timed pulses to both sides, helping the heart pump more blood. Studies show patients on CRT live longer, feel better, and are less likely to be hospitalized.
Some patients get a combo device: an ICD with CRT built in. These are common for people with heart failure and AFib who’ve had an ablation but still need rhythm control and protection from sudden death.
Ablation vs. Medication: The Numbers Don’t Lie
Doctors used to treat AFib with drugs first-beta blockers, antiarrhythmics, blood thinners. But for many, pills just don’t cut it. They cause side effects, don’t always work, and don’t fix the root problem.
A 2020 meta-analysis of nearly 1,800 patients showed catheter ablation reduced AFib recurrence by 58% compared to medication alone. It also cut hospital visits for heart problems by 44%. For people with heart failure and reduced pumping ability (HFrEF), the benefits were even clearer: ablation improved heart function by 5.67% on average, increased walking distance by 25 meters, and cut mid-term death risk by 48%.
And it’s not just physical. A 2023 JAMA study found patients who had ablation reported less anxiety, fewer panic attacks, and better sleep. Why? Because they weren’t living in fear of the next flutter. One patient on Reddit said, “I went from daily palpitations to zero episodes in 9 months-the mental relief is as valuable as the physical.”
But here’s the catch: the CABANA trial in 2019 found no overall survival benefit from ablation in all AFib patients. That’s because not everyone benefits equally. The biggest gains are in younger patients, those with paroxysmal AFib (episodes that start and stop), and especially those with heart failure. If you’re older, have long-standing AFib, or have other serious conditions, the benefit is smaller.
What’s the Cost? And Is It Worth It?
Catheter ablation isn’t cheap. In the U.S., the average cost runs $16,278 to $21,294. Medicare reimburses about $18,500. In Europe, it’s €12,000-€15,000. Device implants like ICDs or CRTs cost more-often $30,000-$50,000 including surgery and device.
But here’s the twist: ablation pays for itself. After 3 to 8 years, the money saved from fewer hospital stays, fewer doctor visits, and less medication use makes up for the upfront cost. A 2017 NIH study found ablation became cost-saving in just 3.2 years for patients with heart failure.
Device therapy costs more upfront and requires lifelong follow-ups, but for high-risk patients, it’s not just cost-effective-it’s life-saving. One ICD can prevent a sudden cardiac death that would cost hundreds of thousands in emergency care and long-term care.
Who Gets Which Procedure?
There’s no one-size-fits-all. Here’s how doctors decide:
- Paroxysmal AFib (episodes come and go) → Catheter ablation is first-line if meds fail. Success rates: 70-80% after one procedure.
- Persistent AFib (episodes last weeks or longer) → Ablation still works, but you might need more than one. Success drops to 50-60% after one session.
- Heart failure with AFib → Ablation is strongly recommended. It improves survival and heart function.
- High risk of sudden death (low EF, prior cardiac arrest) → ICD is the standard, even if you have AFib.
- Slow heart rate after ablation → You may need a pacemaker.
For most people with AFib and no major heart damage, ablation is now recommended after one failed drug trial-per 2020 European guidelines. In 2023, 78% of European centers offered it as first-line treatment for paroxysmal AFib, up from just 35% in 2015.
What Are the Risks?
No procedure is risk-free. Major complications happen in about 8% of ablation cases. The most serious is cardiac tamponade-bleeding into the sac around the heart. It occurs in 1.2% of cases and usually needs drainage.
Other risks:
- Phrenic nerve injury (with cryoablation): 1.5-3% chance. Can cause shortness of breath.
- Blood clots or stroke: less than 0.5% with proper blood thinners.
- Esophageal injury: rare, but serious. PFA has virtually eliminated this risk.
- Recurrence: 20-30% of patients need a second procedure, especially with persistent AFib.
Device therapy carries its own risks: infection at the implant site (1-3%), lead fractures (0.5% per year), or inappropriate shocks from ICDs (10-15% over 5 years).
Still, the benefits outweigh the risks for most candidates. Patient satisfaction is high: 78% of those reviewed on Healthgrades rated the procedure 4 or 5 stars and said they’d recommend it.
What’s Next for Arrhythmia Treatment?
The field is moving fast. AI tools like Medtronic’s AI Path software-expected in 2025-will analyze real-time heart maps to predict where lesions should go. 4D electroanatomic mapping lets doctors see the heart in motion, not just a static picture.
Pulsed field ablation is the biggest game-changer. With no heat, no cold, and no damage to nearby tissues, it could make ablation safer for everyone. Early data shows it’s faster, more precise, and better tolerated.
By 2030, experts predict ablation will become the first choice for nearly all symptomatic AFib patients-not just after drugs fail, but as the initial plan.
What Should You Do If You Have AFib?
If you’ve been told you have atrial fibrillation and meds aren’t working:
- Ask your cardiologist if you’re a candidate for catheter ablation.
- Find out if you have heart failure or reduced ejection fraction-that changes the game.
- Ask about contact force catheters and Ablation Index-ask if your center uses them.
- If you’re at risk for sudden death, ask about an ICD or CRT device.
- Don’t wait. The sooner you treat it, the better your heart recovers.
One patient, John M., 58, had AFib for 8 years. He was on three drugs. Still felt tired. Couldn’t cycle. After cryoablation in March 2022, he’s been AFib-free. No meds. Back on his bike. Competing again.
Your heart doesn’t have to keep skipping beats. There’s a fix. And it’s working better than ever.



Peter Aultman
November 14, 2025 AT 02:25Sean Hwang
November 14, 2025 AT 18:53gent wood
November 16, 2025 AT 00:02Jane Johnson
November 16, 2025 AT 04:54Don Ablett
November 17, 2025 AT 07:57Kevin Wagner
November 18, 2025 AT 13:36Dilip Patel
November 19, 2025 AT 10:23Scarlett Walker
November 19, 2025 AT 14:06Brittany C
November 21, 2025 AT 03:24Sean Evans
November 22, 2025 AT 20:54Anjan Patel
November 23, 2025 AT 19:39