When you take a blood thinner, you're trading one risk for another. You reduce the chance of a deadly clot, but you open the door to something just as dangerous: uncontrolled bleeding. A single extra pill, a missed blood test, or even a bad interaction with another drug can push you into a medical emergency. And the worst part? Many people don’t realize they’re in danger until it’s too late.
What Happens When a Blood Thinner Goes Too Far
Blood thinners like warfarin, apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) work by slowing down your blood’s ability to clot. That’s good when you have atrial fibrillation or a history of clots. But if you take too much-or your body can’t clear it properly-your blood loses its ability to stop bleeding entirely. Even a small bump can turn into a dangerous internal bleed. Warfarin, the oldest of these drugs, can take days to fully leave your system. Its effects can last up to five days after you stop taking it. That means an overdose isn’t a one-time event-it’s a slow-burning fuse. For newer drugs like apixaban or rivaroxaban, the risk is shorter but no less serious. One study found that patients who took just 20% more than their prescribed dose had a 40% higher chance of major bleeding. The key danger isn’t external bleeding. It’s internal. You won’t always see it. Blood can pool silently in your brain, stomach, or muscles. That’s why symptoms can be subtle-and easily ignored.Signs of Internal Bleeding You Can’t Afford to Ignore
If you’re on a blood thinner, here’s what to watch for:- Black, tarry stools or blood in your stool
- Pink, red, or dark brown urine
- Vomiting blood or material that looks like coffee grounds
- Unexplained bruising, especially large or spreading patches
- Small red or purple dots under the skin (petechiae)
- Prolonged nosebleeds or gum bleeding that won’t stop after 10 minutes of pressure
- Heavy or unusual menstrual bleeding
- Sudden, severe headache, dizziness, or confusion
- Sharp pain in your abdomen, chest, or back
- Extreme fatigue, weakness, or feeling like you’re about to pass out
What to Do Right Now If You Suspect an Overdose
Time is everything. The sooner you act, the better your chances.- Call 911 or go to the nearest ER immediately. Don’t wait. Don’t call your doctor first. Internal bleeding doesn’t wait.
- Do not take another dose. Even if you think you missed one, don’t double up. You’re already at risk.
- Write down what you took, when, and how much. Bring the pill bottle with you. This helps doctors act faster.
- Don’t take aspirin, ibuprofen, or naproxen. These make bleeding worse. Stick to acetaminophen (Tylenol) only if you need pain relief-and even then, check with a pharmacist first.
- Apply firm pressure to any external bleeding. Keep pressure on for at least 10 minutes without checking. Lifting pressure too soon can restart bleeding.
- Stay lying down. Elevate the bleeding area if possible. Sitting or standing can increase blood flow to the area and make bleeding worse.

How Doctors Treat Blood Thinner Overdose
What happens in the ER depends on which drug you took and how bad your INR (a blood test that measures clotting time) is. For warfarin overdoses:- If your INR is over 4.5 but you’re not bleeding, you’ll likely get oral vitamin K. This helps your body start making clotting factors again.
- If you’re bleeding, you’ll get 4-factor Prothrombin Complex Concentrate (PCC) within minutes. This is a concentrated mix of clotting factors that works fast-often within 15 to 30 minutes.
- Vitamin K is given intravenously too, but it takes hours to work. That’s why PCC is the first line.
- For dabigatran (Pradaxa), doctors use idarucizumab (Praxbind). It reverses the drug in minutes.
- For apixaban or rivaroxaban, they use andexanet alfa (Andexxa). It’s expensive-up to $10,000 per dose-but life-saving.
- If these aren’t available, doctors may use activated charcoal (if the overdose was recent) or PCC as a backup.
Why People Delay-And Why That’s Deadly
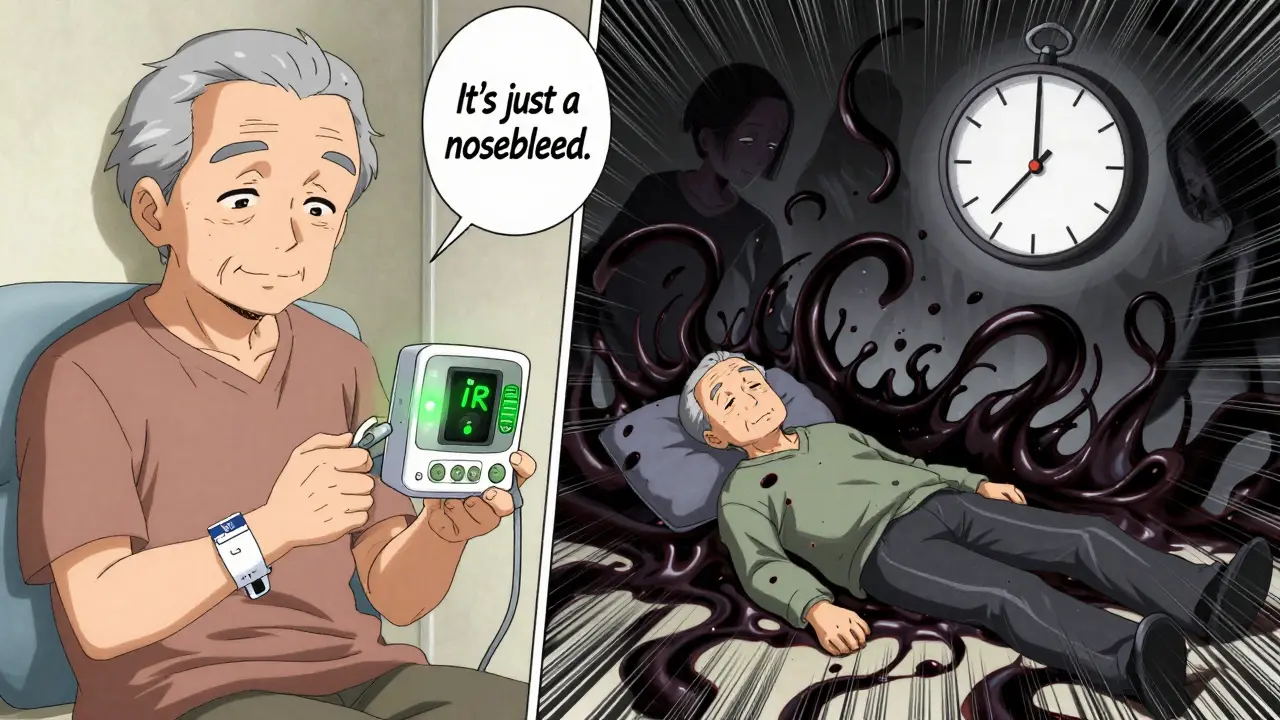
Dr. Katherine L. Hess from Johns Hopkins says nearly 3 out of 10 patients wait more than 12 hours before seeking help. Why? They think:- "It’s just a nosebleed. It’ll stop."
- "My stool is dark because of the iron pills."
- "I’m just tired from working too hard."
How to Prevent This From Happening
You can’t control everything-but you can control these five things:- Know your INR target. Most people need 2.0-3.0. If you have a mechanical heart valve, it’s 2.5-3.5. Ask your doctor to write it down.
- Test regularly. If you’re on warfarin, check your INR every 1-4 weeks. Use a home monitor if your doctor recommends it. Studies show home testing cuts major bleeding by 34%.
- Keep a bleeding risk checklist. Tape it to your fridge. Include: prolonged bleeding, bruising, dark urine, black stools, severe headache.
- Review all your meds with your pharmacist. Antibiotics, NSAIDs, even some herbal supplements like ginkgo or garlic can interact with blood thinners.
- Wear a medical alert bracelet. If you collapse, first responders need to know you’re on a blood thinner. It changes everything.
What’s Changing in 2026
The future is getting better. In 2023, the FDA approved ciraparantag for Phase III trials. This is the first universal reversal agent-it can stop bleeding from any blood thinner in under 10 minutes. It’s not on the market yet, but it’s coming. Meanwhile, point-of-care INR devices are getting cheaper. You can now buy a reliable home monitor for under $300. Some insurance plans cover them. If you’re on warfarin, ask your doctor if it’s right for you.Final Word: Don’t Wait for a Crisis
Blood thinners save lives. But they demand respect. You don’t need to live in fear-but you do need to be alert. Know the signs. Know what to do. And if something feels wrong, act fast. The difference between life and death isn’t always the drug you take. It’s the moment you decide to call for help.Can you reverse a blood thinner overdose at home?
No. There is no safe or effective way to reverse a blood thinner overdose at home. Vitamin K for warfarin or other treatments like PCC or reversal agents require medical supervision and IV delivery. Trying to manage this yourself can lead to fatal internal bleeding. If you suspect an overdose, call 911 immediately.
How long does it take for a blood thinner overdose to show symptoms?
It varies. For warfarin, symptoms can take 12 to 72 hours to appear because it takes time for clotting factors to drop. For DOACs like Eliquis or Xarelto, symptoms can show up within hours, especially if a large dose was taken. But bleeding can also be delayed-some patients don’t show signs until days later. Don’t wait for symptoms to appear before acting.
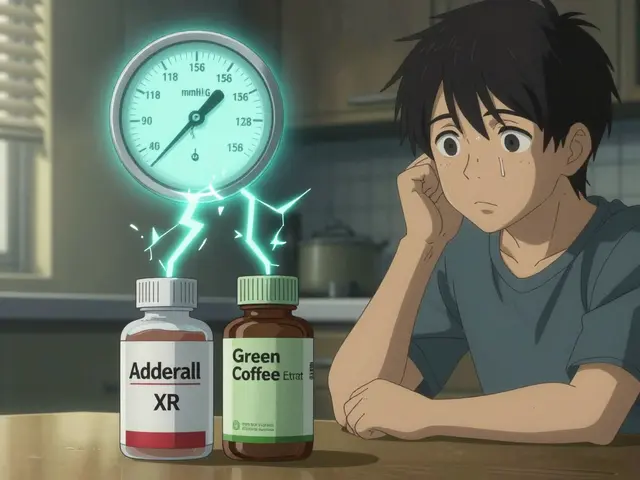
Can you take aspirin if you’re on a blood thinner?
No-not unless your doctor specifically says so. Aspirin is an antiplatelet drug that also thins the blood. Taking it with warfarin, Eliquis, or Xarelto greatly increases your risk of bleeding. Even low-dose aspirin can be dangerous. Always check with your doctor or pharmacist before taking any new medication, including over-the-counter pain relievers.
What’s the safest blood thinner to avoid overdose?
There’s no "safest" blood thinner-only the right one for you. DOACs like apixaban and rivaroxaban don’t require regular blood tests like warfarin does, which reduces the risk of dosing errors. But they’re not foolproof. All blood thinners carry bleeding risks. The key isn’t the drug-it’s adherence, monitoring, and knowing the warning signs. Work with your doctor to choose the best option based on your health, lifestyle, and ability to follow the regimen.
Can you survive a massive blood thinner overdose?
Yes, but only with immediate medical care. One case study in 2016 described a woman who took 450 mg of warfarin-15 times the normal daily dose. She survived because she reached the hospital quickly, received vitamin K, and was monitored closely. Survival depends on how fast you get treatment, how much you took, and your overall health. Delaying care drops survival rates from 97% to 76% within six hours.
Do all blood thinners cause the same kind of bleeding?
The symptoms are similar-internal bleeding, bruising, blood in urine or stool-but the speed and treatment differ. Warfarin affects multiple clotting factors and lasts days, so bleeding can be prolonged. DOACs act faster and wear off quicker, but they can cause sudden, severe bleeding if taken in excess. Reversal agents exist for DOACs but not for warfarin (vitamin K helps, but it’s slower). The type of bleeding isn’t different-it’s the timing and treatment that changes.





Lawrence Jung
January 12, 2026 AT 08:23People think meds are magic bullets but they’re not. You take a blood thinner like it’s coffee and forget you’re playing Russian roulette with your insides. No one tells you how quietly you can bleed out until your hemoglobin hits 6 and you’re staring at the ceiling wondering why your legs feel like lead
Alice Elanora Shepherd
January 13, 2026 AT 23:49It’s so important to recognize that internal bleeding doesn’t always come with screaming symptoms. I’ve seen elderly patients dismiss dark stools as ‘just diet,’ and by the time they get to us, they’re in shock. Please-don’t normalize these signs. If you’re on a blood thinner, treat every odd symptom like a fire alarm. And yes, wear the medical bracelet. It saves lives.
Alex Fortwengler
January 14, 2026 AT 01:35Big Pharma loves these drugs because they make you dependent. Warfarin’s been around since the 1950s and they still can’t get the dosing right. Now they push these $10k reversal agents? That’s not medicine-that’s a money grab. And don’t get me started on home monitors. They’re overpriced junk pushed by reps who don’t care if you live or die as long as the script gets filled
Abner San Diego
January 15, 2026 AT 19:03Why do we even let foreigners design our meds? I mean, look at this-some lab in Switzerland decides what my blood does? And now I gotta carry a damn bracelet like I’m a walking hazard? This is why America’s healthcare is a joke. Just let people die naturally instead of turning us into lab rats with pill schedules
TiM Vince
January 16, 2026 AT 06:50My grandfather took warfarin for 12 years. He never missed a test, always kept his INR log in a notebook, wore his bracelet, and still got a bleed in his gut because he ate a bunch of kale one week. No one warns you that food matters. Spinach, broccoli, even green tea-it all shifts the balance. It’s not just about the pill. It’s about your whole damn life.
Jessica Bnouzalim
January 16, 2026 AT 12:39Y’ALL. I just started on Xarelto last month and I was SO scared. But then I printed out that checklist and taped it to my fridge next to my coffee maker. Now every time I grab a cup, I check: bruise? stool? headache? It’s crazy how much peace of mind that gives me. You don’t need to be paranoid-you just need to be consistent 💪🩸
Jay Powers
January 16, 2026 AT 19:57One thing nobody talks about is how isolating this is. You can’t go hiking with your friends anymore because you’re scared of a fall. You can’t even take Tylenol without checking with your pharmacist. And if you tell someone you’re on a blood thinner, they look at you like you’re broken. But you’re not. You’re just managing a silent war inside your veins.
Konika Choudhury
January 18, 2026 AT 05:31Why do Americans always think they need a new drug for everything? In India we use aspirin and turmeric for everything. Even heart patients. No fancy pills. No $10k reversal agents. Just discipline. You take your medicine. You avoid risk. You don’t panic. This whole system is built on fear and profit. We need to go back to basics.
Windie Wilson
January 19, 2026 AT 09:11Oh wow. So now I’m supposed to be a detective AND a pharmacist AND a nurse? Thanks for the reminder that my body is a ticking time bomb that I have to monitor 24/7. Meanwhile my insurance won’t cover the home monitor and my doctor won’t return my texts. But hey, at least I’m not dying yet. 😌
Daniel Pate
January 19, 2026 AT 12:32The real tragedy isn’t the overdose-it’s the systemic failure to educate. We treat anticoagulants like they’re vitamins, not precision instruments. We don’t teach patients how to think about their own physiology. We hand them a script and say ‘take this.’ And then we’re shocked when they bleed out. Medicine has become transactional, not educational. And education is the only true antidote.
jordan shiyangeni
January 21, 2026 AT 11:20Let me be perfectly clear: if you’re on a blood thinner and you don’t have a written, signed, and witnessed emergency plan with your family, you’re not just irresponsible-you’re endangering others. You think your neighbor will know what to do if you collapse? They’ll call 911, sure, but they won’t know you’re on Xarelto. They won’t know to say ‘don’t give aspirin.’ They won’t know to grab your pill bottle. You owe it to your loved ones to prepare. This isn’t optional. This is moral.
Monica Puglia
January 22, 2026 AT 13:29I’m on Eliquis and I just got my first home INR monitor! It’s like having a tiny doctor in my kitchen 🥹 I test every Monday and Friday and log it in my phone. My doctor says I’ve cut my risk in half. And guess what? I still eat pizza. I just check my symptoms. You don’t have to live in fear-you just have to be smart. 💙
George Bridges
January 23, 2026 AT 08:17Thanks for writing this. My mom had a bleed last year. She didn’t know what was happening until she couldn’t stand up. We got lucky. But reading this made me realize how little I understood. I’m printing this out and putting it in her binder. Not because she’s forgetful-but because everyone deserves to know what’s happening inside their own body.