Handling chemotherapy isn’t just about giving a patient a drug. It’s about protecting the nurse, the caregiver, the environment, and the patient from serious harm. Every vial, every syringe, every drop of bodily fluid after treatment carries risk. In 2024, the standards for chemotherapy safety changed - not because things were broken, but because we now know just how dangerous even small mistakes can be.
Why Chemotherapy Is Different From Other Medications
Most drugs are safe to handle with bare hands. Not chemotherapy. Antineoplastic agents are designed to kill fast-growing cells - that’s how they target cancer. But they don’t know the difference between a cancer cell and a healthy one. Skin contact, inhalation, or accidental ingestion can cause nausea, infertility, birth defects, or even secondary cancers in healthcare workers. This isn’t theoretical. Studies since the 1990s have found chemotherapy drugs on nurses’ gloves, countertops, and even in their urine. The risk doesn’t go away after the treatment ends. For 48 to 72 hours after a patient receives chemo, their sweat, urine, vomit, and even saliva can still contain active drug particles.The Four Pillars of Modern Chemotherapy Safety (ASCO/ONS 2024)
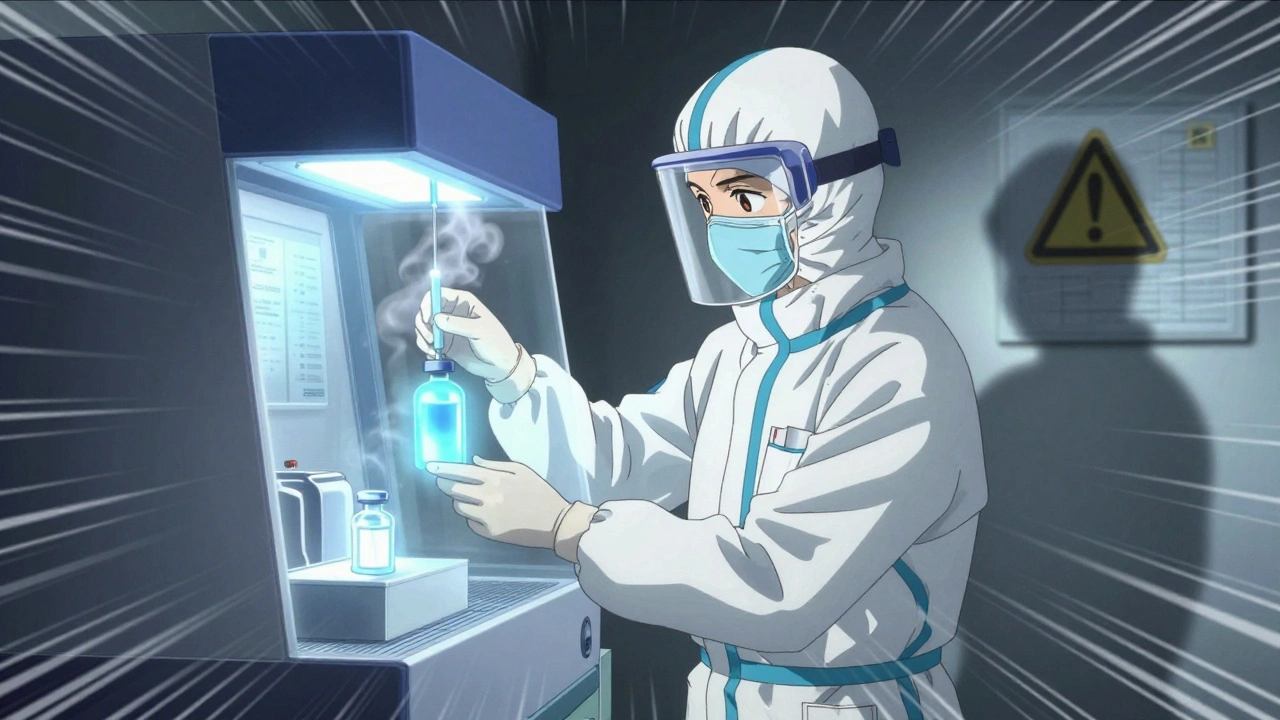
The latest safety standards from the American Society of Clinical Oncology and Oncology Nursing Society aren’t suggestions - they’re mandatory for accredited facilities. They’re built on four core areas:- Safe Environment: Facilities must use engineering controls like closed-system transfer devices (CSTDs) to prevent aerosol release during drug preparation. Ventilated cabinets, spill kits, and dedicated chemo preparation areas are required. No more mixing drugs on a regular counter.
- Patient Consent and Education: Before treatment, patients must be told exactly what drug they’re getting, why, how long it will last, and what side effects to watch for. This isn’t just paperwork - it’s part of safety. A patient who understands their treatment is more likely to report problems early.
- Ordering, Preparing, and Administering: This is where the biggest change happened. The 2024 update added a fourth verification step. Before the drug goes in, two licensed clinicians must check the patient’s name, date of birth, drug name, dose, route, and timing - in front of the patient. They use two identifiers, like name and DOB, not room number or chart number. This step alone reduced patient identification errors by 18% in early adopter clinics.
- Monitoring During and After: New drugs like CAR-T and bispecific antibodies can trigger cytokine release syndrome (CRS), a dangerous immune overreaction. Facilities must now have antidotes like tocilizumab and steroids ready at the bedside. Nurses are trained to recognize early signs: fever above 100.4°F, low blood pressure, or trouble breathing within hours of infusion.
Personal Protective Equipment (PPE) - What You Actually Need
Forget the old rules. You don’t just wear gloves. You wear the right gloves. NIOSH and USP <800> require chemotherapy-tested double gloves. Regular exam gloves? They break down in minutes when exposed to drugs like carmustine or thiotepa. Double gloving isn’t optional - it’s the minimum. The outer glove is changed every 30 minutes or immediately if torn. Gloves are never reused. Gowns must be made of impermeable material - not cotton, not polyester. They’re disposable and worn over regular scrubs. Eye protection is required whenever there’s any chance of splashing. Face shields are recommended during high-risk procedures like reconstitution. Respirators (N95 or higher) are needed if there’s a risk of aerosol, like during needleless system connections or spill cleanup. And here’s the hard truth: once you’ve handled chemo, your PPE is contaminated. Even if it looks clean. You don’t take it home. You don’t reuse it. You dispose of it in a hazardous waste container labeled for antineoplastic agents. A 2015 ACCC study showed that 87% of contamination incidents happened because staff removed gloves incorrectly or reused gowns.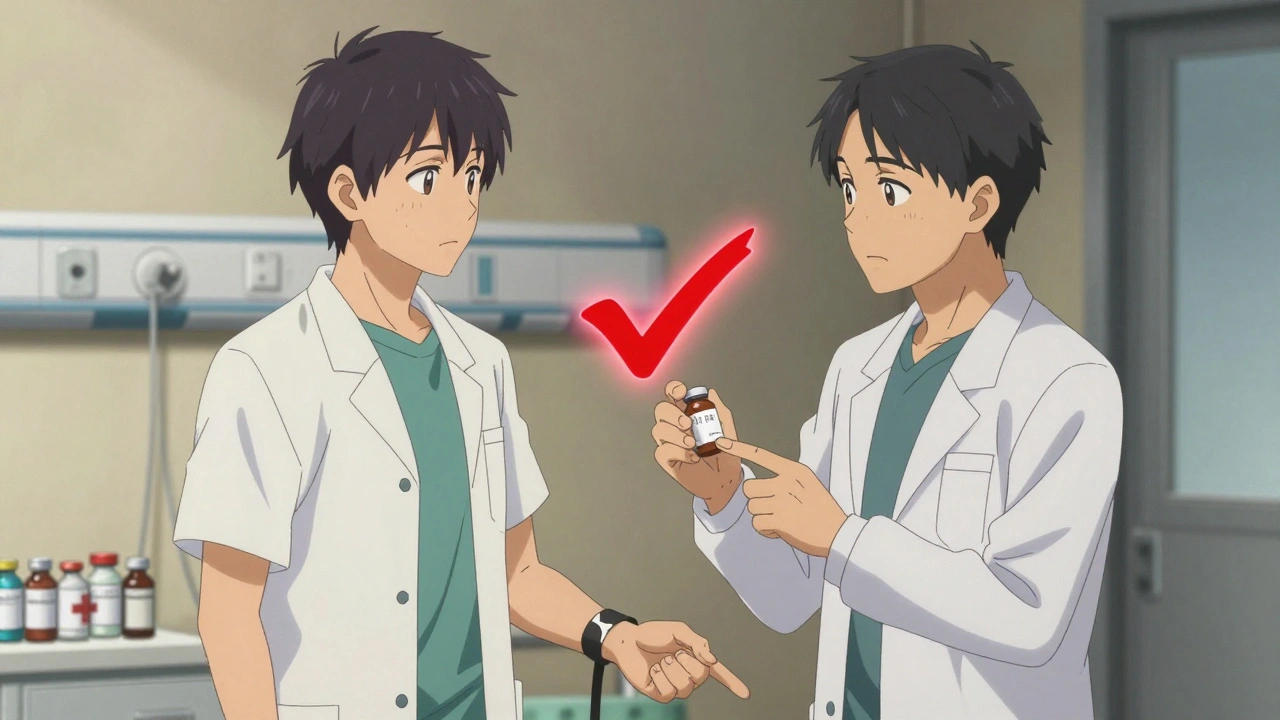
Home Chemotherapy - The Hidden Risk
More patients are getting chemo at home now. It’s convenient. But it’s dangerous if not done right. The American Cancer Society found that 22% of home care incidents involve improper disposal of chemo waste - syringes, vials, even tissues used to wipe nose or mouth. Seventeen percent involve failed spill management. A single drop of fluid on the bathroom floor can expose a child or pet. Families are given education materials. But 65% of caregivers say they still feel unprepared. The biggest fears? Handling urine or vomit (82%) and disposing of needles (76%). Facilities that use the ASCO-developed Chemotherapy Safety at Home toolkit - which includes color-coded disposal bags, spill kits, and step-by-step videos - saw a 41% drop in caregiver-reported safety concerns. The key? Don’t just hand out a pamphlet. Walk them through it. Show them how to use the kit. Have them demonstrate it back.The Real Cost of Getting It Right
Implementing full safety standards isn’t cheap. A medium-sized oncology clinic needs:- $22,000-$35,000 for facility upgrades (CSTDs, ventilation, dedicated rooms)
- $8,500-$12,000 for staff training and certification
- $4,200-$6,800 per year for PPE and hazardous waste disposal
- $15,000-$40,000 to modify EHR systems to support the four-step verification
What’s Next? AI, Certification, and Equity
The future of chemo safety is changing fast. By 2026, a national certification for chemotherapy administration staff is expected - meaning you won’t just be trained, you’ll be certified. Pilot programs at 12 top cancer centers are testing AI tools that scan patient wristbands and drug labels to auto-verify doses. If the system flags a mismatch, it stops the process before the drug is drawn. But there’s a dark side. Rural clinics struggle. Forty-three percent say they can’t afford CSTDs. That means patients in those areas might get the same drug, but not the same safety. Dr. Sarah Temkin from UVA Health warns this is creating a two-tiered system - one standard for cities, another for small towns. Until funding catches up, patients in underserved areas are at higher risk.
What You Can Do - Whether You’re a Nurse, Caregiver, or Patient
If you’re a healthcare worker: Don’t skip the double gloves. Don’t rush the fourth verification. Report near-misses - even if no one got hurt. That’s how systems improve. If you’re a caregiver: Ask for the Chemotherapy Safety at Home toolkit. Practice spill cleanup with your nurse. Don’t assume you know what to do. Keep disposal bags sealed and out of reach of children. Wash hands after touching anything that might be contaminated. If you’re a patient: Ask your nurse: “Are you using two identifiers before giving me this drug?” If they say no, ask why. You have the right to be safe.Frequently Asked Questions
Can I touch my pet after chemotherapy?
For 48 to 72 hours after treatment, your bodily fluids - including saliva, sweat, and urine - can still contain chemotherapy drugs. Avoid letting pets lick you, especially around the mouth or open wounds. Wash your hands before petting them. Use separate bedding and clean litter boxes or pet areas with gloves and disinfectant.
Why do nurses wear two pairs of gloves?
Single gloves can break or allow drugs to permeate within minutes. Double gloving creates a backup layer. Studies show that if the outer glove is torn, the inner glove stops 95% of drug exposure. Gloves are tested for resistance to specific chemotherapy agents - not all gloves are equal. Always use gloves labeled for chemotherapy use.
Is chemotherapy still dangerous if it’s in a closed system?
Closed-system transfer devices (CSTDs) reduce but don’t eliminate risk. They prevent aerosols and spills during transfer, but contamination can still happen during preparation, priming lines, or connecting IV tubing. PPE is still required. CSTDs are a tool, not a replacement for safety protocols.
What happens if a chemo spill occurs?
Never clean it with a regular towel. Use a chemo spill kit, which includes absorbent pads, neutralizing agents, and disposable PPE. Evacuate the area. Wear double gloves, a gown, eye protection, and an N95 mask. Start from the edges of the spill and work inward. Place all contaminated materials in a hazardous waste container labeled for antineoplastic agents. Report the spill to your safety officer.
Why is the fourth verification step so important?
Before 2024, patient identification errors caused 18% of chemotherapy-related adverse events. Giving the wrong drug or dose can be fatal. The fourth verification - done face-to-face with two staff members using two patient identifiers - adds a final, human checkpoint. It’s not just about checking a screen. It’s about looking the patient in the eye and confirming their name and birthdate together.
Can chemotherapy be safely administered in a non-hospital setting?
Yes - but only if the facility meets the full ASCO/ONS 2024 standards. That means proper ventilation, CSTDs, trained staff, verified protocols, and access to emergency drugs like tocilizumab for CRS. Many community clinics now meet these standards. But if a clinic doesn’t have a safety committee, dedicated prep area, or double verification process, it’s not safe.




Steve Sullivan
December 9, 2025 AT 09:28Ajit Kumar Singh
December 10, 2025 AT 20:56Simran Chettiar
December 12, 2025 AT 02:00Anna Roh
December 13, 2025 AT 23:15Richard Eite
December 14, 2025 AT 13:23Katherine Chan
December 15, 2025 AT 04:12Philippa Barraclough
December 17, 2025 AT 03:46Tim Tinh
December 18, 2025 AT 20:56Olivia Portier
December 20, 2025 AT 19:23Andrea Petrov
December 21, 2025 AT 03:35Tiffany Sowby
December 22, 2025 AT 02:02