When a product leaves a manufacturing facility, it shouldn’t carry hidden risks. In pharmaceutical, food, and cosmetic production, environmental monitoring isn’t optional-it’s the last line of defense against contamination that could sicken consumers or trigger recalls. This isn’t about checking boxes. It’s about knowing exactly where germs, particles, or chemicals are hiding before they ruin a batch or worse, reach a patient or family dinner table.
Why Environmental Monitoring Matters More Than You Think
Think about the last time you opened a bottle of medicine or ate a ready-to-eat salad. You trusted it was safe. That trust comes from dozens of invisible checks happening daily inside the factory. Environmental monitoring catches what product testing alone can’t. A single swab from a conveyor belt or air sample near a filling line can reveal a problem before a single contaminated unit is packaged.
The FDA and EMA don’t just recommend this-they require it. In 2023, the FDA explicitly stated that environmental monitoring and product testing are the primary tools to verify control of microbial hazards. The CDC backs this up: up to 87% of foodborne illness outbreaks tied to manufacturing could’ve been stopped with proper environmental sampling. That’s not a small number. It’s $77.7 billion in annual economic losses, according to the USDA.
Pharmaceutical companies have known this for decades. But food processors, especially small ones, are still catching up. Only 76% of food facilities have formal programs, compared to 98% of drug manufacturers. That gap isn’t just a compliance issue-it’s a public health risk.
The Zone System: How to Map Risk in Your Facility
You can’t test everything. So you test smart. That’s where the zone system comes in. It’s not fancy, but it’s proven. Facilities divide their space into four risk zones based on how close surfaces are to the product.
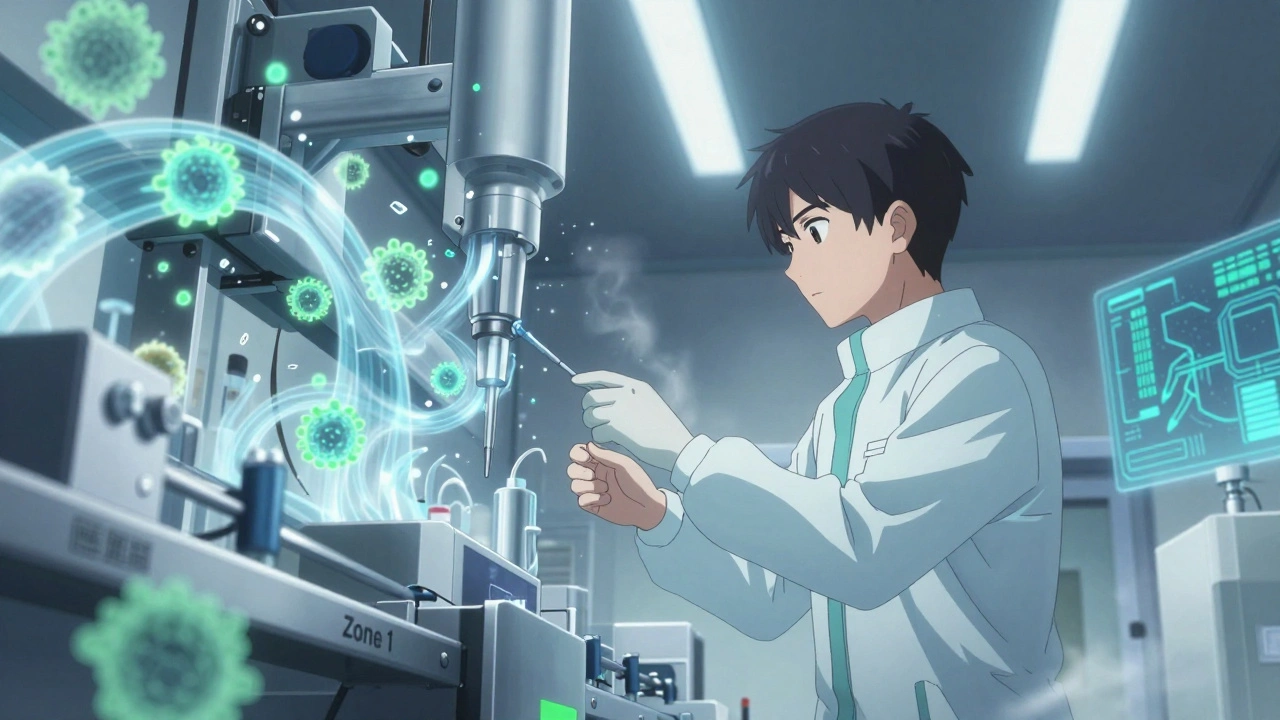
- Zone 1: Direct product contact surfaces-slicers, mixers, filling nozzles, packaging molds. These are the highest risk. If a pathogen lands here, it goes straight into your product.
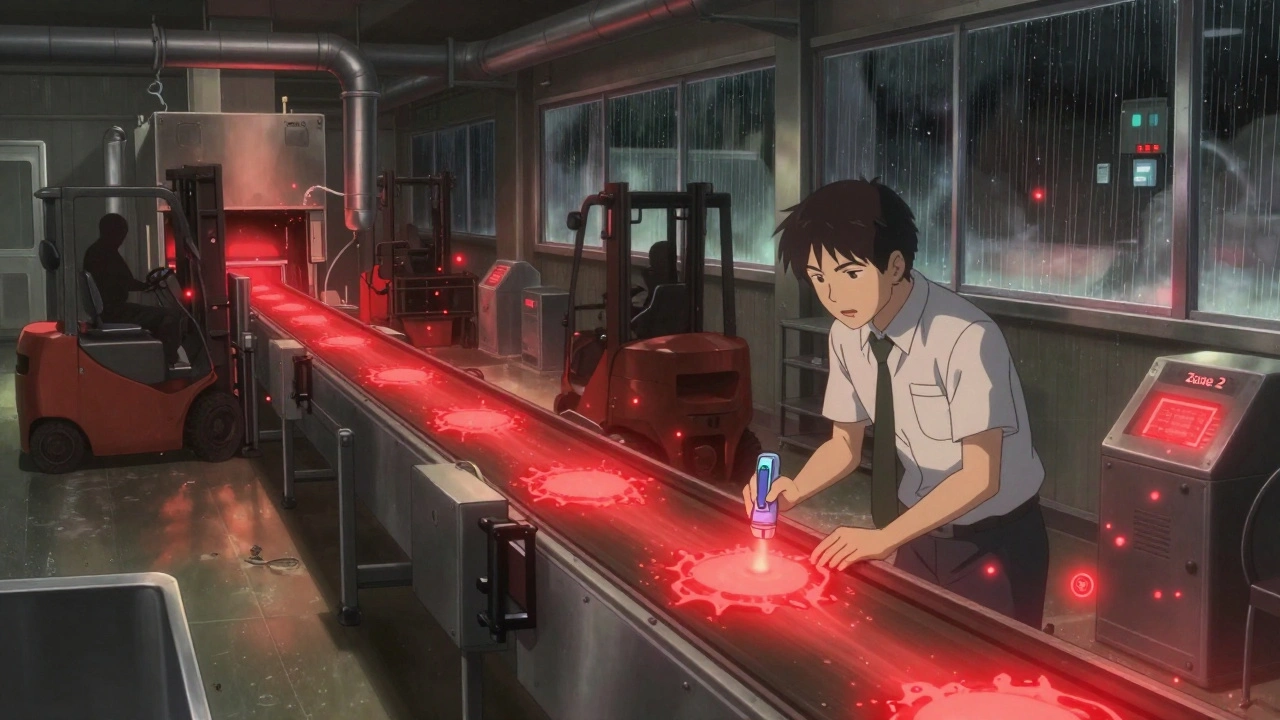
- Zone 2: Surfaces near product contact-equipment housings, refrigeration units, nearby conveyor belts. Contamination here can drift or splash onto Zone 1.
- Zone 3: Remote but still in the production area-forklifts, carts, overhead pipes, maintenance tools. These seem harmless, but a 2010-2013 study by PPD Laboratories found that 62% of all contamination events originated from Zone 3 and 4 surfaces.
- Zone 4: Outside production areas-break rooms, hallways, restrooms. Low risk, but still monitored to catch cross-contamination.
Here’s the catch: not every facility agrees on what belongs in each zone. One manager might see condensation on a pipe and treat it as Zone 1. Another might ignore it. That inconsistency is one of the top reasons monitoring programs fail. Clear, documented zone definitions based on actual risk-not guesswork-are non-negotiable.
What You’re Testing For-and How
Not all contamination is the same. The tools you use depend on what you’re looking for.
- Microbes: Swabs, sponges, and air samplers detect bacteria like Salmonella, Listeria monocytogenes, and molds. In RTE food plants, Listeria is the #1 target. In pharma, it’s general bioburden and endotoxins.
- Airborne particles: In cleanrooms, laser-based particle counters measure non-viable particles per cubic meter. Pharmaceutical cleanrooms must meet ISO Class 5 (EU Grade B) standards-continuous monitoring is required.
- Chemicals and metals: ICP (Inductively Coupled Plasma) detects trace metals. Chromatography (GC, HPLC) finds residual solvents or cleaning agents.
- Water quality: Pharmaceutical facilities test purified water using conductivity and TOC (Total Organic Carbon) to meet USP <645> standards. Food plants rely on EPA municipal water rules.
Sampling methods matter too. Liquid impingers and solid impactors pull air through liquid or onto sticky surfaces to capture microbes. Slit or sieve impactors must be sterilized before every use-something 68% of facilities still mess up, according to the IDFA’s 2020 survey.
How Often Should You Test?
Frequency isn’t one-size-fits-all. It’s risk-based.
- Zone 1: Daily to weekly. FDA requires weekly Listeria testing in RTE food Zone 1 areas.
- Zone 2: Weekly to monthly.
- Zone 3 and 4: Monthly to quarterly.
But don’t just follow a calendar. If a new machine is installed, or a leak occurs, ramp up sampling. If your air particle counts spike after cleaning, investigate. Monitoring isn’t passive-it’s reactive and adaptive.
One common mistake: relying only on traditional microbiology tests that take 24-72 hours to yield results. That’s too slow. ATP (adenosine triphosphate) testing gives results in seconds by measuring organic residue. Facilities using ATP report 32% faster production turnaround times. It’s not a replacement for microbial testing-it’s a real-time checkpoint.
Who Does the Work-and Are They Trained?
Environmental monitoring isn’t something you hand off to the janitorial staff. It requires trained personnel who understand sterile technique, sampling protocols, and data interpretation.
The FDA recommends at least 40 hours of hands-on training before someone can collect official samples. That includes learning how to swab correctly-pressure, area covered, surface type-and how to avoid contaminating the sampler itself. Many labs fail because the sampler’s interior wasn’t sterilized. Sounds basic? It’s overlooked more than you’d think.
Medium-sized food plants typically assign 2-3 full-time staff to environmental monitoring. Annual costs for supplies and lab services run $15,000-$25,000. Small facilities under 50 employees struggle most-only 48% maintain fully compliant programs, per USDA data. Outsourcing to a certified lab is often the smarter move.
The Biggest Pitfalls-and How to Avoid Them
Even with the best tools, programs fail because of human error and poor systems.
- Inconsistent zone classification: 42% of facilities have this problem. Fix it with a documented, cross-departmental zone map reviewed quarterly.
- Fragmented data: ATP, allergen, and microbiological results are often stored separately. That’s like having three different dashboards for your car’s speed, fuel, and engine light. Integration is key. Newer software platforms now combine all data into one dashboard.
- Ignoring Zone 3 and 4: Remember, 62% of contamination events came from these areas in PPD’s study. Don’t treat them as afterthoughts.
- Over-monitoring: More tests don’t mean better safety. PPD found that a focused, fit-for-purpose program with limited but smart sampling outperforms sprawling, untargeted efforts.
What’s Next? AI, Real-Time Data, and Faster Detection
Environmental monitoring is evolving fast. The FDA’s 2023 draft guidance encourages next-generation sequencing (NGS) and metagenomics to identify pathogens in under 24 hours-down from 3-5 days. That’s huge for recall prevention.
EU GMP Annex 1, updated in August 2023, now requires real-time data trending for critical parameters like temperature, humidity, and particle counts. Facilities that don’t adopt this risk non-compliance.
AI is coming. By 2027, 38% of monitoring systems will use machine learning to predict contamination risks based on historical data, shift patterns, and environmental changes. One study showed integrating environmental data with culture contamination logs reduced false positives by 27%.
And don’t ignore antimicrobial resistance. The CDC found 19% of Listeria isolates from food environments are now resistant to multiple antibiotics. Monitoring isn’t just about cleanliness anymore-it’s about tracking evolving threats.
Final Thought: It’s Not About Compliance. It’s About Trust.
Environmental monitoring isn’t a cost center. It’s a trust engine. Every swab, every air sample, every data point builds confidence-for regulators, for customers, and for your own team.
When you know your Zone 1 surfaces are clean, your air meets ISO Class 5, and your water is pure, you don’t just avoid recalls. You build a reputation for reliability. In industries where one mistake can cost lives, that’s the only metric that truly matters.
What’s the difference between environmental monitoring and product testing?
Product testing checks the final item-like a pill or a packaged meal-for contamination. Environmental monitoring checks the surroundings: surfaces, air, water, and equipment where contamination could originate. You can have clean products but dirty environments, which means the next batch could be contaminated. Environmental monitoring stops problems before they happen.
Do small manufacturing facilities need full environmental monitoring programs?
Yes-even small facilities are legally required to control contamination. But they don’t need the same scale as big pharma. They can focus on Zone 1 and 2, use ATP testing for quick checks, and outsource lab analysis. The USDA found only 48% of small facilities (<50 employees) are fully compliant, but even basic monitoring reduces risk dramatically.
How do I know if my environmental monitoring program is working?
Look at trends over time. If alert or action limits are rarely exceeded, and contamination events are rare and isolated, your program is effective. If you’re seeing recurring positives in the same location, you have a design or cleaning flaw. Also, track how often you have to recall or rework batches-if that number drops after implementing monitoring, you’re succeeding.
Can ATP testing replace microbiological testing?
No. ATP measures organic residue-dirt, food, oils-which correlates with cleanliness but doesn’t confirm the presence of pathogens. Microbiological tests identify specific bacteria like Listeria or Salmonella. Use ATP for quick feedback between production runs. Use microbial tests for official compliance and root-cause analysis.
What’s the biggest mistake facilities make with environmental monitoring?
Treating it as a checklist instead of a system. Many facilities collect samples, send them to a lab, and never look at the data again. The real value is in analyzing trends, adjusting cleaning protocols, training staff based on findings, and responding to spikes. Without action, monitoring is just paperwork.

Ben Greening
December 9, 2025 AT 17:21Environmental monitoring is one of those quiet backbones of public safety that rarely gets attention-until something goes wrong. The zone system outlined here is exactly how I’ve seen it implemented in FDA-audited facilities. Zone 3 is often underestimated, but the PPD data is undeniable. Consistency in documentation, not just sampling, is what separates compliant from catastrophic.
What’s missing in most discussions is the human factor: training fatigue. Even the best protocols fail when the person swabbing is rushed, overworked, or not incentivized to care. Culture matters as much as calibration.
And yes-ATP testing is a game changer. Not a replacement, but a daily pulse check. It’s like having a fever thermometer before running a full blood panel.
Nikki Smellie
December 10, 2025 AT 13:53Let’s be honest-this entire system is a controlled illusion. The FDA doesn’t care about your swabs. They care about liability. The real contamination happens in the supply chain-raw ingredients shipped from countries with zero oversight. You can sterilize every surface in your plant, but if your milk powder comes from a farm where cows are bathed in antibiotics, your Zone 1 is already compromised.
And who’s monitoring the monitors? The lab techs? The auditors? All of them are paid by the same companies they’re supposed to police. This isn’t science-it’s theater. And the audience? We’re the ones paying for the tickets.
PS: I’ve seen the same facility pass inspection one week and shut down the next. Coincidence? I think not. :)
David Palmer
December 11, 2025 AT 01:48Bro, I work at a small food plant. We don’t have $20K for lab tests. We wipe down the slicer with bleach every shift and call it a day. The boss says we’re fine. The FDA hasn’t shown up yet. So… we’re good?
Zone 3? What’s that? The break room? Yeah, we don’t clean that till someone throws up.
ATP tester? We got a $15 Amazon gadget that blinks green. That’s our ‘tech.’
Don’t get me wrong-I want safety. But this whole thing feels like rich people’s homework for poor people’s jobs.
Doris Lee
December 12, 2025 AT 08:06This is such an important topic-and you laid it out so clearly. Thank you.
Small facilities can absolutely do this without going broke. Focus on Zone 1, use ATP for quick checks, and partner with a local lab for monthly testing. It’s not about perfection-it’s about consistency.
And hey-if you’re reading this and feeling overwhelmed? Start with one surface. One swab. One data point. Progress, not perfection. You’ve got this.
Michaux Hyatt
December 14, 2025 AT 02:49One thing people overlook: training isn’t a one-time event. It’s a ritual. We do a 10-minute huddle every Monday before shift start-review last week’s results, highlight a zone that had a spike, and let the team ask questions. It turns compliance into ownership.
Also-yes, Zone 3 is the silent killer. We had a Listeria scare last year because a forklift tire tracked in debris from the parking lot. No one thought to swab it. Now we do. Every Friday.
And ATP? Game changer. We cut our downtime by nearly half. Real-time feedback means we fix things before they become problems.
Raj Rsvpraj
December 14, 2025 AT 06:11How can you trust Western standards? In India, we have been monitoring environmental contamination for centuries-using traditional methods passed down through generations. We don’t need expensive machines or ISO classes. Our elders knew: if the air smells clean, the water is clear, and the workers are healthy-then the product is safe.
Western obsession with data is arrogance disguised as science. You measure everything… and still miss the point.
Our pharma plants use copper vessels, turmeric paste on surfaces, and sunlight exposure. No ATP. No swabs. No $25K budgets. And yet-we have zero recalls. Why? Because we respect nature, not bureaucracies.
Perhaps you should learn from us-not the other way around.
Frank Nouwens
December 15, 2025 AT 01:44Thank you for the comprehensive overview. The integration of real-time data trending under EU GMP Annex 1 is a necessary evolution. The shift from retrospective analysis to predictive modeling represents a fundamental paradigm change in quality assurance.
It is worth noting that the adoption of machine learning for contamination risk prediction is not merely a technological upgrade-it is a cultural one. Organizations must foster data literacy across all levels, from line staff to executives.
The referenced 27% reduction in false positives is statistically significant and clinically meaningful. This is not incremental improvement; it is transformational.
One final observation: the economic argument is compelling, but the ethical imperative is absolute. When lives are at stake, compliance is not a cost-it is a moral obligation.