Topical Cream Selector
Select your situation to get a recommendation:
Quick Take
- Flutivate (fluticasone) is a mid‑potency corticosteroid cream approved for eczema, psoriasis and other inflammatory skin disorders.
- Low‑potency options like hydrocortisone work well for mild flare‑ups but may need frequent re‑application.
- High‑potency choices such as clobetasol give fast relief for severe plaques but carry higher risk of skin thinning.
- Non‑steroid immunomodulators (tacrolimus, pimecrolimus) avoid steroid side effects but can cause a brief burning sensation.
- Choosing the right product hinges on potency, condition severity, treatment duration and personal tolerance.
Flutivate skin cream sits in the middle of the potency spectrum, offering a balance of effectiveness and safety for most adults with moderate eczema or psoriasis. Below we break down how it stacks up against the most common alternatives.
What is Flutivate (Fluticasone) Anyway?
Flutivate is a topical corticosteroid that contains fluticasone propionate, a synthetic glucocorticoid designed to reduce skin inflammation, itching and redness. It was FDA‑approved in 2020 for short‑term use on the face, scalp and body. The cream’s 0.05% concentration places it in the mid‑potency group, making it stronger than over‑the‑counter hydrocortisone but milder than high‑potency agents like clobetasol.
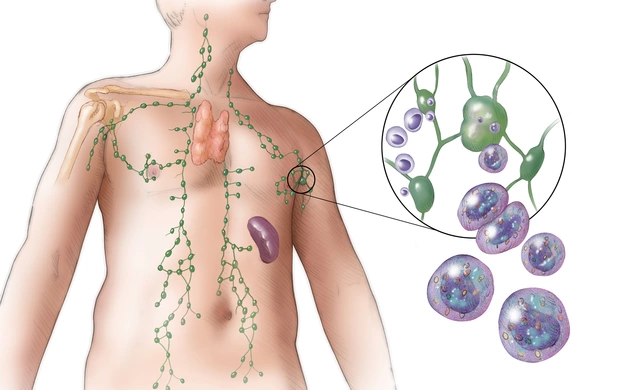
Fluticasone works by binding to glucocorticoid receptors in skin cells, switching off inflammatory genes and promoting the production of anti‑inflammatory proteins. The result is quicker symptom relief without the heavy‑dosing schedule typical of stronger steroids.
Key Factors When Comparing Topical Creams
Before diving into the side‑by‑side table, keep these five criteria in mind:
- Potency level - Low, medium or high; dictates how quickly symptoms improve and the risk of side effects.
- Active ingredient - Determines the drug class (corticosteroid vs. calcineurin inhibitor) and mechanism of action.
- Prescription requirement - Over‑the‑counter (OTC) versus prescription can affect accessibility and cost.
- Typical use case - Acute flare‑ups, maintenance therapy, facial skin, or thick plaques.
- Safety profile - Potential for skin atrophy, telangiectasia, systemic absorption, or allergic reactions.

Side‑by‑Side Comparison Table
| Product | Active Ingredient | Potency | Prescription Needed? | Typical Indication |
|---|---|---|---|---|
| Flutivate | Fluticasone propionate (0.05%) | Medium | Yes | Eczema, psoriasis, seborrheic dermatitis |
| Hydrocortisone 1% | Hydrocortisone | Low | No (OTC) | Mild eczema, insect bites, rash |
| Triamcinolone Acetonide 0.1% | Triamcinolone | Medium‑high | Yes | Moderate‑severe eczema, psoriasis plaques |
| Mometasone Furoate 0.1% | Mometasone | Medium‑high | Yes | Body & scalp psoriasis, chronic dermatitis |
| Clobetasol Propionate 0.05% | Clobetasol | Very high | Yes | Severe plaque psoriasis, lichen planus |
| Tacrolimus 0.1% Ointment | Tacrolimus | Non‑steroid | Yes | Atopic dermatitis, sensitive‑area eczema |
| Pimecrolimus 1% Cream | Pimecrolimus | Non‑steroid | Yes | Facial & intertriginous eczema |
| Betamethasone Dipropionate 0.05% | Betamethasone | High | Yes | Thick plaques, chronic eczema |
Deep Dive into the Most Common Alternatives
Hydrocortisone is a low‑potency corticosteroid often sold as a 1% cream or ointment for over‑the‑counter use. It’s gentle enough for the face and infants, but you’ll usually need to apply it two to three times daily for a week or more to see relief. Because it’s mild, skin thinning is rare, but the trade‑off is slower itch control.
Triamcinolone Acetonide is a medium‑high potency steroid commonly prescribed as a 0.1% cream for stubborn dermatitis and psoriasis plaques. Patients typically use it once or twice daily for up to two weeks. It can reduce inflammation faster than hydrocortisone but carries a higher chance of localized thinning if used beyond the recommended period.
Mometasone Furoate offers a medium‑high potency profile with strong anti‑inflammatory action while keeping systemic absorption low. Its 0.1% formulation is popular for scalp psoriasis because it spreads easily and doesn’t leave a greasy residue.
Clobetasol Propionate is a very high‑potency steroid reserved for short, intensive bursts on severe plaques or hyperkeratotic lesions. Doctors often limit use to two weeks to avoid permanent skin changes. It’s not for the face or intertriginous zones.
Tacrolimus belongs to the calcineurin inhibitor class, providing anti‑inflammatory effects without steroid‑related skin atrophy. The 0.1% ointment works best for sensitive areas like the eyelids or groin, though users may notice a transient burning sensation for the first few days.
Pimecrolimus is another non‑steroidal immunomodulator, formulated as a 1% cream specifically for facial and intertriginous eczema. Its safety profile allows for longer‑term use, but like tacrolimus, it can cause mild irritation at the start of therapy.
Betamethasone Dipropionate is a high‑potency steroid often used for thick, chronic plaques where lower‑strength agents fail. It’s effective but must be cycled with non‑steroid moisturizers to mitigate thinning.
Safety, Side Effects, and Practical Tips
All topical steroids share a core risk set: skin atrophy, telangiectasia, striae, and potential suppression of the hypothalamic‑pituitary‑adrenal (HPA) axis when large areas are treated for weeks. The likelihood rises with potency, treatment length, and the age of the patient. Here’s a quick cheat‑sheet:
- Low‑potency (hydrocortisone) - minimal atrophy, safe for face and children.
- Medium (Flutivate, triamcinolone, mometasone) - moderate risk; limit continuous use to 2‑4 weeks on any single site.
- High‑potency (betamethasone, clobetasol) - higher atrophy risk; use short bursts, rotate with moisturizers.
- Non‑steroid (tacrolimus, pimecrolimus) - no skin thinning, but watch for burning, especially in winter.
When you’re on a steroid, always pair it with an emollient. A good moisturizer restores barrier function, reduces rebound itching once the steroid is tapered, and can sometimes allow you to lower the steroid strength.
Choosing the Right Product for Your Situation
Think of the decision as a three‑step flow:
- Assess severity and location. Mild hand eczema = hydrocortisone. Moderate facial dermatitis = Flutivate or tacrolimus (if you’re steroid‑averse).
- Consider duration. Short flare‑ups (<2 weeks) can tolerate medium potency; chronic maintenance benefits from low‑potency or non‑steroid agents.
- Weigh side‑effect tolerance. If you’ve had skin thinning before, steer clear of high‑potency steroids and explore calcineurin inhibitors.
In practice, many dermatologists follow a “step‑down” protocol: start with a medium‑potency cream like Flutivate for rapid control, then transition to a low‑potency steroid or moisturizer as symptoms improve. This approach maximizes relief while minimizing long‑term risks.

Frequently Asked Questions
Can I use Flutivate on my face?
Yes. Flutivate’s mid‑potency makes it safe for short‑term facial use, but limit application to once daily and no longer than 2‑4 weeks without a doctor’s guidance.
How does Flutivate compare to over‑the‑counter hydrocortisone?
Flutivate is stronger, so it reduces redness and itch faster. Hydrocortisone is gentler, better for very mild rashes or for daily maintenance after a steroid course.
Are there any drug interactions with Flutivate?
Topical steroids have minimal systemic interaction, but using large amounts over broken skin can increase systemic absorption. Discuss with your doctor if you’re on oral corticosteroids or have liver/kidney disease.
What should I do if I notice skin thinning while using a steroid?
Stop the steroid immediately and switch to a non‑steroidal moisturizer or a calcineurin inhibitor like tacrolimus. Consult a dermatologist to assess the extent of atrophy.
Is it safe to use tacrolimus and a steroid together?
Usually not recommended on the same spot because it can increase irritation. Some doctors alternate: steroid for a few days, then tacrolimus on off‑days.
Bottom line: Flutivate offers a sweet spot for many adults battling moderate eczema or psoriasis. If you need something milder, reach for hydrocortisone; if the rash is severe, consider a higher‑potency steroid or a non‑steroidal immunomodulator. Always pair any active treatment with a good moisturizer, and consult your healthcare provider before starting a new regimen.





Ellie Chung
September 28, 2025 AT 22:06Holy smokes, this cream sounds like the superhero cape your skin’s been begging for!
Sophia Simone
September 28, 2025 AT 22:15While the enthusiasm is noted, one must acknowledge that the comparative matrix presented is marred by a lack of rigorous statistical validation, rendering the purported superiority of Flutivate a speculative assertion rather than an evidence‑based conclusion.
Juan Sarmiento
September 28, 2025 AT 22:40I get where you’re coming from, and I’ve walked that tightrope between steroid relief and the dreaded skin thinning more times than I care to admit. First, let’s paint the picture: you’ve got a flare that’s itching like a hundred tiny fireworks, and you reach for that tube of Flutivate hoping for calm. The good news is that fluticasone’s medium potency does a solid job of dousing the flames without shouting “danger!” to the rest of your body. Second, remember that consistency is king; applying a thin layer twice daily for the prescribed two‑week window often yields noticeable dimming of redness within just a few days. Third, never underestimate the power of a good moisturizer; slathering one on after the steroid helps restore barrier function and can actually prolong the benefits of the medication. Fourth, keep an eye on the treatment site – if you start noticing thin patches, stretch marks, or persistent bruising, it’s time to taper off and consider a non‑steroidal alternative. Fifth, don’t let the fear of side effects keep you from using the cream when you truly need it; short, targeted bursts are generally safe for most adults. Sixth, if your skin is particularly sensitive, you might opt for tacrolimus or pimecrolimus, but be prepared for that initial burning sensation that usually fades. Seventh, make sure to rotate the medication with a steroid‑free regimen after the initial course; this prevents your skin from becoming too accustomed to the drug. Eighth, keep the application area clean and dry before putting on the cream – sweat and moisture can dilute its effectiveness. Ninth, educate yourself on the potency ladder; knowing that hydrocortisone is low and clobetasol is very high helps you make informed choices. Tenth, always have a backup plan – a low‑potency steroid or an OTC barrier cream can bridge the gap between prescription refills. Eleventh, communicate with your dermatologist; they can tailor the tapering schedule to your specific skin type and flare pattern. Twelfth, if you notice any systemic symptoms like unexplained weight gain or mood swings, seek medical advice promptly. Thirteenth, remember that lifestyle factors – stress, diet, sleep – can amplify or dampen skin inflammation, so treat your whole body, not just the rash. Fourteenth, keep a journal of what works and what doesn’t; over time you’ll develop a personal protocol that feels like a second skin. Finally, celebrate the small victories – a night of restful sleep without scratching is a triumph worth savoring.
Patrick McVicker
September 28, 2025 AT 22:48Spot on, man! You nailed the whole “apply a thin layer” thing – it’s basically the Goldilocks rule for steroids. Just a heads‑up though: instead of “slathering one on after the steroid,” it’s smoother to say “apply a moisturizer after the steroid” for clarity. Keep it up, and your skin will thank you 😊.
Liliana Phera
September 28, 2025 AT 22:56If we strip away the marketing fluff, the real battle is between a fleeting numbing of symptoms and the long‑term erosion of self‑respect that comes from ceding control to a chemical crutch; embracing non‑steroidal options isn’t just a medical choice, it’s a declaration of autonomy against the tyranny of quick fixes.