Most people with diabetes assume that if their insulin shot stings a little or leaves a red bump, it’s just normal. But what if that redness doesn’t fade? What if your arm swells up hours later, or you suddenly feel dizzy after injecting? These aren’t just side effects-they could be signs of an insulin allergy.
Insulin allergies are rare. Only about 2.1% of people using insulin report true allergic reactions, according to the Independent Diabetes Trust. But even though they’re uncommon, they can be serious. Left unchecked, they can lead to anaphylaxis-a life-threatening response that shuts down breathing. And here’s the scary part: many people stop taking insulin because they think the reaction means they’re allergic to the drug itself. That’s dangerous. Stopping insulin can trigger diabetic ketoacidosis, which can kill you faster than the allergy.
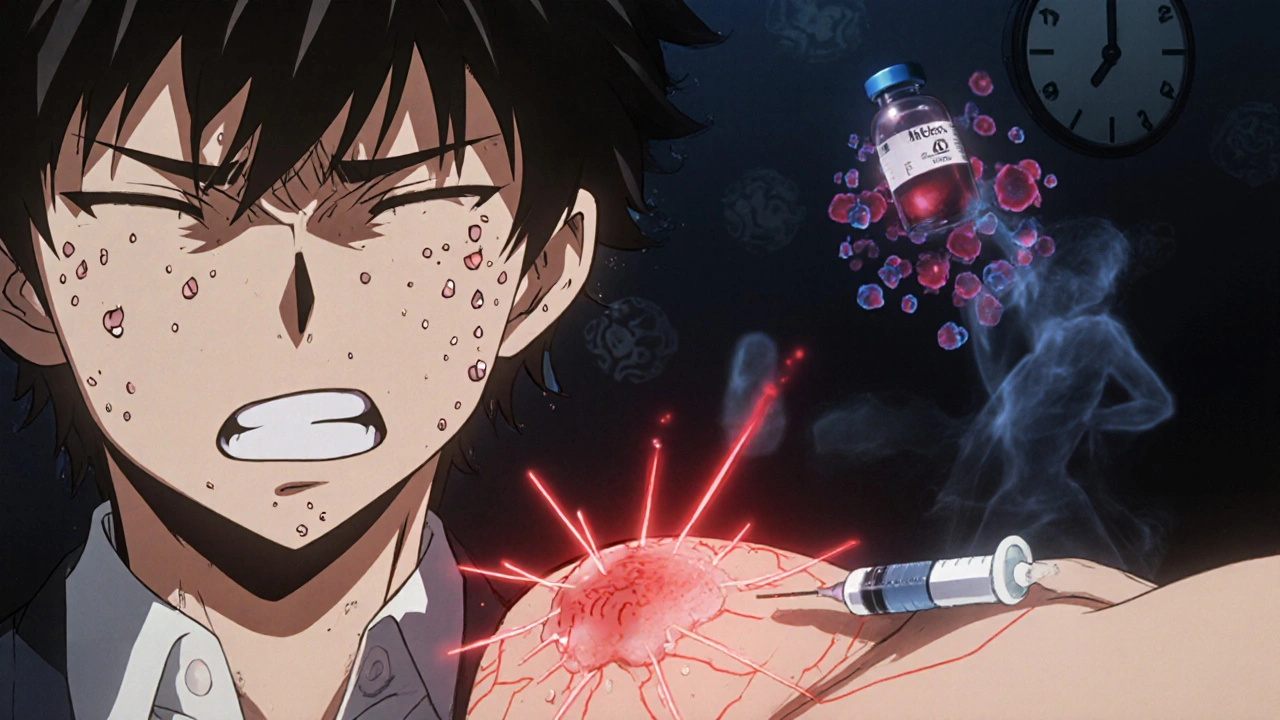
What Does an Insulin Allergy Actually Look Like?
Not all reactions are the same. There are three main types, and they look very different.
Localized reactions are the most common-about 97% of all insulin allergies fall into this category. These happen right at the injection site. You’ll notice redness, swelling, itching, or a small lump that feels tender to the touch. It might show up 30 minutes after your shot, or it might wait until 6 hours later. These bumps can turn into hard nodules under the skin. Most of the time, they go away on their own in 1-2 days. But if they keep coming back in the same spot, or if they spread beyond the injection area, that’s a red flag.
Systemic reactions are rare-less than 0.1% of insulin users-but they’re emergencies. These aren’t just skin deep. You might break out in hives all over your body. Your lips, tongue, or throat could swell. You might feel your chest tighten, your breathing get shallow, or your blood pressure drop. This is anaphylaxis. It doesn’t wait. It hits fast. If you’ve ever had a severe bee sting reaction, this feels similar. You need help now.
Delayed reactions are the sneaky ones. They can show up hours-or even days-after your injection. Think joint pain, muscle aches, or bruising that looks like a bad bump but doesn’t fade for two weeks. These aren’t caused by IgE antibodies like typical allergies. Instead, they’re T-cell driven. That means they’re not the kind you can fix with an antihistamine. And they can appear even after you’ve been on the same insulin for 10 years. No warning. No pattern. Just one day, your body says, “Enough.”
Is It Really the Insulin-or Something Else?
Here’s something most people don’t know: you might not be allergic to insulin at all. You could be reacting to the additives.
Insulin isn’t pure. It’s mixed with preservatives like metacresol and zinc to keep it stable. Some brands, like Humalog, have higher levels of metacresol. If your skin reacts every time you use that pen-but not with another brand-it’s probably not the insulin molecule. It’s the chemical sitting beside it.
That’s why switching insulin types works for about 70% of people with allergic reactions. If you’ve been on NovoLog and start breaking out, try switching to Lantus or Tresiba. Different formulation. Different additives. Often, the problem disappears. But you can’t just swap on your own. You need guidance.
And don’t confuse allergy symptoms with low blood sugar. Shaking, sweating, anxiety-those are hypoglycemia. They’re common. They’re not allergic. If you’re not sure, check your glucose. If it’s normal and you’re still reacting, it’s likely the immune system, not the sugar.
What Should You Do If You React?
First: don’t stop injecting insulin. That’s the biggest mistake people make. Even if you’re scared, keep going. Your body needs insulin to survive. Instead, call your diabetes team immediately. They’ll help you figure out what’s happening and how to stay safe.
If you’re having a systemic reaction-swelling in your throat, trouble breathing, dizziness, or passing out-call emergency services right away. In Australia, that’s 000. Don’t drive yourself. Don’t wait. Anaphylaxis can kill in minutes. If you have an epinephrine auto-injector (like an EpiPen), use it. Even if you’re not sure, better safe than sorry.
For localized reactions, your doctor might suggest antihistamines like cetirizine or loratadine. These help with itching and swelling. Steroids-either oral or topical-can calm down the immune response. For stubborn nodules, applying a mid-to-high potency corticosteroid cream (like flunisolide 0.05%) right after injection, then again 4-6 hours later, can prevent the bump from forming.
For delayed reactions, topical calcineurin inhibitors like tacrolimus or pimecrolimus are often more effective than steroids. These work differently-they calm T-cells instead of suppressing inflammation broadly. They’re prescription-only, but they’re a game-changer for people who’ve been stuck with recurring joint pain or bruising.

Can You Get Used to It? Desensitization Explained
If you’re allergic but still need insulin, there’s a path forward: desensitization.
This isn’t magic. It’s science. Under strict medical supervision, you’re given tiny, increasing doses of the insulin you’re allergic to-over hours or days-until your body stops reacting. It sounds risky, but it works. In one study, 66.7% of patients had their symptoms completely resolved after desensitization. The rest saw major improvement.
This process has to happen in a hospital or allergy clinic. You can’t do it at home. You need monitors, emergency meds, and trained staff nearby. But once you’re through it, many people can go back to their regular insulin without problems.
And here’s the kicker: some people who’ve been allergic for years have been successfully desensitized-even after using insulin for over a decade. It’s not about how long you’ve had it. It’s about how you handle it.
How Do Doctors Know It’s an Allergy?
It’s not just guessing. There’s a real diagnostic process.
First, your doctor will ask you to track everything: when you injected, what type of insulin, where on your body, what symptoms showed up, and how long they lasted. Patterns matter. If every time you use insulin glargine, you get swelling on your thigh, that’s data.
Then comes testing. Skin prick tests or intradermal tests are the gold standard. A tiny amount of the insulin is placed under your skin. If you react, you’ll get a red, itchy bump. Blood tests can check for IgE antibodies specific to insulin or its additives.
But here’s what many doctors miss: they test for insulin and forget the excipients. Make sure your allergist tests the preservatives too-metacresol, zinc, phenol. Sometimes, the solution isn’t changing insulin. It’s changing the brand.

What If Nothing Works?
For a small group-about 25% of cases in one study-switching to oral diabetes medications is the answer. But that’s only possible if you have type 2 diabetes. If you’re type 1, your pancreas doesn’t make insulin. You can’t survive without it. For those patients, the options are limited: desensitization, switching insulin types, or using newer analogs with cleaner formulations.
Newer insulins like Fiasp or Toujeo have fewer additives and lower immunogenicity. That means less chance of triggering a reaction. If you’ve tried everything else, ask your doctor about switching to one of these. It might be the solution you didn’t know existed.
What You Need to Remember
Insulin allergies are rare. But they’re real. And they’re treatable.
You don’t have to live with itchy bumps every day. You don’t have to fear your next injection. You don’t have to stop taking insulin.
Work with your diabetes team and an allergist. Track your reactions. Get tested. Try a different brand. Consider desensitization. Use the right creams. Know the signs of an emergency.
Most people who face this problem go on to manage their diabetes just fine. They just needed the right help at the right time.
Don’t ignore it. Don’t power through it. Don’t quit insulin. Get help. Your life depends on it.

Ellen Calnan
November 19, 2025 AT 06:57I used to get these nasty nodules every time I injected in my thigh-like little marble bumps that lasted weeks. I thought it was just bad technique until my endo referred me to an allergist. Turns out, it wasn’t the insulin-it was the metacresol in my brand. Switched to Tresiba and poof. No more lumps. No more anxiety before shots. If you’re dealing with this, don’t just power through. Get tested. Your skin deserves better.
Paige Lund
November 20, 2025 AT 08:27So… you’re telling me I’ve been scared of my own insulin for years because of a red bump? Cool. I’ll just keep ignoring it then.
Reema Al-Zaheri
November 22, 2025 AT 07:01This is incredibly important information. I have a cousin in Mumbai who stopped insulin after developing hives-she thought she was allergic to the drug itself. She ended up in the hospital with DKA. Please, if you're reading this and you're experiencing any reaction, no matter how 'minor'-seek professional help immediately. This isn't just about comfort; it's about survival.
Derron Vanderpoel
November 22, 2025 AT 21:46I had the delayed reaction thing-joint pain for 3 weeks after every shot. No swelling, no redness, just… my knees felt like they were filled with gravel. My doctor laughed at first. Said it was ‘just aging.’ Then I showed him this article. He ordered a T-cell panel. Turns out it was the insulin. We switched brands. Within 10 days, I could walk again. I didn’t even know this was a thing. Thank you for writing this.
Michael Petesch
November 24, 2025 AT 07:02It is worth noting that the prevalence of true IgE-mediated insulin allergies is indeed low, as cited by the Independent Diabetes Trust. However, the underdiagnosis of non-IgE-mediated reactions-particularly T-cell-driven delayed hypersensitivity-remains a significant clinical blind spot. Many primary care providers lack the training to recognize these patterns, leading to unnecessary insulin discontinuation or misattribution to other etiologies. A multidisciplinary approach involving endocrinology and immunology is imperative for accurate diagnosis and management.
Christopher Robinson
November 24, 2025 AT 20:48Big thank you for this. I’ve been on Lantus for 8 years and just started getting these weird bruises that wouldn’t fade. Thought it was just thin skin. Now I know it’s probably the preservatives. I’m switching to Fiasp next week 🙌
Michael Salmon
November 25, 2025 AT 09:10Wow. Another fear-mongering article from the insulin industry. You know what’s really dangerous? The fact that Big Pharma makes billions off people being scared of their own medicine. Why don’t you ask why insulin costs $300 a vial while the raw molecule costs $6? Maybe your ‘allergy’ is just your body screaming at the price gouging.
Joe Durham
November 26, 2025 AT 14:28I get what you’re saying about not stopping insulin-but I also think we need to talk about how scary it is to inject something that makes you feel like you’re dying. I’ve had two systemic reactions. I carry two EpiPens. I still shake before every shot. It’s not just a medical issue-it’s a trauma. If you’re going through this, you’re not alone. Talk to someone. Even if it’s just a Reddit thread.
Sam Reicks
November 27, 2025 AT 15:38So insulin is causing allergies but the government says its safe? Funny how that works. You ever hear of the Tuskegee experiment? Or the Vioxx scandal? They said it was safe too. They’re lying to you. The additives? Totally manufactured. The whole system is rigged. I stopped insulin and started eating raw garlic and moon water. My sugar’s better now. Also my dog says I’m healed.
Codie Wagers
November 27, 2025 AT 23:12You speak of desensitization as if it were a benevolent medical intervention. But let us not forget: the body does not ‘adapt’ to poison. It submits. You are not overcoming an allergy-you are conditioning your immune system to tolerate a foreign invader. Is this healing? Or is it surrender? The insulin molecule is not your friend. It is a synthetic mimic, a corporate construct masquerading as salvation. Your pancreas was not broken. It was abandoned.
Christopher K
November 28, 2025 AT 16:13Y’all are so weak. Back in my day, we didn’t have ‘delayed reactions’ or ‘additives’-we had insulin made from pigs and we took it like men. No antihistamines. No T-cell panels. Just grit. Now we got millennials crying because their arm itches. Get a grip. You’re not allergic-you’re entitled.
James Ó Nuanáin
November 30, 2025 AT 04:24As a British endocrinologist with over 27 years of clinical experience, I must commend the precision of this article. The delineation between localized, systemic, and delayed hypersensitivity reactions is clinically impeccable. However, I must note that the prevalence figures cited are drawn from North American cohorts-European populations exhibit significantly lower rates of IgE-mediated reactions due to differing preservative formulations. That said, the recommendation to test for excipients remains paramount. I have personally managed 14 cases of metacresol hypersensitivity in the past decade. Always test the excipients. Always.
Kara Binning
November 30, 2025 AT 23:16Oh my god. I’ve been getting these ‘bruises’ for 5 years and thought I was just clumsy. I’ve been injecting in my belly and now I’m terrified to look at my skin. I’m going to cry in the shower. Thank you for this. I feel less alone. Also I’m switching to Toujeo. And maybe therapy. Definitely therapy.
river weiss
December 1, 2025 AT 09:41To anyone reading this who’s scared: you’re not broken. You’re not weak. You’re not failing. You’re just navigating a system that rarely talks about the emotional toll of chronic illness. The fact that you’re here, reading this, trying to understand-this is strength. Please, reach out to your care team. Ask for a referral to an allergist. Bring this article. You deserve to live without fear every time you pick up your pen.
Timothy Reed
December 3, 2025 AT 02:59Thank you for the thorough breakdown. I’ve been a diabetes educator for 15 years and see patients dismiss these reactions all the time. I always emphasize: ‘It’s not ‘just a bump.’ It’s your body’s language.’ If you’re having a reaction, it’s not in your head. It’s real. And there are solutions. You’re not alone. I’ve seen patients go from terrified to thriving-just by switching brands or getting desensitized. It’s not magic. It’s medicine. And you deserve it.