Cephalexin vs. Antibiotic Alternatives Comparison Tool
Recommended Antibiotics
Quick Take
- Cephalexin (Phexin) is a first‑generation cephalosporin best for skin, bone and urinary infections.
- Amoxicillin offers a broader gram‑negative reach but shares a similar allergy profile.
- Dicloxacillin is ideal for penicillin‑resistant Staphylococcus aureus (MRSA‑susceptible strains).
- Clindamycin covers anaerobes and some MRSA but can cause serious gut issues.
- Azithromycin is a macrolide useful for atypical pathogens and is often taken once‑daily.
What is Cephalexin (Phexin)?
When doctors prescribe Cephalexin (Phexin), they are giving a first‑generation cephalosporin that attacks the bacterial cell wall. It’s approved in the UK and US for uncomplicated skin, bone and urinary tract infections, plus ear‑nose‑throat (ENT) infections. The drug is taken orally, comes in 250mg and 500mg tablets, and usually runs for 5‑10days depending on the infection severity.
How does it work?
Cephalexin binds to penicillin‑binding proteins (PBPs) inside the bacterial cell wall. This stops the wall from cross‑linking, leading to cell lysis. Because it targets PBPs found mostly in gram‑positive organisms, the drug is especially powerful against Staphylococcus aureus (non‑MRSA) and Streptococcus species.
When would you actually need Cephalexin?
Typical indications include:
- Cellulitis or impetigo (skin infections)
- Osteomyelitis (bone infection) caused by susceptible bacteria
- Uncomplicated urinary tract infection (UTI) caused by Escherichia coli that is still sensitive
- Middle ear infections (otitis media) in children
If the culture shows a gram‑negative rod resistant to cephalosporins, you’ll need a different class.
Key criteria for comparing antibiotics
When you line up alternatives, keep these factors front‑and‑center:
- Spectrum of activity - Does it cover the likely bug?
- Allergy cross‑reactivity - Cephalosporins share a 10‑15% cross‑allergy risk with penicillins.
- Dosage convenience - Once‑daily vs. thrice‑daily can affect adherence.
- Side‑effect profile - GI upset, C.difficile risk, liver impact.
- Cost & availability in the UK - NHS prescription charge or private price.
Top alternatives to Cephalexin
Below are the most common competitors you’ll see on a GP prescription pad.
Amoxicillin
Amoxicillin is a broad‑spectrum penicillin that tackles many gram‑negative organisms that Cephalexin can miss. It’s the go‑to for sinusitis, bronchitis and some UTIs. Dose: 500mg three times daily for adults.
Dicloxacillin
Dicloxacillin is a penicillinase‑resistant penicillin, meaning it can handle beta‑lactamase‑producing Staphaureus (non‑MRSA). It’s used for skin infections when a penicillin allergy is not an issue. Dose: 250‑500mg four times daily.
Clindamycin
Clindamycin is a lincosamide that covers anaerobes and many MRSA strains. It’s a good rescue drug for deep‑tissue infections but comes with a higher chance of causing C.difficile colitis. Dose: 300mg three times daily.
Azithromycin
Azithromycin is a macrolide with excellent tissue penetration and a simple once‑daily regimen (500mg day1, then 250mg days2‑5). It’s useful for atypical pathogens (like Mycoplasma) and for patients who can’t take beta‑lactams. Side effects are usually mild GI upset.
Penicillin V
Penicillin V is an older narrow‑spectrum option perfect for streptococcal throat infections. It’s cheap and well‑tolerated but should be avoided if you’re allergic to any beta‑lactam.
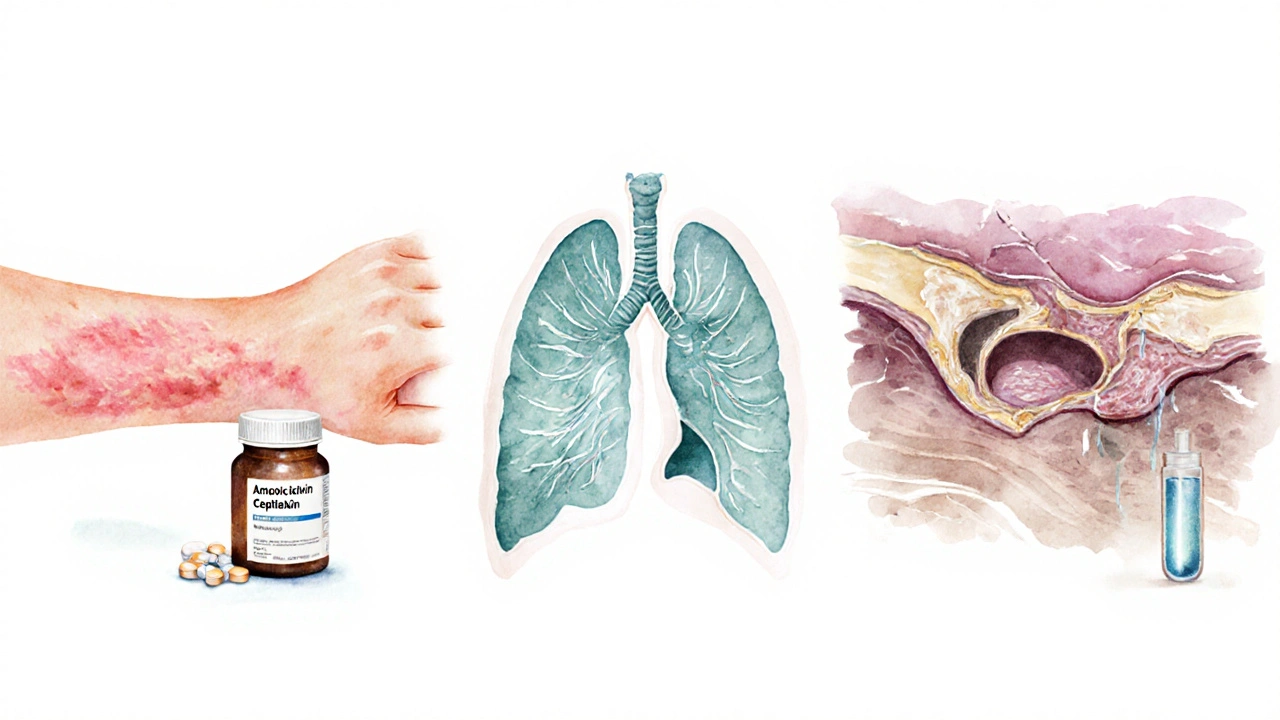
Side‑effect snapshot
All antibiotics can cause nausea, diarrhoea and rash, but the likelihood varies:
- Cephalexin: mild GI upset (5‑10%); rare rash; low C.difficile risk.
- Amoxicillin: higher rash rate in penicillin‑allergic patients.
- Dicloxacillin: similar to other penicillins.
- Clindamycin: up to 10% risk of C.difficile colitis.
- Azithromycin: minimal GI upset, occasional QT‑prolongation.
Cost comparison (2025 NHS pricing)
| Antibiotic | Typical adult dose | Gram‑positive coverage | Gram‑negative coverage | UK prescription charge* |
|---|---|---|---|---|
| Cephalexin | 500mg 3×day | Excellent | Limited | £9.35 (standard) |
| Amoxicillin | 500mg 3×day | Good | Broad | £9.35 |
| Dicloxacillin | 500mg 4×day | Very good (beta‑lactamase resistant) | Moderate | £9.35 |
| Clindamycin | 300mg 3×day | Excellent (including MRSA) | Limited | £9.35 + possible extra monitoring |
| Azithromycin | 500mg day1, then 250mg days2‑5 | Good | Good (atypical) | £9.35 |
*Standard NHS prescription charge for adults as of October2025.
Decision guide: Which antibiotic fits your situation?
Use this quick flow:
- If the infection is confirmed skin‑cellulitis caused by MSSA, Cephalexin or Dicloxacillin are first‑line.
- For sinusitis or bronchitis where Haemophilus or Morganella may be involved, switch to Amoxicillin.
- If you have a documented beta‑lactam allergy, Azithromycin or Clindamycin become attractive options.
- When MRSA is likely (e.g., post‑surgical wound), Clindamycin or a specialist‑prescribed linezolid is safer.
- Consider cost and dosing convenience for elderly patients - a once‑daily Azithromycin course often wins adherence.
Always discuss culture results with your GP; they’ll tailor the choice to local resistance patterns (the UK’s 2024 “ESKAPE” surveillance shows rising cephalosporin‑resistance in hospital‑acquired Staphaureus).
Safety considerations and drug interactions
All beta‑lactams can trigger a rash in patients with a penicillin allergy. Cephalexin’s cross‑reactivity sits around 5‑10% - a modest risk but worth flagging. Warfarin patients should get INR checks when starting any antibiotic, especially Clindamycin, which can potentiate anticoagulation.
Pregnant or breastfeeding women usually tolerate Cephalexin and Amoxicillin, but macrolides like Azithromycin need a doctor’s green light for the first trimester.
How resistance is shaping choices
Antibiotic resistance isn’t static. The UK’s 2023 report on antibiotic resistance notes a 12% rise in cephalosporin‑non‑susceptible Staph isolates. That makes clinicians more cautious about prescribing Cephalexin for empiric therapy unless the infection is clearly skin‑derived and culture‑proven.
In contrast, macrolide resistance in respiratory pathogens remains under 5% in England, keeping Azithromycin a viable backup when beta‑lactams are ruled out.
Bottom line
Cephalexin (Phexin) remains a solid, affordable option for uncomplicated gram‑positive infections. If you need broader coverage, have a beta‑lactam allergy, or are dealing with MRSA‑suspected disease, you’ll likely move to Amoxicillin, Dicloxacillin, Clindamycin, or Azithromycin based on the criteria above.

Frequently Asked Questions
Can I take Cephalexin if I’m allergic to penicillin?
There is a 5‑10% cross‑reactivity risk. Most doctors will perform an allergy test or choose a non‑beta‑lactam like Azithromycin if the allergy is severe.
What’s the main advantage of Dicloxacillin over Cephalexin?
Dicloxacillin resists beta‑lactamase enzymes, so it works better against penicillinase‑producing Staph strains that might shrug off Cephalexin.
Why would a doctor prescribe Clindamycin instead of Cephalexin?
Clindamycin covers anaerobes and many MRSA strains, making it the go‑to for deep‑tissue or post‑surgical infections when gram‑positive coverage alone isn’t enough.
Is Azithromycin safe for children?
Yes, the pediatric dose is weight‑based (10mg/kg on day1, then 5mg/kg daily). It’s often used for ear infections when a beta‑lactam isn’t tolerated.
How do I know if my infection is resistant to Cephalexin?
Your GP may send a swab for culture and sensitivity. If the lab reports “Cephalexin‑resistant,” they’ll switch you to a more appropriate drug.





Tiarna Mitchell-Heath
October 1, 2025 AT 12:52Right off the bat, Cephalexin isn’t the miracle drug the pharma press wants you to think; it’s just another beta‑lactam with a narrow playbook. If you’re not careful, you’ll end up with a resistant infection faster than you can finish the prescription.
Katie Jenkins
October 3, 2025 AT 08:52Firstly, the article mistakenly capitalises “Cephalexin” as “Phexin” in several places – that’s an error; the correct trade name is Phexin, but the generic is Cephalexin. Also, the dosage recommendations omit the essential weight‑based adjustments for paediatrics, which is a serious oversight in any clinical guide.
Jack Marsh
October 5, 2025 AT 04:52While many laud cephalexin’s low side‑effect profile, the data on C. difficile risk is not negligible; consider the epidemiological numbers from 2023 showing a 3‑% incidence even with first‑generation cephalosporins.
Steven Waller
October 7, 2025 AT 00:52Think of antibiotic selection as a balance between spectrum and stewardship. Cephalexin shines for uncomplicated skin infections, but once you suspect polymicrobial or anaerobic involvement, expanding coverage responsibly is essential.
Puspendra Dubey
October 8, 2025 AT 20:52Yo, so like, imagine you’re in a drama where the hero picks Cephalexin for a busted skin wound, but the villain’s bacteria are secretly MRSA‑savvy. That plot twist would force a switch to clinda or even linezolid – cue the epic music!
It’s a classic case of underestimating the enemy.
Shaquel Jackson
October 10, 2025 AT 16:52Honestly, the guide glazes over the real cost of clindamycin‑induced colitis – that’s a lazy omission.
Tom Bon
October 12, 2025 AT 12:52I appreciate the thoroughness of the comparison; the side‑effect tables are especially helpful for clinicians balancing patient compliance.
Clara Walker
October 14, 2025 AT 08:52Did you know the Big Pharma lobby pushed the NHS to list Cephalexin as first‑line despite rising resistance? The hidden agenda is clear when you dig into the 2024 funding disclosures.
Jana Winter
October 16, 2025 AT 04:52Your article’s grammar is riddled with commas splicing clauses; a well‑written medical guide would not stumble over basic punctuation.
Linda Lavender
October 18, 2025 AT 00:52When we embark upon the grand odyssey of antimicrobial selection, one must first acknowledge the historical tapestry from which cephalexin emerged, a first‑generation cephalosporin birthed in the crucible of mid‑twentieth‑century pharmaceutical innovation.
Its molecular architecture, a β‑lactam ring fused to a dihydrothiazine moiety, confers a predilection for gram‑positive cocci, rendering it a stalwart ally against Staphylococcus aureus strains devoid of methicillin resistance.
Yet, the narrative does not end in triumph; the relentless march of bacterial evolution has furnished us with β‑lactamase enzymes capable of hydrolysing the very backbone that bestows cephalexin its potency.
Consequently, clinicians must weigh the specter of resistance, especially within nosocomial settings where the prevalence of cephalosporin‑non‑susceptible Staphylococci has risen by double‑digit percentages in recent surveillance reports.
In juxtaposition, the drug’s pharmacokinetic profile-characterised by rapid absorption and a half‑life conducive to thrice‑daily dosing-offers a pragmatic advantage in outpatient regimens, fostering adherence compared to agents requiring more frequent administration.
The side‑effect spectrum remains relatively benign, with gastrointestinal upset in a minority of patients and a low incidence of Clostridioides difficile colitis, though vigilance remains paramount given the potential for dysbiosis.
From an economic perspective, the NHS price point of £9.35 per prescription underscores its affordability, yet this metric must be balanced against downstream costs incurred by treatment failures or resistance-driven escalations to broader‑spectrum agents.
Moreover, the cross‑reactivity with penicillin, estimated at 5‑10 %, demands a thorough allergy assessment, as inappropriate exposure may precipitate hypersensitivity reactions in susceptible individuals.
Alternative agents such as amoxicillin, dicloxacillin, clindamycin, and azithromycin each inhabit distinct niches within the antimicrobial armamentarium, offering expanded gram‑negative coverage, β‑lactamase resistance, anaerobic efficacy, or convenient dosing schedules respectively.
For instance, amoxicillin’s broader gram‑negative reach makes it suitable for sinusitis and bronchitis, whereas clindamycin’s activity against anaerobes and certain MRSA strains renders it indispensable in deep‑tissue infections, despite its heightened C. difficile risk.
Azithromycin’s pharmacodynamic convenience-once‑daily dosing over a five‑day course-enhances patient compliance, particularly among pediatric populations where adherence challenges are pronounced.
In clinical decision‑making, a judicious algorithm incorporating infection site, microbiological data, patient allergies, and pharmacoeconomic considerations will invariably yield superior outcomes.
Thus, while cephalexin retains a venerable position within the therapeutic hierarchy for uncomplicated gram‑positive infections, its role must be continually re‑evaluated against the evolving backdrop of antimicrobial resistance, patient-specific factors, and emerging evidence.
Jay Ram
October 19, 2025 AT 20:52Great rundown! Remember to keep the dosing simple for patients; a clear schedule can dramatically boost treatment success.
shikha chandel
October 21, 2025 AT 16:52Cephalexin isn’t a universal fix; consider resistance patterns before prescribing.
Mary Ellen Grace
October 23, 2025 AT 12:52Thanks for the clear tables! The side‑effect list helped me explain to my mom why we might avoid clindamycin.
Kelly Larivee
October 25, 2025 AT 08:52Cephalexin works well for skin infections, but if you have a penicillin allergy, azithromycin is a good alternative.
Emma Rauschkolb
October 27, 2025 AT 03:52From a pharmacodynamics standpoint, the time‑dependent killing of beta‑lactams like cephalexin necessitates maintaining serum concentrations above MIC; sub‑therapeutic troughs can precipitate resistance-a classic case of PK/PD mismanagement.
Landmark Apostolic Church
October 28, 2025 AT 23:52Philosophically, the choice of an antibiotic reflects a broader societal contract: we trust physicians to steward microbes responsibly, yet we must also demand transparency about pharmaceutical influences.
Matthew Moss
October 30, 2025 AT 19:52It is imperative that our national healthcare policy prioritises the use of cost‑effective, evidence‑based antibiotics such as Cephalexin, thereby safeguarding our citizens from unnecessary foreign drug dependence.
Antonio Estrada
November 1, 2025 AT 15:52I concur with the prior comment; integrating local resistance data into prescribing protocols will enhance outcomes and limit collateral damage.
Andy Jones
November 3, 2025 AT 11:52Oh sure, because a 2025 guide magically solves all your antibiotic dilemmas-next they’ll write a guide on how to perfectly time your Netflix binge.