When you pick up a prescription, you expect the medicine to work. But what if the pill you get today looks nothing like the one you took yesterday? For millions of people, this isn’t just a minor surprise-it’s a safety risk. The problem isn’t the drug itself. It’s how we explain it.
Why Generic Medications Confuse Patients
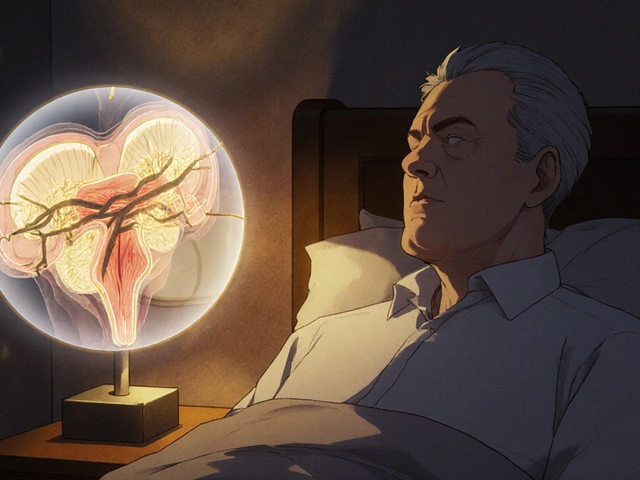
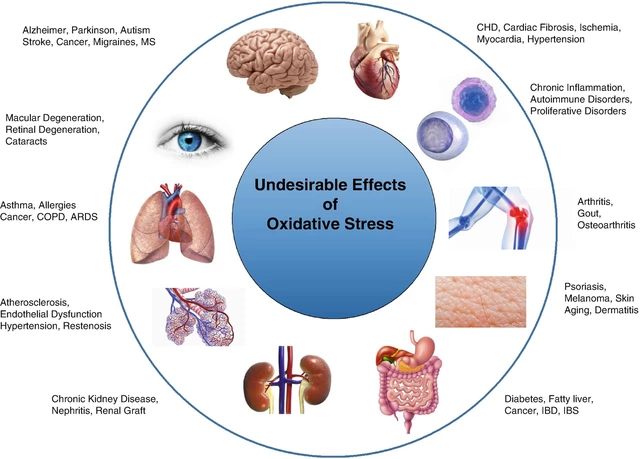
Generic drugs are chemically identical to their brand-name cousins. They contain the same active ingredient, work the same way, and are held to the same safety standards. But they look different. A white oval pill today might be a pink round one tomorrow. The name on the bottle changes. The packaging shifts. And for patients with low health literacy, this isn’t just confusing-it’s terrifying.One in three American adults struggles to understand basic health information. That’s 80 million people. When someone with limited reading skills sees a new-looking pill, they often assume it’s a different medicine. Some stop taking it. Others double up, thinking they missed a dose. One man with type 2 diabetes didn’t take his metformin for three days after his generic changed shape. He ended up in the ER with dangerously high blood sugar.
This isn’t rare. A 2021 study found that over half of older adults taking heart medications threw away pills they didn’t recognize. That’s called “pill dumping.” And it’s happening because the system doesn’t account for how people actually experience medicine-not as scientific terms, but as shapes, colors, and labels they can’t always read.
The Brand-Name Advantage (and Why Generics Get Blamed)
Brand-name drugs have an edge: recognition. Years of TV ads, logos, and consistent packaging make them familiar. When a patient sees “Lipitor” or “Zoloft,” they know what to expect. Generics? No such luck. They’re sold under chemical names like “atorvastatin” or “sertraline.” No marketing. No brand loyalty. Just a pill that looks different every time it’s refilled.That’s why 68% of patients worry generics won’t work-even though they do. A 2018 study showed patients were three times more likely to refuse a generic if they had low health literacy. And it’s not just fear. Many patients believe the cheaper price means lower quality. That’s not science. It’s perception. And perception drives behavior.
Doctors and pharmacists often assume patients understand the difference. But research shows 42% of patients can’t correctly identify that generics are therapeutically equal. If you’re not trained to ask, you won’t know they’re confused. And if they’re too embarrassed to say they don’t understand, the gap stays hidden.
What Happens When Patients Don’t Understand
The consequences are real-and dangerous.- Medication errors linked to generic confusion caused over 1,200 reported incidents between 2015 and 2020.
- Patients with low health literacy are 2.5 times more likely to take the wrong dose.
- Medicare beneficiaries with basic literacy skills are 3.1 times more likely to refuse generic substitution.
- Emergency room visits tied to medication mistakes cost the U.S. system over $2 billion annually.
These aren’t statistics. They’re people. A grandmother who stops her blood pressure pill because it’s now blue instead of white. A veteran who skips his diabetes meds because the label says “metformin” instead of “Glucophage.” A single parent who doesn’t know how to explain the new pill to their child’s caregiver.
The system isn’t broken because people are careless. It’s broken because it was designed for people who already understand how medicine works. But most people don’t.
What’s Being Done to Fix It
Change is happening-but slowly. Here’s what’s working:The “Ask Me 3” Program trains doctors and pharmacists to ask three simple questions: What is my main problem? What do I need to do? Why is it important? When this was used in over 1,200 clinics, medication errors linked to generics dropped by 31%.
Brown Bag Reviews let patients bring all their pills to appointments. Pharmacists lay them out and check for mismatches. In one Johns Hopkins study, this cut medication errors by 44%. It’s simple. It’s cheap. And it works.
Standardized Packaging is gaining ground. Australia started color-coding generics by therapeutic class-like blue for blood pressure, green for diabetes. Errors dropped by 33%. The FDA is now drafting similar guidelines. The European Union already requires consistent appearance for generics in 27 countries. Mistakes fell by 27%.
Digital Tools are helping too. Apps like Medisafe let users take a photo of their pill. The app matches it to a database and says: “This is metformin 500mg. Same as before. Just a different maker.” In a clinical trial, this boosted understanding by 37%. And new AI tools that recognize pills by image are now showing 63% improvement in low-literacy users.
Even the government is stepping up. The FDA spent $4.7 million in 2023 on plain-language labeling for generics. The CDC’s Universal Precautions approach is now used in over 90% of community health centers. And in 38 states, pharmacists are now legally required to assess a patient’s understanding before switching to a generic.
What You Can Do Right Now
You don’t need to wait for policy changes to protect yourself or a loved one. Here’s how to take control:- Always ask: “Is this the same medicine as before?” If the pill looks different, it’s not a mistake-it’s normal. But you have a right to know why.
- Use the Brown Bag method: Bring all your meds-pills, patches, inhalers-to every appointment. Even if you think you know them all.
- Take a photo: Snap a picture of each pill when you get it. Save it in your phone. Next time, compare.
- Use free apps: Medisafe, MyTherapy, and Pill Identifier by WebMD let you search by shape, color, or imprint. They’re free. They’re accurate.
- Speak up: If you’re confused, say so. No one will judge you. Pharmacists are trained to help. But they can’t help if you don’t tell them.
And if you’re a caregiver, family member, or friend: don’t assume they understand. Ask. Show them the pill. Help them take the photo. Be their bridge to the system.
The Bigger Picture
This isn’t just about pills. It’s about dignity. It’s about trust. It’s about whether a person can safely manage their own health in a system that’s not built for them.Health literacy isn’t about how smart someone is. It’s about how well the system speaks to them. And right now, the system is speaking in jargon, changing colors, and expecting people to remember chemical names.
The good news? We know what works. We have the tools. We have the data. What’s missing is the will to make it standard-not optional-for everyone.
Next time you see a different-looking pill, don’t panic. Don’t guess. Ask. Take a picture. Call your pharmacist. You’re not being difficult. You’re being smart.
And if you’re on the other side-the doctor, the pharmacist, the nurse-remember: your job isn’t just to dispense medicine. It’s to make sure it’s understood.
Are generic medications really the same as brand-name drugs?
Yes. Generic medications contain the same active ingredient, dose, strength, and route of administration as their brand-name version. They are required by the FDA to work the same way in the body and meet the same quality and safety standards. The only differences are in inactive ingredients (like dyes or fillers), shape, color, and packaging-none of which affect how the drug works.
Why do generic pills look different every time I refill them?
Different manufacturers make the same generic drug, and each can choose its own pill shape, color, and imprint. There’s no national standard for how generics must look. So if your pharmacy switches suppliers, your pill might change appearance-even though it’s the same medicine. This is normal, but it’s also a major cause of confusion.
What should I do if my generic medication looks different?
Don’t stop taking it. Don’t assume it’s wrong. Call your pharmacist and ask: “Is this the same medicine as before?” They can confirm it’s the same generic drug, just from a different maker. You can also use a pill identifier app or take a photo for comparison. If you’re still unsure, ask your doctor to write “Dispense as Written” on the prescription to prevent substitutions.
Can low health literacy lead to dangerous medication mistakes?
Yes. Studies show people with low health literacy are 2.5 times more likely to take the wrong dose or skip medication because they don’t understand the label or recognize a changed pill. This leads to hospitalizations, ER visits, and worsening health conditions. It’s not about being careless-it’s about the system not being designed for how people actually understand information.
Are there tools or apps that can help me identify my generic medications?
Yes. Apps like Medisafe, MyTherapy, and WebMD’s Pill Identifier let you take a photo of your pill or enter its shape, color, and imprint. They match it to a database and tell you the name, use, and dosage. Many of these apps also track changes and alert you if your pill looks different. They’re free, easy to use, and proven to improve understanding.
What is the “Brown Bag” method and how can it help?
The Brown Bag method means bringing all your medications-prescription, over-the-counter, vitamins, supplements-to your doctor or pharmacist appointment. They lay them out and check for duplicates, interactions, or changes you may not have noticed. This simple step reduces medication errors by 44% and helps catch confusion over generic switches before they cause harm.
What Comes Next
The future of generic medication safety lies in standardization, technology, and human-centered design. Australia’s color-coding system, the EU’s packaging rules, and AI-powered recognition tools are all steps in the right direction. But real progress won’t come from new laws alone. It will come when every pharmacist asks, “Do you know what this is?” and every patient feels safe saying, “No, I don’t.”Understanding your medicine isn’t a skill you’re born with. It’s something we all need to be taught-and the system needs to be built to support that.





Alex Flores Gomez
January 30, 2026 AT 14:16Wow, finally someone gets it. Most of these ‘generic’ pills are just corporate bait-and-switch with different dyes and shapes to make you feel like you’re getting the cheap version. Newsflash: they’re chemically identical, but the system wants you to think otherwise so you’ll pay more for the brand. Pathetic.
Frank Declemij
January 30, 2026 AT 19:23The data here is solid. Medication errors from generic confusion are underreported and vastly underestimated. Standardized pill appearance isn't a luxury-it's a public health imperative. The FDA should mandate color and shape coding by therapeutic class, period.
Pawan Kumar
January 31, 2026 AT 19:31This is all orchestrated. Big Pharma and the FDA are in cahoots to keep you confused. Why do you think the pills change color? So you'll keep buying brand names. They know you're too dumb to read the label, so they make you doubt yourself. The real danger isn't the pill-it's the system that profits from your ignorance.
kabir das
February 2, 2026 AT 15:21Oh my god, I just realized-I’ve been throwing away my meds for YEARS because they looked different!!! I thought I was being smart, but I was just scared and confused… I’m crying right now. My blood pressure is probably through the roof. Why didn’t anyone tell me this before?!?!?!?!?!?!
Keith Oliver
February 4, 2026 AT 05:54Bro, if you can't tell the difference between a white oval and a pink round pill, maybe you shouldn't be managing your own meds. Just let your kid or your wife handle it. This isn't rocket science. You don't need an app to know what your heart pill looks like.
Kacey Yates
February 4, 2026 AT 22:46I'm a nurse and I see this every damn day. People stop their meds because the pill changed color. They don't ask. They don't call. They just quit. And then they show up in the ER with a crisis. We need mandatory visual education at the pharmacy counter. No more just handing out bottles like it's a vending machine.
ryan Sifontes
February 6, 2026 AT 15:15Yeah sure. More apps. More photos. More ‘brown bags.’ Meanwhile, my pharmacy still won’t tell me why my pill changed. And the guy behind the counter just shrugs and says ‘it’s the same thing.’ Like that’s enough. Whatever. I’m just gonna stop taking it.
Laura Arnal
February 7, 2026 AT 15:10This made me so emotional 😭 I used to be terrified of my meds changing colors too-until my pharmacist sat down with me and showed me the pill ID app. Now I take a pic every time. I feel so much safer. You’re not alone. And yes, you’re being smart by asking questions 💪❤️
Jasneet Minhas
February 8, 2026 AT 03:04How quaint. In India, we don’t have ‘generic’ confusion-we have no access to any pills at all. But yes, let’s spend millions on color-coding when people are dying because insulin costs more than their rent. #FirstWorldProblems
Eli In
February 8, 2026 AT 13:12I’m from a rural town where half the folks can’t read English. My grandma uses the pill app, and I take her to brown bag reviews. It’s not perfect, but it’s human. We need more of this-simple, kind, patient care. Not more jargon. More hugs.
Megan Brooks
February 9, 2026 AT 16:12The underlying issue here is not merely informational-it is epistemological. The medical establishment assumes that visibility equates to comprehension, and that physical consistency implies cognitive clarity. But the human experience of medication is phenomenological: it is rooted in memory, identity, and trust. Until we design systems that honor that, we will continue to fail those who need us most.
Ryan Pagan
February 10, 2026 AT 06:34Let’s be real-this whole generic pill chaos is a goddamn circus. You’ve got pharmacists handing out mystery capsules like they’re lottery tickets, and patients are left guessing if they’re getting the real deal or some chem-lab reject. But here’s the kicker: the tools to fix this already exist. Apps, color codes, brown bags, plain-language labels. We’re not lacking solutions. We’re lacking the guts to make them mandatory. Stop treating patients like lab rats and start treating them like humans who deserve to know what’s in their body. That’s not hard. It’s just inconvenient for the system.