Getting the quantity and directions right on a controlled substance prescription isn’t just good practice-it’s the law. One wrong number, one unclear sig, and you could be looking at license suspension, massive fines, or even criminal charges. The DEA recorded over 6,200 enforcement actions between 2018 and 2023 because of verification failures. Most of those weren’t fraud cases-they were simple mistakes that slipped through because someone skipped a step.
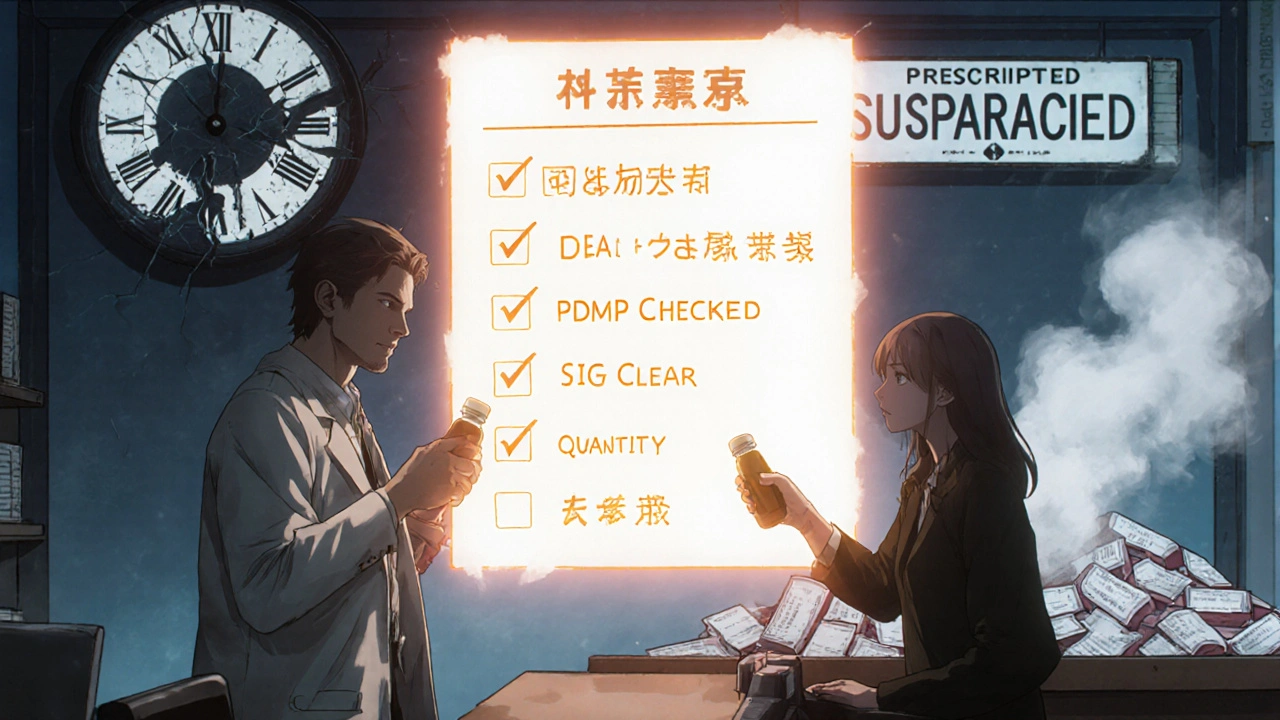
What You Must Check Every Time
Every controlled substance prescription, whether it’s oxycodone, Adderall, or gabapentin under Schedule IV, must pass seven legal checks before you dispense it. Missing even one puts you at risk. These aren’t suggestions-they’re federal requirements under 21 CFR § 1306.05.- Prescriber’s full name and address: No abbreviations. If it says "Dr. J. Smith, 123 Main St," but the DEA registration is under "Johnathan Smith," that’s a red flag.
- Date of issuance: Schedule II prescriptions must be dated the same day they’re presented. For Schedules III-V, the prescription can’t be older than six months.
- Patient’s full name and address: Middle initials matter. "J. Smith" isn’t the same as "James Smith" if the DEA registration lists the full name.
- Drug name and strength: "Hydrocodone 5mg" isn’t the same as "Hydrocodone 10mg." Watch for look-alike names like hydromorphone vs. hydrocodone.
- Dosage form: Is it a tablet, capsule, liquid, or patch? A transdermal fentanyl patch prescribed as "100 mcg/hr" isn’t interchangeable with a 50 mcg/hr patch.
- Quantity prescribed: This is where most errors happen. The number must match the written word. "30 tablets" must be written as "thirty (30) tablets." If it’s just "30," that’s incomplete and invalid under CMS rules.
- Directions for use (sig): "Take one by mouth every 6 hours as needed for pain" is clear. "1 q6h PRN pain" is acceptable if it’s standard shorthand. But "take 2 every day" without specifying if it’s for pain, cough, or something else? That’s ambiguous and must be clarified.
Verifying the DEA Number: The Math You Can’t Skip
A DEA number isn’t just a random string. It’s a checksum code designed to catch fake or mistyped numbers. The DEA’s official validation method is simple but easy to mess up if you rush.Here’s how it works:
- Take the DEA number: AB1234567
- Check the second letter: It must match the prescriber’s last name initial. If the prescriber is Dr. Smith, the second letter must be S. If it’s B, stop. Call the prescriber.
- Add the 1st, 3rd, and 5th digits: 1 + 3 + 5 = 9
- Add the 2nd, 4th, and 6th digits, then multiply by 2: (2 + 4 + 6) × 2 = 12 × 2 = 24
- Add those two results: 9 + 24 = 33
- The last digit of that sum (3) must match the 7th digit of the DEA number. In this case, the 7th digit is 5. 3 ≠ 5. Invalid.
The DEA says this method catches 98.7% of fake DEA numbers. That’s not luck-it’s math. If you’re not doing this every time, you’re leaving the door open for fraud.
Quantity and Sig: Where Most Mistakes Happen
A 2022 CMS report found that 2% of all Medicaid prescription rejections were due to mismatched quantities. That’s not a tiny number-it’s hundreds of thousands of prescriptions per year. And it’s not just about numbers.Look at this example: A prescription says "Hydrocodone 10mg, take 1 tablet every 4 hours for pain, 60 tablets." That sounds fine-until you check the patient’s PDMP history. They filled a 60-tablet script for the same drug just 10 days ago. That’s a red flag.
Or this one: "Methadone 10mg, take 1 tablet twice daily." Sounds harmless. But if the patient is on 60mg/day of oxycodone, CDC conversion factors say that’s equivalent to 24mg of methadone daily. A 10mg twice-daily dose (20mg total) is underdosed. That’s not just a mistake-it’s a safety risk.
That’s why you need to cross-reference with the CDC’s opioid conversion table:
- Codeine: 0.15
- Fentanyl transdermal: 2.4 mcg/hr
- Hydrocodone: 1
- Hydromorphone: 4
- Methadone: 4 (for 0-20mg/day), 8 (21-40mg), 10 (41-60mg), 12 (61-80mg+)
Use these to calculate total daily opioid equivalents. If the new prescription pushes the patient over 90 MME (morphine milligram equivalents) without clear clinical justification, you’re legally required to question it.
PDMP Checks: Not Optional, But Not Perfect
Forty-nine states require pharmacists to check the Prescription Drug Monitoring Program (PDMP) before dispensing controlled substances. But here’s the catch: not all PDMPs are created equal.Only 27 states require real-time updates (under 5 minutes). In 18 states, data can be up to 24 hours old. Four states update only once a week. That means a patient could get a script in California, fill it in Tennessee, and the PDMP still shows no recent activity-because the data hasn’t synced yet.
That’s why you can’t rely on PDMP alone. Use it as one piece of the puzzle. Combine it with:
- DEA number validation
- Quantity and sig review
- Prescriber contact if something doesn’t add up
Pharmacists using the NABP’s PMP InterConnect platform report a 37% reduction in verification time. But even with the best tech, you still need to think critically. If a patient is getting multiple high-dose opioids from different prescribers, that’s not a system error-it’s a warning sign.
Handwritten Prescriptions: The Wild West
Sixty-eight percent of pharmacists say illegible handwriting is their biggest headache. A scribbled "5" that looks like a "9". A "q4h" that might be "q6h". A "mg" that’s smudged into "mcg".You cannot guess. You cannot assume. You must call the prescriber. Every time.
Reddit’s r/Pharmacy_Tech is full of stories like this: one tech spent 20 minutes on a methadone script because the prescriber wrote "10" but the patient’s history showed they were on 40mg/day. The prescriber had meant 10mL, not 10mg. The script was invalid. The patient was at risk of withdrawal.
There’s no shortcut. If you can’t read it, call. Even if it’s 5:58 PM and you’re closing in two minutes. That’s your job.
Security Features You Must Spot
Since 2008, all controlled substance prescriptions must have tamper-resistant features. If you’re dispensing a paper script, check for:- Microprinting: Under 10x magnification, you should see tiny text like "DEA" or "RX" that disappears if photocopied.
- "Rx is void if more than ___ prescriptions" statement: Usually near the bottom. If it’s missing, the script is invalid.
- Quantity check-off boxes in 25-unit increments: Helps prevent tampering by limiting how much can be written in.
- Asterisk-bordered fields for quantity and refill count: These are designed to be altered only with special ink.
If any of these are missing, the prescription is not compliant. Don’t dispense it. Document why you refused. Protect yourself.
What Happens If You Skip Steps?
In 2022, DEA inspections found 38% of pharmacies had verification deficiencies. Independent pharmacies? 52% failed. Chain pharmacies? 29%. That’s not a coincidence. Chains use automated systems. Independents often rely on memory.The penalties are steep:
- Civil fines: Up to $758,574 per violation (adjusted for inflation in 2023)
- License suspension or revocation
- Criminal charges for aiding diversion
And it’s not just you. Your pharmacy’s DEA registration can be suspended. Your entire practice can be shut down.
What’s Changing in 2025 and Beyond
The DEA announced in May 2024 that all controlled substance prescriptions must include a QR code by 2026. This links to a digital record with the full prescription data, tamper history, and DSCSA product identifier.That means:
- Scanning the QR code will show you the original e-prescription, prescriber details, and whether it’s been altered.
- Verification will shift from manual math to digital validation.
- AI systems will flag patterns-like multiple high-dose scripts from the same prescriber to the same patient.
But here’s the truth: technology doesn’t replace judgment. It just gives you better data. You still need to ask: Does this make clinical sense? Is this patient at risk? Is this prescriber acting appropriately?
Final Checklist: Before You Hand Over the Meds
Use this before you count out the pills:- Is the prescriber’s DEA number valid? (Run the math)
- Is the date current and within limits?
- Does the patient’s name and address match the DEA registration?
- Is the drug name, strength, and form correct?
- Do the numerical and written quantities match?
- Are the directions clear and clinically appropriate?
- Did you check the PDMP? (Even if your state doesn’t require it, do it anyway.)
- Is the prescription printed on tamper-resistant paper?
- Did you call the prescriber if anything was unclear?
If you can answer yes to all nine, you’ve done your job. Not just legally-but ethically.
What happens if I dispense a controlled substance without verifying the quantity?
Dispensing without verifying quantity violates 21 CFR § 1306.05 and can trigger DEA enforcement. You could face civil penalties up to $758,574 per violation, license suspension, or criminal charges if the error contributed to diversion or harm. CMS data shows 2% of Medicaid rejections are due to quantity mismatches-these aren’t rare errors, they’re preventable.
Can I accept a faxed controlled substance prescription?
Yes, but only under specific conditions. Schedule II prescriptions can be faxed if they’re later followed by the original signed paper copy within 7 days. For Schedules III-V, a faxed prescription is valid as long as it meets all other DEA requirements (valid DEA number, correct quantity, etc.). However, if the fax is illegible, you must call the prescriber. Never dispense based on a poor-quality fax.
Do I need to check the PDMP in every state?
You’re legally required to check the PDMP only in states that mandate it-but 49 states do. Even in the one state without a mandate (Missouri), best practice is to check if the patient is from a state with a PDMP. Many systems like PMP InterConnect allow cross-state queries. Skipping this step leaves you vulnerable to liability if the patient has a history of misuse.
What if the prescriber’s DEA number doesn’t match their name?
Stop. Do not dispense. The second letter of the DEA number must match the prescriber’s last name initial. If it doesn’t, the number is invalid. This is a common sign of a forged or stolen DEA number. Contact the DEA’s Diversion Control Division at 1-800-882-9539 to report it. Never assume it’s a typo.
Is it okay to fill a prescription if the quantity is handwritten but the sig is printed?
No. The entire prescription must be consistent in format. If the quantity is handwritten and the rest is printed, that’s a red flag for tampering. The DEA requires the full prescription to be either handwritten or electronically generated. A hybrid format is not compliant. Call the prescriber for clarification or request a new, fully compliant prescription.
How do I verify methadone doses when the patient is switching from another opioid?
Use the CDC’s methadone conversion factors. For patients on 61-80mg of morphine equivalents daily, use a 12:1 ratio. For example, if a patient is on 72mg of oxycodone daily (72 × 1 = 72 MME), the equivalent methadone dose is 72 ÷ 12 = 6mg/day. Never assume a 1:1 conversion. Overdosing on methadone is a leading cause of accidental opioid death.
Can I use an electronic verification system instead of manual checks?
Yes-but only if the system is DSCSA-compliant and integrates with your pharmacy software. Systems with 99.2% accuracy are reliable, but they’re not foolproof. Always review alerts manually. If the system flags a discrepancy, investigate it. Never rely on automation to replace professional judgment. The FDA requires all systems to validate product identifiers with 99.9% accuracy as of September 2023.


Travis Freeman
November 29, 2025 AT 03:00Love this breakdown-seriously, every pharmacist should print this out and tape it to their counter. I’ve seen too many near-misses because someone rushed through the sig. Taking that extra 30 seconds could save a life.
Chris Taylor
November 29, 2025 AT 23:32Man, I remember one time a guy came in with a scribble that looked like '5mg' but the PDMP showed he was on 40mg daily. Called the doc-turns out he meant 5mL of liquid. We almost gave him a lethal dose. Never guess. Always call.
Melissa Michaels
November 30, 2025 AT 05:31The checklist at the end is essential. Every pharmacist should have it as a quick-reference sheet. Verification is not optional. It is a professional obligation grounded in federal regulation and ethical responsibility. Failure to comply endangers patients and exposes the practitioner to severe legal consequences. Always verify. Always document. Always act with integrity.
Nathan Brown
November 30, 2025 AT 07:50Technology will help, sure. QR codes, AI flags, automated checks. But here’s the thing: no algorithm can feel the weight of a patient’s silence when they’re in withdrawal. No system can hear the hesitation in a prescriber’s voice when they say, 'I know it looks weird, but she’s been stable for months.' We’re not just verifying scripts-we’re guarding lives. And that’s why we still have to think. Even when the machine says it’s fine.
Matthew Stanford
December 1, 2025 AT 03:11Good call on the handwritten vs printed hybrid. I’ve seen that trick before. Always a red flag. If it’s not fully digital or fully handwritten, don’t fill it. Call the prescriber. Simple. Clean. Safe.
Olivia Currie
December 2, 2025 AT 21:55OMG THIS IS SO IMPORTANT!! I just cried reading the part about the methadone conversion-like, imagine giving someone 10mg thinking it’s safe when they’re on 72mg of oxycodone?? That’s not a mistake, that’s a tragedy waiting to happen. Please, please, please, pharmacists-use the CDC table. Your hands are the last line of defense. Don’t let anyone down.
Curtis Ryan
December 3, 2025 AT 18:18Just got back from a 12-hour shift and this hit different. I called a doc at 5:45pm because the sig said 'take 1 q4h' but the patient had already filled 2 scripts in 4 days. Turns out he meant 'q6h' and the script was miswritten. Saved a potential OD. Worth the extra 10 minutes. Always call. Always.