Living with Irritable Bowel Syndrome (IBS) means dealing with unpredictable pain, bloating, and bowel changes that can turn a simple day into a challenge. It’s not just "a sensitive stomach." IBS is a real, measurable condition affecting 10-15% of people worldwide, with women making up about two-thirds of cases. Symptoms often start between ages 20 and 30, and while there’s no cure, many people find real relief with the right approach. The key is understanding your body’s signals-what triggers flare-ups, what eases them, and what treatments actually work.
What IBS Symptoms Look Like in Real Life
- Abdominal pain that comes and goes, often worse after eating and better after a bowel movement.
- Bloating that makes your belly feel tight, swollen, or distended-even if you haven’t eaten much.
- Diarrhea that hits suddenly, sometimes with urgency, or constipation that leaves you feeling incomplete after going.
- Changes in stool consistency: watery, lumpy, or alternating between the two.
- Mucus in stool, excess gas, or a feeling that you still need to go even after you’ve finished.
There are three main types, based on your dominant bowel pattern:
- IBS-D (diarrhea-predominant): About 40% of people. Bowel movements are frequent, loose, and urgent.
- IBS-C (constipation-predominant): Around 35%. Hard stools, straining, and feeling like you haven’t fully emptied.
- IBS-M (mixed): Roughly 25%. You switch between diarrhea and constipation, sometimes within the same day.
Extra-intestinal symptoms are common too. About 70% of people with IBS report things like acid reflux, nausea, early fullness after meals, or even chest pain that feels like a heart issue but isn’t. It’s all connected-your gut doesn’t work in isolation.
What Makes IBS Flare Up?
- High-FODMAP foods: These are short-chain carbs that ferment in your gut and cause gas, bloating, and pain. Common ones include onions, garlic, wheat, apples, milk, beans, and artificial sweeteners like sorbitol. About 70% of people with IBS see improvement on a low-FODMAP diet.
- Caffeine and alcohol: Both stimulate the gut and can speed things up-or make cramping worse.
- Fatty or fried foods: These slow digestion and can trigger pain or bloating, especially in IBS-C.
- Stress: Emotional pressure doesn’t cause IBS, but it makes symptoms 60-80% worse. Think deadline stress, family arguments, or even sleep loss.
- Hormonal shifts: Many women notice symptoms spike right before or during their period. Estrogen and progesterone affect gut motility.
- Antibiotics: About 1 in 4 people develop IBS after a course of antibiotics. They disrupt the balance of good bacteria in your gut.
It’s not about being "too sensitive." It’s about your gut reacting differently to things most people handle without issue. The triggers vary from person to person. That’s why keeping a food and symptom diary for 2-4 weeks is one of the most useful first steps.
How Is IBS Diagnosed?
There’s no single test for IBS. Doctors use the Rome IV criteria, which requires:
- Recurrent abdominal pain at least one day per week over the last three months.
- Pain linked to bowel movements-either improving or worsening after going.
- Changes in stool frequency or form.
Before diagnosing IBS, your doctor will rule out other conditions. That’s why they may order:
- Complete blood count (to check for anemia or infection)
- Celiac disease blood test (tissue transglutaminase IgA)
- Fecal calprotectin (to detect gut inflammation, which rules out Crohn’s or ulcerative colitis)
- Hydrogen breath test (for lactose intolerance or SIBO-small intestinal bacterial overgrowth)
- Colonoscopy (if you’re over 45 or have red flags like weight loss, rectal bleeding, or family history of colon cancer)
Red flags you should never ignore: unexplained weight loss, blood in stool, anemia, or nighttime diarrhea that wakes you up. These aren’t typical IBS signs-they need faster investigation.
Medications That Actually Help
Medications aren’t one-size-fits-all. They’re chosen based on your subtype and worst symptoms.
For IBS-D (Diarrhea)
- Loperamide (Imodium): Over-the-counter. Slows bowel movements. Works for about 60% of people, but doesn’t touch pain or bloating.
- Rifaximin (Xifaxan): A non-absorbed antibiotic. Taken for 14 days. Reduces bloating and diarrhea in 40-50% of patients. Often used for flare-ups.
- Eluxadoline (Viberzi): Prescription-only. Works on gut nerves to reduce pain and diarrhea. Helps about half of IBS-D patients. Can cause constipation or pancreatitis in rare cases.
For IBS-C (Constipation)
- Linaclotide (Linzess): Taken daily. Increases fluid in the intestines. About 30-40% of people get at least three full bowel movements per week.
- Plecanatide (Trulance): Similar to linaclotide. Often better tolerated with fewer side effects like diarrhea.
- Lubiprostone (Amitiza): A chloride channel activator. Helps soften stools. Works for 25-30% of users.
For Pain and Overall Symptoms
- Antispasmodics (hyoscine, dicyclomine): These relax gut muscles. Help with cramping in about 55% of people. Can cause dry mouth or dizziness.
- Low-dose antidepressants (amitriptyline, nortriptyline): Taken at 10-30 mg at night. Not for depression. These calm the nerves between gut and brain. About 40-50% of people report better pain control and fewer bowel issues.
It’s important to know: most meds take 2-4 weeks to show effect. Antidepressants can take up to 8 weeks. Don’t give up too soon.
Non-Medication Approaches That Work
Medications help, but they’re not the whole story. Many people find better results combining treatments.
- Low-FODMAP diet: Done under a dietitian’s guidance, this is the most studied dietary approach. The process has three phases: eliminate, reintroduce, personalize. About 70% of people find their trigger foods and reduce symptoms significantly.
- Gut-directed hypnotherapy: This isn’t stage hypnosis. It’s a structured therapy that retrains how your brain responds to gut signals. Studies show 40-60% improvement in symptoms-comparable to meds.
- Cognitive behavioral therapy (CBT): Helps manage stress and negative thought patterns linked to IBS flare-ups. Works especially well for people with anxiety or trauma history.
- Probiotics: Not all are equal. Only Bifidobacterium infantis 35624 has consistent evidence in clinical trials. It improved symptoms in 35% of users versus 25% on placebo.
One big mistake people make: going too strict on the low-FODMAP diet for too long. It’s meant to be temporary. Long-term restriction can hurt your gut microbiome. The goal is to find your personal tolerance-not eliminate everything forever.
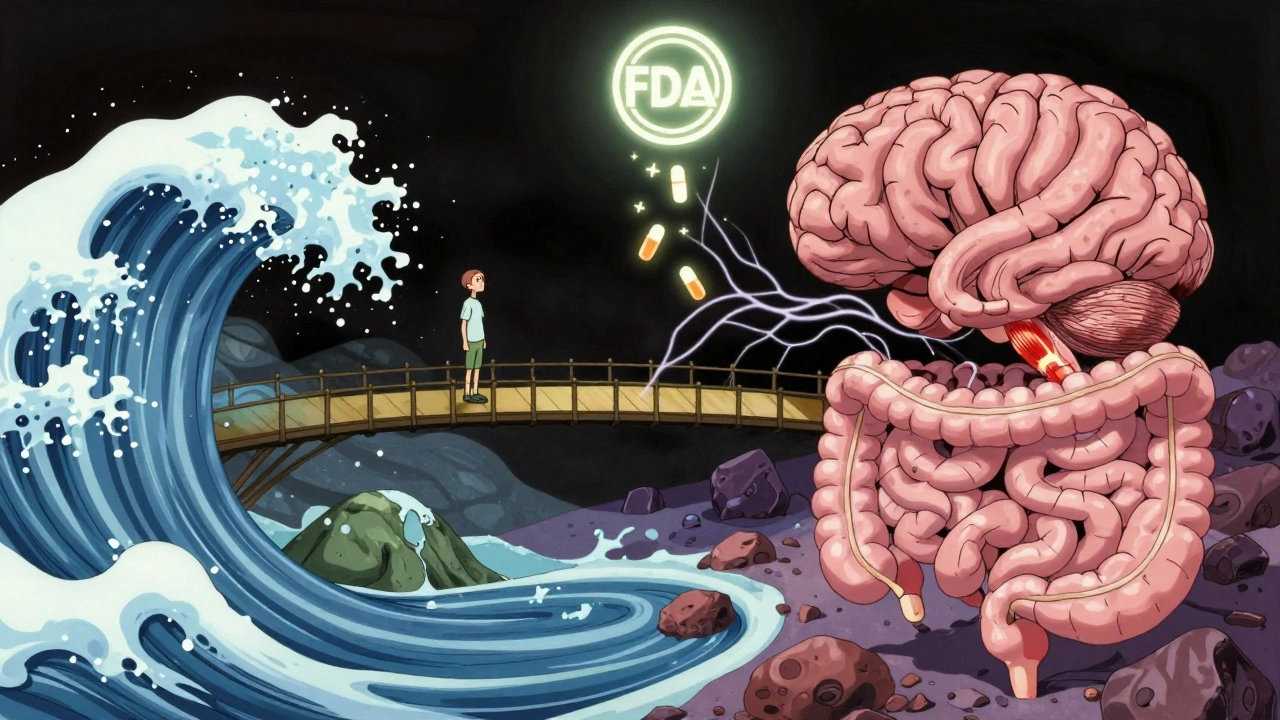
What’s New in IBS Research?
Science is moving fast. In 2023, the FDA gave breakthrough status to ibodutant, a new drug targeting gut-brain nerves. Early trials showed 45% symptom improvement versus 22% on placebo.
Fecal microbiota transplantation (FMT)-essentially a "gut transplant" from a healthy donor-is being tested in clinical trials. One 2022 study found 35% of IBS patients went into remission after FMT, compared to 15% with a placebo.
Researchers are also identifying distinct gut bacteria patterns in IBS-D versus IBS-C. This could lead to personalized probiotics or treatments based on your unique microbiome.
What to Expect Long-Term
IBS is chronic, but it’s not progressive. It doesn’t turn into Crohn’s, colitis, or cancer. Many people go years with little to no symptoms, then have a flare-up after stress, travel, or antibiotics.
A 2022 survey of over 1,200 IBS patients found:
- 68% missed work or school due to symptoms-averaging 13 days a year.
- 78% struggled to stick to dietary changes long-term.
- 62% saw major improvement with diet and lifestyle changes.
- 55% felt "much better" after 6 months of combined treatment.
Success doesn’t mean being symptom-free. It means having control. Knowing what triggers you. Having tools to manage flare-ups. Getting back to your life without fear.
Can IBS go away on its own?
IBS doesn’t usually disappear completely, but symptoms can go into remission for months or even years. Many people find that with the right diet, stress management, and sometimes medication, they can live with minimal disruption. It’s not about curing it-it’s about managing it so it doesn’t manage you.
Is IBS the same as IBD?
No. IBS (Irritable Bowel Syndrome) is a functional disorder-it affects how your gut works, but there’s no inflammation or damage. IBD (Inflammatory Bowel Disease), which includes Crohn’s disease and ulcerative colitis, involves chronic inflammation, ulcers, and structural damage. IBD can be seen on scans or biopsies; IBS cannot. The treatments are completely different.
Why do I feel bloated even when I haven’t eaten much?
In IBS, your gut is hypersensitive. Even small amounts of gas or normal digestion can trigger a strong sensation of fullness or bloating. This isn’t about how much you ate-it’s about how your nerves interpret the signals. Low-FODMAP diets and gut-directed hypnotherapy can help reduce this sensitivity over time.
Can stress cause IBS?
Stress doesn’t cause IBS, but it’s one of the strongest triggers. If you already have a sensitive gut, stress can make symptoms worse by changing how your brain and gut communicate. Managing stress with therapy, breathing exercises, or mindfulness doesn’t cure IBS-but it often reduces flare-ups by 50% or more.
Are probiotics worth trying?
Only specific strains have proven benefits. Bifidobacterium infantis 35624 is the most studied and recommended for IBS. Most other probiotics on shelves haven’t shown consistent results. Don’t waste money on generic brands-look for products that list this exact strain and have clinical backing.
How long does it take for IBS medication to work?
It varies. Loperamide works within hours. Linaclotide and rifaximin usually show results in 1-2 weeks. Antidepressants like amitriptyline can take 4-8 weeks at the right dose. Don’t stop too early. Give it time-and talk to your doctor if you’re not seeing improvement after 6-8 weeks.
Next Steps If You Suspect IBS
Start by tracking your symptoms for two weeks. Note:
- What you ate and when
- When pain or bowel changes happened
- Your stress levels that day
- Whether you slept well
Then, make an appointment with your doctor. Bring your notes. Ask about the Rome IV criteria and whether you need any tests to rule out other conditions.
If you’re diagnosed, don’t rush into medication. Start with diet and lifestyle. Find a registered dietitian who specializes in IBS and the low-FODMAP diet. Consider talking to a therapist trained in gut-directed hypnotherapy or CBT. Medication can be added later if needed.
IBS is frustrating, but you’re not alone. Thousands of people have found ways to live well with it. The path isn’t always linear-but with the right tools, relief is possible.




Declan O Reilly
December 3, 2025 AT 13:25Man, IBS is like having a rebellious roommate in your gut who throws tantrums when you eat avocado or stress about deadlines. I used to think it was all in my head until I started tracking everything-turns out, my body hates garlic more than my ex hates my music.
Low-FODMAP was a game-changer. Took me 3 weeks to adjust, but now I can eat out without planning my route to the nearest bathroom like it’s a military op.
Also, gut hypnotherapy? Sounds like witchcraft but I swear, after 8 sessions, my bloating cut in half. My therapist said my gut was basically screaming for a nap. Weird? Maybe. Effective? Absolutely.
Conor Forde
December 5, 2025 AT 08:09Let me guess-you’re one of those people who think ‘functional disorder’ means ‘it’s not real.’ Oh sweet summer child. IBS isn’t a glitch-it’s a full-on betrayal by your own nervous system.
And don’t get me started on ‘just take Imodium.’ That’s like slapping duct tape on a leaking nuclear reactor and calling it a fix.
Eluxadoline? Sounds like a villain in a Marvel movie. And yes, I’ve tried it. Side effects? My left butt cheek now has existential dread. Worth it? Depends if you enjoy being alive.
Linda Migdal
December 5, 2025 AT 12:18As an American who’s seen every fad diet under the sun, I’m skeptical-but this low-FODMAP thing actually has peer-reviewed data behind it. Unlike that keto cleanse your cousin swore by.
And let’s be real: if you’re not seeing a GI specialist who knows the Rome IV criteria, you’re wasting time. Insurance won’t cover hypnotherapy? Tough. Your gut health is worth more than your deductible.
Also, stop blaming stress. Stress doesn’t cause IBS-it exposes it. And if you’re still drinking kombucha like it’s holy water, you’re part of the problem.
Dennis Jesuyon Balogun
December 5, 2025 AT 15:18As a Nigerian who’s seen people treat IBS like a curse from ancestors, I want to say this: your body is not cursed-it’s communicating. We need to stop treating gut health like a taboo.
I’ve helped three cousins through this. First step? Stop eating fried plantain with pepper sauce at 2 a.m. Second? Find a dietitian who doesn’t think ‘African diet’ means ‘everything spicy.’
And yes-probiotics matter. But not the ones from the corner shop. Use Bifidobacterium infantis 35624. Spell it right. It’s not magic. It’s science.
Lucinda Bresnehan
December 7, 2025 AT 13:49I was diagnosed with IBS-M after 4 years of being told I was ‘just anxious.’ My doctor finally ordered the calprotectin test and said, ‘Your gut is screaming, and I’m finally listening.’
My advice? Don’t rush meds. Start with the dietitian. I did the low-FODMAP elimination phase with a notebook and cried over my lost onions. But now I eat garlic-infused oil instead-and it’s life-changing.
Also, Linaclotide? It’s expensive, but my insurance covered it after I proved I’d tried everything else. Worth every penny.
ANN JACOBS
December 9, 2025 AT 05:45It is with profound humility and a deep sense of scientific reverence that I submit the following observation: the pathophysiological underpinnings of Irritable Bowel Syndrome, as elucidated by contemporary gastroenterological research, reveal a complex, bidirectional neuro-gastrointestinal axis that is both exquisitely sensitive and profoundly modifiable through non-pharmacological interventions.
Indeed, the empirical evidence supporting gut-directed hypnotherapy as a modality for symptom attenuation is not merely statistically significant-it is phenomenologically transformative, with effect sizes rivaling those of pharmacologic agents, and without the attendant risk of iatrogenic sequelae.
Furthermore, the temporal lag in therapeutic response to low-dose tricyclic antidepressants necessitates a paradigm shift in patient expectations: one must embrace patience as a therapeutic modality in and of itself.
May we all find peace within our intestinal ecosystems.
Nnaemeka Kingsley
December 10, 2025 AT 19:24bro i had this for years and thought it was normal. then i started writing down what i ate and when i felt bad. turns out? milk and apples = disaster.
took me 2 weeks to stop eating them. now i drink oat milk and eat bananas. no more panic before meetings.
also, probiotics? just get the one with Bifidobacterium infantis. dont waste money on fancy bottles with rainbows.
Kshitij Shah
December 11, 2025 AT 06:44So let me get this straight-you’re telling me the solution to my gut chaos is… eating boring food, talking to a therapist, and paying $300 for a pill that makes me constipated?
And the FDA just greenlit a drug called ‘ibodutant’? Sounds like a rejected Marvel villain’s name.
At this point, I’d rather just move to a monastery and live on rice and silence.
Sean McCarthy
December 11, 2025 AT 13:4870% improvement on low-FODMAP? Where’s the p-value? What was the sample size? Was there a placebo control? Who funded the study? Did they correct for multiple comparisons? Did they account for dietary adherence bias? The data is statistically weak and methodologically suspect.
And antidepressants for IBS? That’s just psychiatric gaslighting dressed up as medicine. Your gut isn’t broken-it’s being misdiagnosed by a system that prefers pills over real answers.
Jaswinder Singh
December 13, 2025 AT 02:44bro you ain’t got IBS, you got anxiety. just stop stressing. i had the same thing, ate more rice, drank warm water, and now i’m fine.
why you need all these tests and pills? you just need to be strong. my uncle in Punjab, he never heard of FODMAP, still poops like a champ.
Bee Floyd
December 13, 2025 AT 07:21I’ve been living with IBS-C for 12 years. I used to think I was broken. Then I found a dietitian who didn’t judge me for eating three bananas a day.
Turns out, my body doesn’t hate fiber-it hates the wrong kind. Soluble fiber, not insoluble. Psyllium husk, not bran.
And yes, I took amitriptyline. Took 6 weeks. Now I sleep through the night without worrying if my gut’s going to revolt.
It’s not perfect. But it’s mine. And I’m learning to live with it, not fight it.
Jeremy Butler
December 14, 2025 AT 11:09The epistemological framework underpinning contemporary IBS management is predicated upon a reductionist biomedical paradigm that neglects the phenomenological lived experience of the patient. One is compelled to interrogate the ontological status of the ‘functional disorder’ designation-does it signify a lack of pathophysiology, or merely a lack of diagnostic instrumentation?
Furthermore, the commodification of gut-directed hypnotherapy as a ‘treatment modality’ raises ethical concerns regarding the medicalization of subjective experience. Is the mind’s influence on the gut a therapeutic avenue-or a capitulation to the limitations of materialist medicine?
Courtney Co
December 15, 2025 AT 05:28Wait-so you’re saying stress doesn’t cause IBS? But I cried over a dead plant last week and then spent 3 hours in a bathroom. That’s not coincidence, that’s destiny.
Also, I tried the low-FODMAP diet and I miss onions so much I started crying in the grocery store. Is that normal? Should I be on antidepressants for grief? I think I’m grieving my garlic.
Can we just make a support group for people who miss food? I need to talk to someone who understands.