Macrolides: What They Are, How They Work, and Which Ones You Might Encounter
When your doctor prescribes an antibiotic for a stubborn sinus infection, bronchitis, or a skin rash, one of the most likely names you’ll hear is macrolides, a class of antibiotics that block bacteria from making proteins they need to survive. Also known as protein synthesis inhibitors, macrolides have been around since the 1950s and still hold their ground in modern treatment plans. They don’t kill bacteria outright—they stop them from multiplying. That gives your immune system the upper hand. Unlike broad-spectrum drugs that hit everything, macrolides are often chosen when you need something targeted, especially for infections caused by atypical bacteria like mycoplasma or chlamydia.
Three names come up again and again in this group: azithromycin, a once-daily pill often used for pneumonia and ear infections, clarithromycin, commonly paired with other drugs to treat stomach ulcers caused by H. pylori, and erythromycin, the original macrolide, still used when patients can’t take penicillin. Each has its own rhythm—azithromycin lasts longer in the body, so you take fewer pills. Clarithromycin works faster in some cases. Erythromycin? It’s older, has more stomach upset, but it’s cheap and reliable. These aren’t interchangeable. Your doctor picks based on the bug, your history, and possible side effects.
Macrolides don’t just fight infections—they’re also used in long-term care for chronic lung conditions like bronchiectasis or cystic fibrosis, where reducing inflammation matters as much as killing germs. They’re not magic, though. Overuse has led to resistance, especially in strep throat and ear infections. That’s why you’ll often see them as a second choice after penicillin or amoxicillin. But when those fail, or you’re allergic, macrolides step in. You’ll also find them in combination therapies, like with proton pump inhibitors for ulcers, or with other antibiotics for tougher lung infections.
Side effects? Stomach pain and diarrhea are common. Rarely, they can mess with heart rhythm—especially if you’re already on other meds that affect your QT interval. That’s why your pharmacist asks about all your pills. And no, you shouldn’t grab azithromycin from a friend’s old prescription. Even if the symptoms look the same, the bug might not be, and you could make things worse.
What you’ll find in the posts below is a collection of real-world guides on how macrolides fit into the bigger picture of antibiotics, drug interactions, and treatment choices. You’ll see how they compare to other classes like cephalosporins and tetracyclines, what to watch for when mixing them with antidepressants or heart meds, and how they stack up against newer options. This isn’t theory—it’s what people actually deal with when prescriptions come in, side effects show up, or a doctor suggests switching. Whether you’re taking one now, were prescribed one in the past, or just want to understand why your doctor picked it, these posts give you the straight facts.
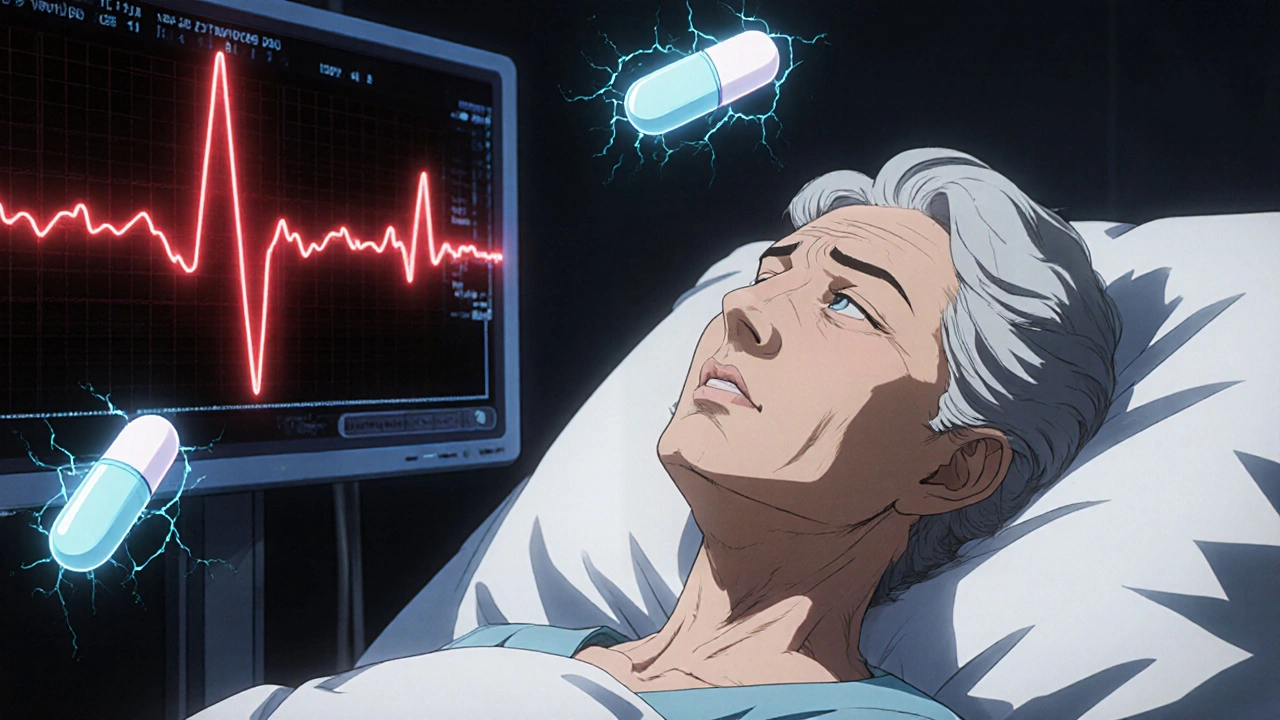
QT Prolongation with Fluoroquinolones and Macrolides: Monitoring Strategies
Fluoroquinolones and macrolides can cause dangerous QT prolongation, increasing the risk of life-threatening arrhythmias. Learn how to assess risk, choose safer antibiotics, and implement effective ECG monitoring strategies.
Detail