It’s easy to think that taking a few extra pills or mixing a supplement with your prescription is harmless. But when drugs interact, the results can turn dangerous - fast. You might feel a little dizzy after starting a new antibiotic. Or your heart starts racing after adding an over-the-counter cold medicine. At first, you brush it off: “It’s just stress,” “I didn’t sleep well,” or “This happens sometimes.” But those symptoms could be your body screaming that something’s wrong with how your medications are working together.
Drug interactions happen when one substance - whether it’s a prescription, an OTC pill, a supplement, or even grapefruit juice - changes how another drug works in your body. This can make the drug too strong, too weak, or trigger side effects you’ve never had before. The U.S. Food and Drug Administration says these interactions can make your medication less effective, cause unexpected side effects, or even increase its power dangerously. And it’s not rare: about 1.3 million emergency room visits in the U.S. each year are linked to adverse drug reactions, with over 350,000 leading to hospital stays.
Immediate Emergency Signs: Call 911 Now
If you’re taking multiple medications - especially for heart conditions, mental health, or chronic pain - you need to know the red flags that demand immediate action. These aren’t minor inconveniences. They’re life-threatening.
- Difficulty breathing or oxygen levels below 90%: If you’re gasping, wheezing, or your finger pulse oximeter reads under 90%, this could mean anaphylaxis or severe lung reaction. In 78% of serious allergic reactions, this is the first sign.
- Swelling of the face, lips, tongue, or throat: This isn’t just a rash. It’s angioedema - and it can block your airway in under 20 minutes. Once the swelling moves into your throat, you won’t be able to speak, swallow, or breathe.
- Heart rate over 120 with blood pressure below 90: This combo signals cardiovascular collapse. It’s a hallmark of anaphylactic shock and requires epinephrine and IV fluids within minutes.
- Seizures lasting more than 2 minutes: Especially if you’re on antidepressants, pain meds, or seizure drugs. A single seizure from lidocaine toxicity, for example, can lead to brain damage if untreated.
- Body temperature above 41°C (106°F) with rigid muscles and extreme agitation: This is serotonin syndrome - a dangerous buildup of serotonin from mixing SSRIs, opioids, migraine meds, or even St. John’s wort. Without quick treatment, it can cause organ failure.
- High fever over 40°C (104°F), dark urine, and extreme stiffness: These are signs of neuroleptic malignant syndrome, a rare but deadly reaction to antipsychotics. Creatine kinase levels can spike above 10,000 U/L - a clear sign of muscle breakdown.
If you or someone else shows any of these, don’t wait. Don’t call your doctor’s office. Don’t Google it. Call 911 or go to the nearest emergency room. Every minute counts.
Symptoms That Need a Doctor Within 24 Hours
Not every interaction causes a crisis - but many still need urgent attention. Waiting too long can turn a manageable issue into a serious one.
- A rash covering more than 30% of your body: Especially if it’s red, raised, and spreading. This could be DRESS syndrome - a delayed allergic reaction that can damage your liver, kidneys, or lungs. It often shows up 2-6 weeks after starting a new drug, especially anticonvulsants or antibiotics.
- Unexplained fever above 38.5°C (101.3°F) for more than 48 hours: If you’ve recently started a new antibiotic, anticonvulsant, or anti-inflammatory, this could mean serum sickness or a systemic reaction. Don’t assume it’s a cold.
- Unusual bruising, bleeding gums, or nosebleeds: A platelet count below 100,000/μL means your blood can’t clot properly. This can happen with antibiotics like vancomycin or even common painkillers like ibuprofen over time.
- Yellow skin or eyes, dark urine, or belly pain: These are signs your liver is struggling. ALT levels above 120 U/L suggest drug-induced liver injury. It’s rare - about 1 in 10,000 to 100,000 cases - but can lead to liver failure if ignored.
- Little or no urine for 6+ hours with rising creatinine: If you’re on blood pressure meds, NSAIDs, or diuretics, your kidneys might be under stress. A 0.3 mg/dL rise in creatinine over 48 hours is a red flag for acute kidney injury, which affects up to 25% of hospital patients due to medications.
These symptoms won’t always land you in the ER - but they should land you in your doctor’s office the same day. Delaying care increases the risk of permanent damage.

Who’s at Highest Risk?
It’s not just older adults - though they’re most affected. People taking five or more medications have a 57% chance of experiencing a major drug interaction, according to the Journal of the American Geriatrics Society. That’s why seniors on heart meds, blood thinners, and painkillers are especially vulnerable.
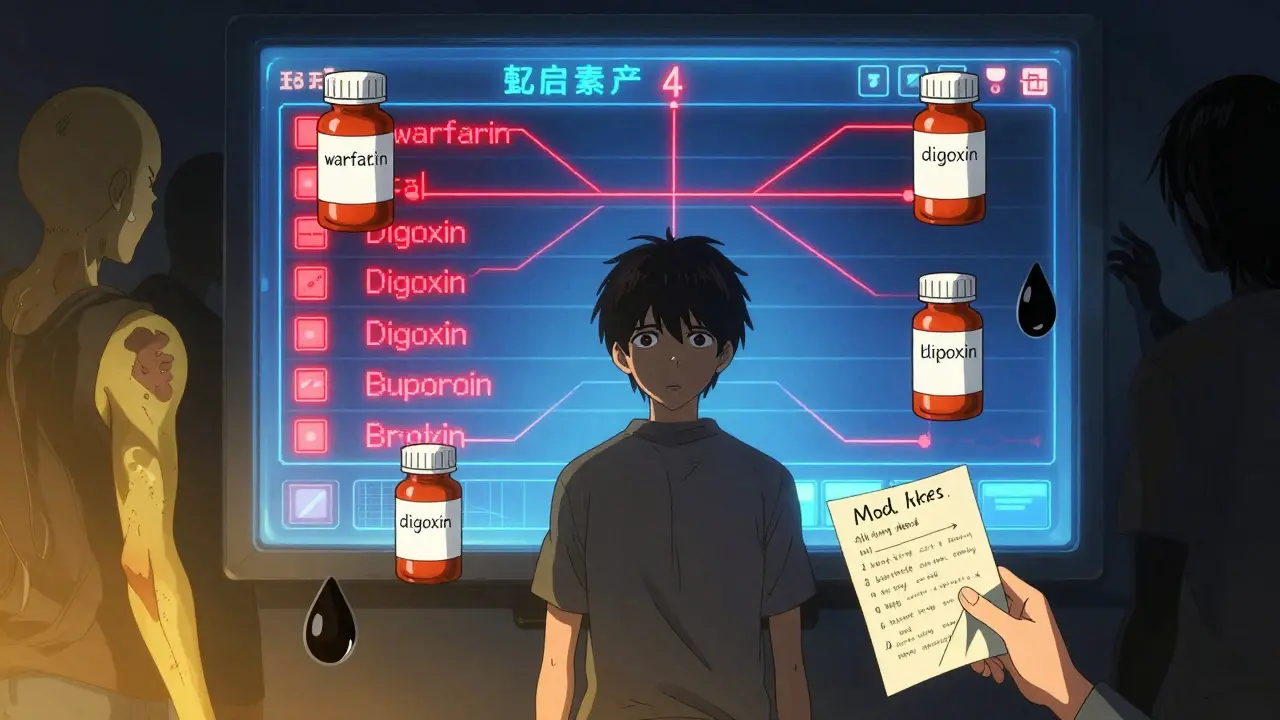
But it’s not just age. Anyone taking drugs with a narrow therapeutic index is at risk. These are medications where even a small change in blood level can cause harm:
- Warfarin (blood thinner): A single interaction with antibiotics or vitamin K supplements can cause dangerous bleeding or clots.
- Digoxin (heart medication): Grapefruit juice, antibiotics, or even magnesium supplements can spike levels to toxic ranges.
- Phenytoin (seizure drug): Even minor changes can trigger seizures or neurological damage.
And it’s not just prescriptions. Herbal supplements like St. John’s wort, garlic, or ginkgo biloba cause 18% of serious interactions, according to the National Institutes of Health. Many people don’t think of them as “drugs,” but they act like them - and they can interfere with everything from antidepressants to chemotherapy.
What You Can Do Before It Gets Worse
Prevention is your best tool. Here’s how to protect yourself:
- Keep a full list of everything you take: Include prescriptions, OTC meds, vitamins, herbs, and even recreational substances like alcohol or marijuana. Write down doses and how often you take them.
- Use a reliable drug interaction checker: Drugs.com’s tool screens over 24,000 medications and 500,000 interactions. The Liverpool Drug Interaction Group checker is especially good for HIV and transplant patients.
- Ask your pharmacist every time you pick up a new prescription: They’re trained to spot interactions. A 2022 survey found that 58% of patients waited over 12 hours to ask for help - but those who called poison control within an hour avoided ER visits 89% of the time.
- Use the STOP protocol: If you suspect an interaction, Stop taking the medication, Telephone your provider, Observe your symptoms, and Present all your medication containers at your appointment.
Many doctors rely on clinical decision support tools built into electronic health records - but a 2022 report found only 63% of these systems properly flag the severity of interactions. That means you can’t always count on your doctor to catch it. You need to be your own advocate.
Why People Wait Too Long - And Why It’s Dangerous
A 2023 study on MedHelp showed that 72% of people who had moderate drug interactions initially ignored their symptoms. They thought they were just tired, anxious, or dehydrated. One Reddit user described taking fluoxetine and then getting fentanyl for a dental procedure. Within hours, he developed clonus (involuntary muscle jerks), sweating, and confusion. He thought it was “just nerves.” By the time he went to the ER, he needed ICU care.
Another study in JAMA Internal Medicine found that 68% of patients couldn’t recognize serious interaction symptoms from the printed leaflets in their pill bottles. The language is confusing. The warnings are buried. And most people assume “side effects” mean mild nausea or drowsiness - not seizures or organ failure.
Don’t make that mistake. If you feel something is off - especially if it’s new, sudden, or getting worse - trust your gut. Medications are powerful. They’re not harmless. And interactions don’t always show up right away. Sometimes, it takes days. Sometimes, it takes weeks. But when they hit, they hit hard.
What Happens When You Get Help
If you go to the doctor or ER with suspected drug interactions, they’ll likely:
- Ask for a full medication list - including supplements and alcohol use
- Check your vital signs: heart rate, blood pressure, temperature, oxygen levels
- Order blood tests: liver enzymes, kidney function, electrolytes, drug levels
- Use the CIOMS scale to determine if the interaction is “definite” - based on timing, symptom resolution after stopping the drug, and recurrence if restarted
- Stop or adjust the offending medication(s)
- Provide supportive care: IV fluids, activated charcoal, antidotes like naloxone or cyproheptadine for serotonin syndrome
Early intervention saves lives. A 2022 report from the American Association of Poison Control Centers found that 65% of the 2.1 million exposure calls they handled were managed without hospital visits - because people called early.
What should I do if I think I’m having a drug interaction?
Stop taking the medication that you suspect caused the reaction. Call your doctor or pharmacist immediately. If you’re experiencing trouble breathing, swelling, chest pain, seizures, or a very high fever, call 911. Don’t wait to see if it gets better. Keep all your medication containers handy - including vitamins and supplements - to show your provider.
Can over-the-counter drugs cause dangerous interactions?
Yes. Common OTC painkillers like ibuprofen or naproxen can interact with blood pressure meds, increasing kidney risk. Cold medicines with decongestants like pseudoephedrine can raise blood pressure dangerously when taken with antidepressants. Even antacids can reduce absorption of antibiotics like ciprofloxacin. Always check with your pharmacist before taking anything new, even if it’s sold without a prescription.
Are herbal supplements safe to take with prescription drugs?
Not always. St. John’s wort can make birth control, antidepressants, and HIV meds ineffective. Garlic and ginkgo can increase bleeding risk when taken with warfarin. Turmeric can interfere with blood sugar control. Many people assume “natural” means “safe,” but herbs act like drugs - and can cause serious interactions. Always tell your doctor what supplements you’re using.
How can I check for drug interactions myself?
Use trusted tools like Drugs.com’s drug interaction checker or the Liverpool Drug Interaction Group tool. Enter every medication you take - including vitamins, herbs, and alcohol. These tools screen thousands of combinations and flag serious risks. But remember: no app replaces professional advice. Always confirm with your pharmacist or doctor.
Why do doctors sometimes miss drug interactions?
Many electronic health systems flood doctors with alerts - sometimes dozens per patient. This leads to “alert fatigue,” where doctors start ignoring warnings. A 2022 study found that nearly half of physicians override 20% or more of interaction alerts. Also, patients often forget to mention supplements, alcohol, or OTC meds. The system isn’t perfect - so you need to speak up.
What if I’m on a lot of medications? Am I doomed to have interactions?
No - but you need to be more careful. People taking five or more drugs have a 57% risk of interaction. Talk to your doctor about whether you really need all of them. Ask if any can be stopped, reduced, or replaced. A medication review every 6-12 months can cut risks significantly. Use a pill organizer and keep a written list. Your safety depends on being organized and proactive.
Drug interactions are preventable - but only if you act. Don’t wait for a crisis. Know the signs. Keep track of what you take. Ask questions. And when in doubt, get help. Your life might depend on it.





Vicky Zhang
January 14, 2026 AT 21:01Oh my god I just realized I’ve been taking melatonin with my blood pressure med for months and I’ve been getting these crazy dizzy spells. I thought it was just me being tired from work but now I’m scared. I called my pharmacist today and they said it could totally mess with the meds. I’m so glad I read this. I’m deleting all my supplements off my nightstand until I talk to my doctor. Please everyone, don’t be like me and just ignore it.
Susie Deer
January 15, 2026 AT 19:40Stop taking everything and just live. Drugs are poison. The system wants you dependent. Your body works fine if you stop listening to doctors.
Andrew Freeman
January 17, 2026 AT 15:25bro i took ibuprofen with my antidepressant once and i was fine lmao. why are we acting like every combo is gonna kill us. also grapefruit juice is fine if you dont drink 2 gallons a day
says haze
January 19, 2026 AT 02:43It’s fascinating how society has pathologized bodily autonomy under the guise of pharmaceutical safety. We’ve outsourced our physiological intuition to algorithmic alert systems and clinical decision trees, all while ignoring the epistemological violence of medical paternalism. The real interaction isn’t between drugs-it’s between the individual and the institutional apparatus that demands compliance over curiosity.
Alvin Bregman
January 20, 2026 AT 22:47i get what the post is saying but honestly i think people freak out too much. i take like 6 things and never had a problem. maybe just pay attention to how you feel and dont panic every time you get a headache
Sarah -Jane Vincent
January 22, 2026 AT 01:00EVERYONE knows the FDA is in bed with Big Pharma. They only warn you about the most obvious stuff. Did you know they suppress data on 80% of drug interactions? I’ve got screenshots. The real danger is they don’t tell you about the combo between your blood thinner and that ‘natural’ turmeric supplement they sell at Whole Foods. They want you sick so they can keep selling you more pills. Wake up.
Henry Sy
January 23, 2026 AT 03:56yo i had serotonin syndrome last year after mixing my SSRI with some energy gummies. thought i was just having a panic attack. ended up in the ER screaming about aliens controlling my nerves. they gave me cyproheptadine and i cried for an hour. now i keep a printed list of everything i take taped to my fridge. i’m alive because i didn’t ignore it. don’t be a dumbass like me.
shiv singh
January 23, 2026 AT 23:09you people are so naive. you think the system cares if you live or die? they want you weak. they want you dependent. you take one pill, then another, then another. they make you believe you need them. your body was made to heal itself. stop trusting poison. stop trusting doctors. stop trusting the government. you are being manipulated. this post is a distraction from the real truth.
TooAfraid ToSay
January 24, 2026 AT 15:33my cousin died from a drug interaction. he took omeprazole with his heart med. they said it was ‘rare’. he was 28. now i check every single thing i take against every other thing. even if it’s just a vitamin. i don’t care if it’s ‘natural’. if it’s in your body, it’s a chemical. and chemicals interact. don’t gamble with your life.
Robert Way
January 26, 2026 AT 05:05did u kno that some antacids can make antibiotics not work? i did that once and got a super infection. my bad. now i always ask my pharmacist. theyre like the real heroes. not the docs who just click next.
Sarah Triphahn
January 27, 2026 AT 08:00it’s not about fear. it’s about responsibility. if you can’t be bothered to read the label or ask a simple question, then you’re not just risking your life-you’re burdening the system. you think ER nurses want to clean up your mess because you ‘didn’t think it was a big deal’? wake up. this isn’t drama. this is negligence dressed up as casual living.
Allison Deming
January 28, 2026 AT 04:41There is a profound cultural failure in our collective inability to treat pharmacological agents with the gravity they deserve. We treat medications like candy-pop a pill, feel better, repeat. We have outsourced our bodily wisdom to corporate-sanctioned algorithms and physician time constraints. The burden of vigilance has been shifted entirely onto the patient, who is often the least qualified to interpret complex pharmacokinetic interactions. This is not merely a medical issue-it is a moral one.
Dylan Livingston
January 29, 2026 AT 14:58Oh honey, I’m so touched you’re so concerned about your ‘drug interactions’. Meanwhile, I’m over here drinking a glass of wine with my antidepressant and calling it ‘self-care’. But sure, go ahead and check your pill bottles and call your pharmacist. Maybe if you stop being so anxious, you wouldn’t need so many pills in the first place. #toxicwellness #blessed