Allergic Reaction to Insulin: Signs, Risks, and What to Do
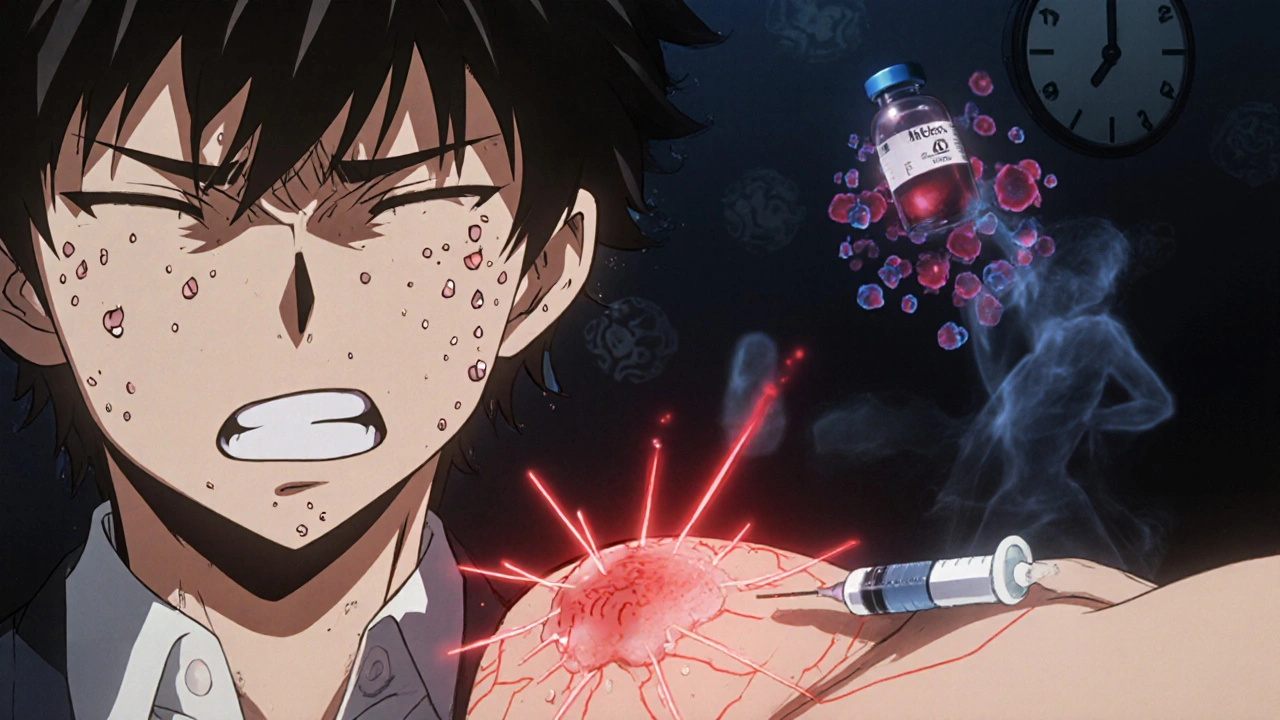
When your body treats insulin, a hormone used to control blood sugar in people with diabetes. Also known as pancreatic hormone therapy, it is essential for millions—but for some, it triggers an immune response. An allergic reaction to insulin, an immune system overreaction to insulin or its additives isn’t common, but when it happens, it can be dangerous. Symptoms range from mild itching at the injection site to life-threatening anaphylaxis, a severe, whole-body allergic response that can block airways and drop blood pressure. Most people tolerate insulin just fine, but if you’ve noticed swelling, hives, or trouble breathing after an injection, don’t ignore it.
Insulin allergies usually aren’t to the hormone itself, but to older additives like protamine or zinc, or even the preservatives in some formulations. Modern human insulin and analogs are purer, so reactions are rarer—but they still happen. Some people react to the injection device, too—like the rubber in syringes or the plastic in pens. If you’ve switched brands and suddenly broke out in hives, that’s a clue. Even if you’ve used the same insulin for years, your body can change. A reaction doesn’t mean you can’t use insulin ever again. Often, switching to a different type—like switching from beef insulin to recombinant human insulin—solves the problem. In rare cases, allergists can help with desensitization, slowly building tolerance under medical supervision.
What you shouldn’t do is stop insulin because of a rash. High blood sugar is far more dangerous than most allergic reactions. If you suspect an allergy, talk to your doctor before making any changes. They might order a skin test or blood work to confirm it’s insulin-related. You might also need to switch to a different formulation—like using insulin glargine instead of NPH—or try an insulin pump with a different delivery system. Some people find relief by using newer, more purified insulins like insulin lispro or insulin degludec, which have fewer additives. And if you’ve ever had a reaction, make sure your emergency plan includes an epinephrine auto-injector, just in case.
Below, you’ll find real-world insights from people who’ve dealt with this, along with medical guidance on testing, alternatives, and how to stay safe while managing diabetes. These aren’t theoretical tips—they’re lessons from patients and clinicians who’ve faced this exact problem.
Insulin Allergies: How to Spot and Handle Injection Reactions
Insulin allergies are rare but serious. Learn how to recognize injection reactions-local, systemic, or delayed-and what to do next, from antihistamines to desensitization, without stopping life-saving insulin therapy.
Detail