Urology: Bladder Health, Urinary Incontinence & Physical Therapy
Bladder problems can be frustrating and embarrassing, but they don’t have to rule your life. Urology covers issues from urinary tract infections to incontinence and pelvic pain. You’ll find clear, practical steps here—what works, when to get help, and how physical therapy often improves symptoms without surgery or long-term pills.
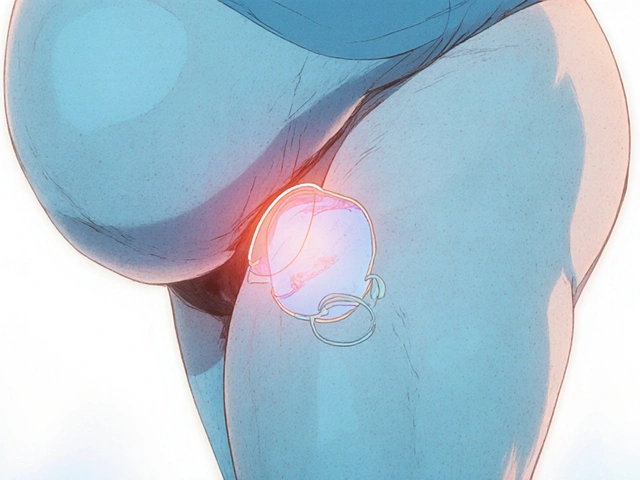
How physical therapy helps
Physical therapists who focus on pelvic health teach targeted exercises and habits that change how your bladder and pelvic muscles behave. That can mean fewer leaks, less urgency, and better control. Common PT tools include pelvic floor strengthening, biofeedback (a way to learn which muscles are working), bladder retraining, and hands-on techniques to release tight muscles.
Not every plan is the same. For example, if your pelvic floor is weak, the therapist will teach strengthening moves. If it’s too tight, therapy focuses on relaxation and stretching. Biofeedback uses simple sensors so you can see which muscles activate—this helps because many people do Kegels wrong and end up making symptoms worse.
Expect practical homework: short daily exercises, timed voiding schedules, and small lifestyle changes. Many people notice improvement in weeks, though complex cases can take a few months.
When to see a urologist and quick self-care tips
See a urologist if you have blood in your urine, severe pain, fever with urinary symptoms, sudden inability to urinate, or if simple measures don’t help after a few weeks. A urologist will take a history, check urine, do a physical exam, and may order tests like imaging or urine culture. They often work with pelvic floor physical therapists for conservative care before suggesting medications or procedures.
Quick, useful tips you can try now:
- Cut back on caffeine and alcohol; they irritate the bladder.
- Try timed voiding: plan bathroom visits every 2–3 hours and gradually stretch the interval.
- Balance fluids—don’t overdrink, but avoid dehydration.
- Practice pelvic floor exercises correctly: aim for a mix of quick squeezes and slow holds; a therapist can show the right form.
- Maintain a healthy weight and avoid heavy lifting that strains the pelvic floor.
Physical therapy is low-risk and often helps reduce symptoms enough to avoid stronger treatments. If you’re unsure where to start, ask your primary care doctor for a pelvic floor PT referral or search for a licensed pelvic health therapist. Small, consistent steps usually lead to the biggest improvements.
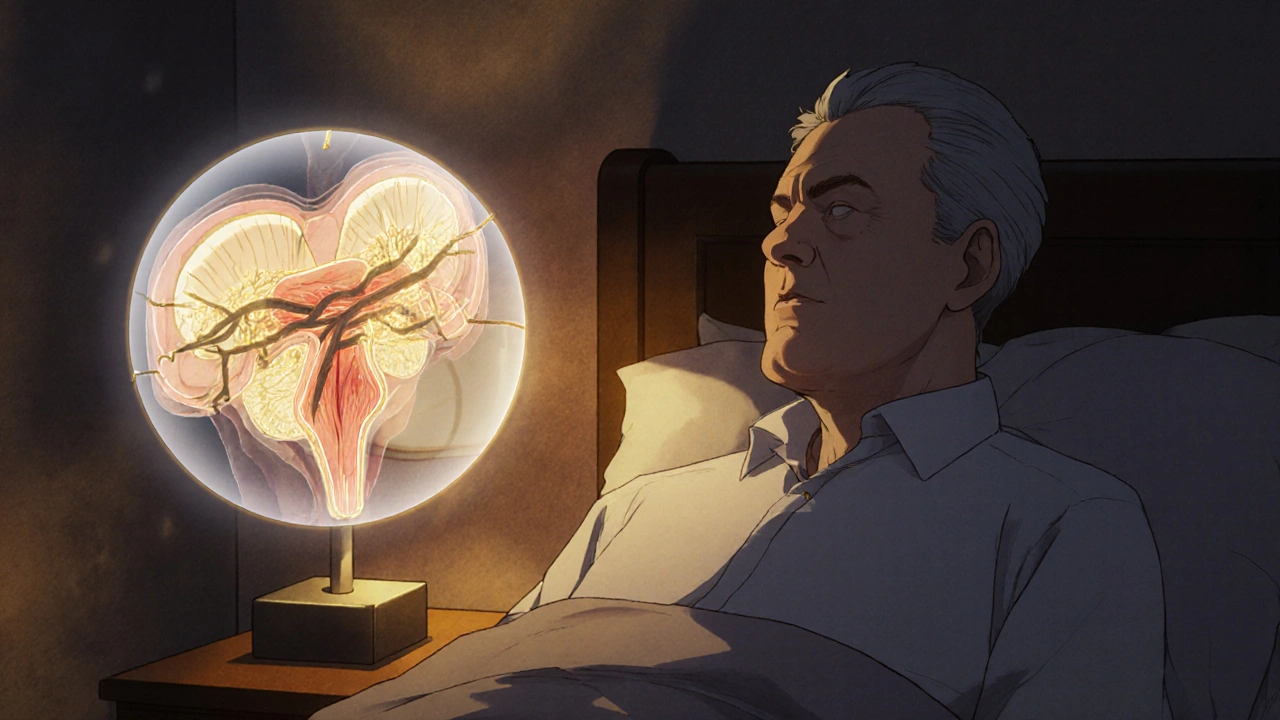
How Alfuzosin Works to Reduce Prostate Size and Improve Urinary Symptoms
Alfuzosin doesn't shrink the prostate but effectively relieves urinary symptoms by relaxing prostate muscles. Learn how it works, how it compares to other BPH treatments, and what to expect when taking it.
Detail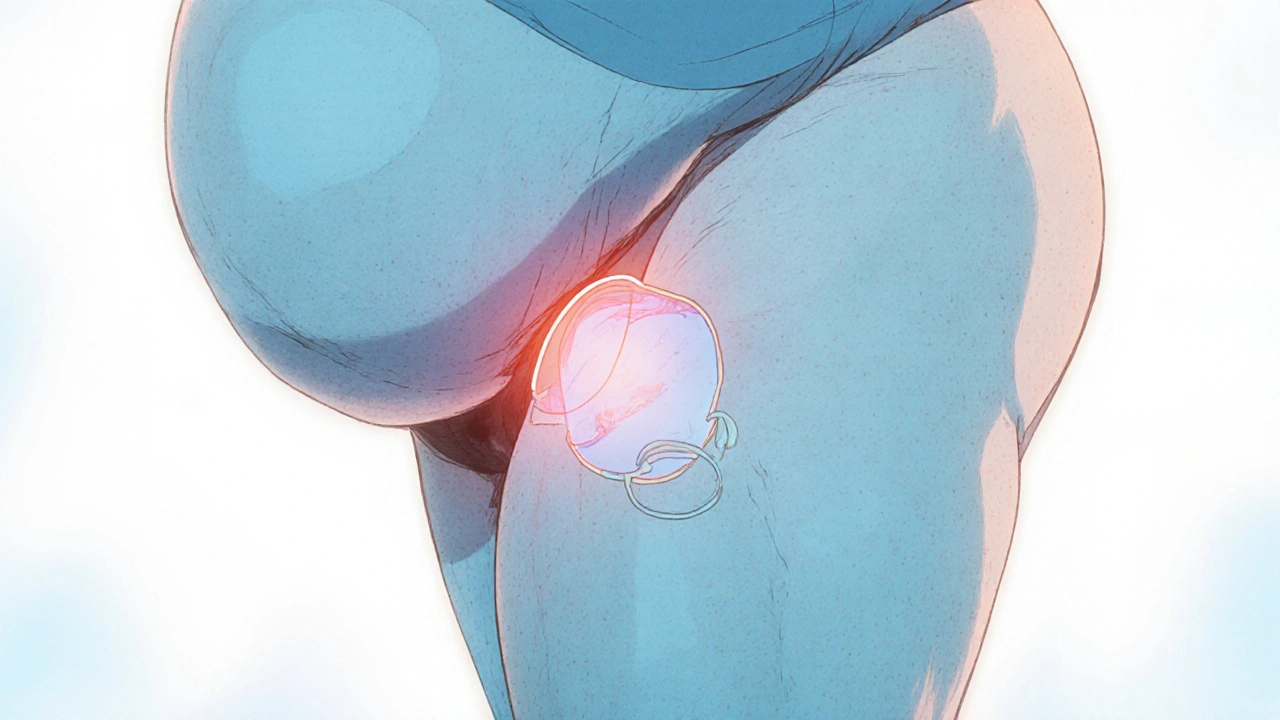
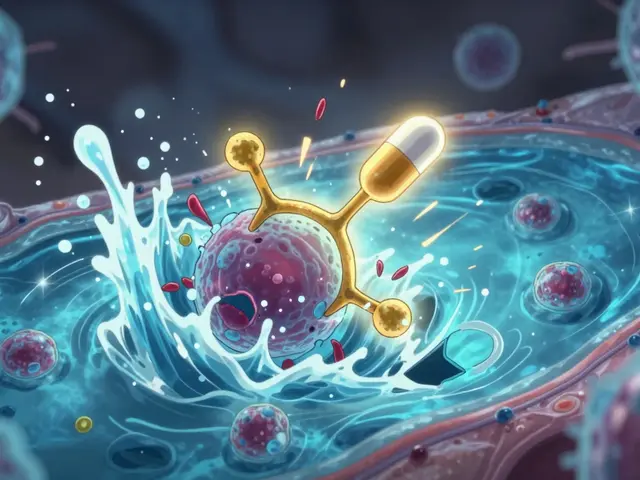
How Obesity Increases Urinary Retention Risk and What You Can Do About It
Explore how excess weight raises urinary retention risk, learn the underlying mechanisms, and discover practical lifestyle and medical strategies to manage the condition.
Detail
How Liver Failure Affects the Urinary System - Symptoms, Risks & Management
Explore how liver failure disrupts kidney function and bladder health, recognize warning signs, and learn treatment steps to protect your urinary system.
Detail
Physical Therapy's Role in Easing Bladder Issues and Urinary Incontinence
Physical therapy can be a game-changer for those dealing with bladder issues and urinary incontinence, offering non-invasive techniques to manage and improve symptoms. This approach strengthens pelvic muscles, enhances bladder control, and improves the overall quality of life. The therapy involves tailored exercises and lifestyle modifications under professional guidance. Many find relief and regain confidence through these personalized treatment plans, often reducing or even eliminating symptoms over time.
Detail