Most people think too much iron is a good thing - maybe you’ve heard that iron boosts energy or fights anemia. But when your body can’t get rid of excess iron, it starts eating away at your organs. And the liver? It’s the first to go. Hemochromatosis isn’t just a rare genetic quirk. It’s a silent killer that affects 1 in 200 people of Northern European descent. In Australia, where ancestry from Ireland and Scotland is common, it’s hiding in plain sight - in people who are tired all the time, have aching joints, or think their diabetes just came out of nowhere.
What Really Happens When You Have Too Much Iron
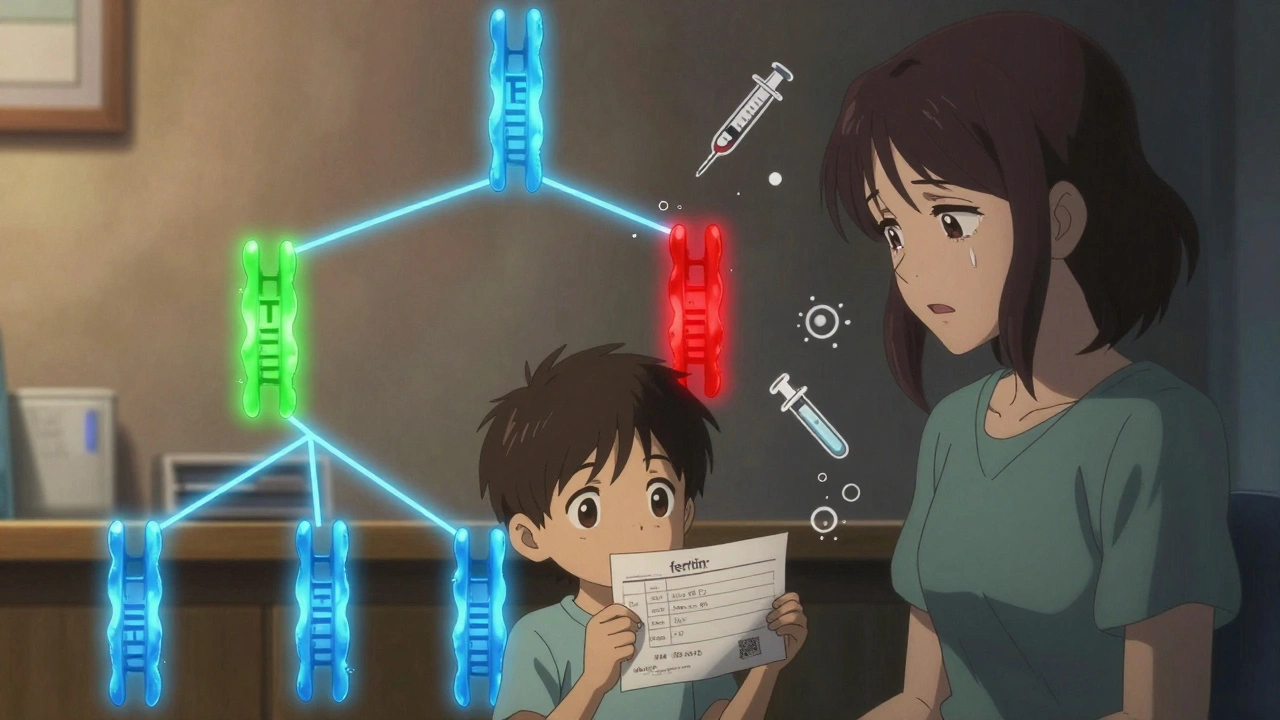
Your body doesn’t have a natural way to flush out extra iron. Unlike other minerals, you can’t sweat it out or pee it away. So when you inherit two faulty copies of the HFE gene - one from each parent - your gut keeps absorbing iron like it’s running a sale. Normally, your liver makes a hormone called hepcidin that tells your body to slow down iron intake. In hemochromatosis, that signal breaks. Iron pours in. And it doesn’t stop.
Every year, your body stores an extra 0.5 to 1 gram of iron. That sounds small, but over 10 years, you could end up with 5 grams of iron in your system. The average healthy person has less than 1 gram. That buildup doesn’t just sit there. It oxidizes. It rusts inside your liver, pancreas, heart, and joints. And that rust? It triggers inflammation, cell death, and scarring.
By the time symptoms show up - usually between ages 30 and 50 in men - you’re already halfway to organ damage. Fatigue? That’s your liver struggling. Joint pain? Iron settled in your knuckles. Skin that looks bronze or gray? That’s iron staining your skin. And if you’re a man with unexplained diabetes, you’re not just unlucky - you’re likely carrying the C282Y mutation.
Why Doctors Miss It - And How to Get Diagnosed
Most patients see 3 to 5 doctors before they get the right diagnosis. Why? Because the symptoms look like everything else: depression, aging, stress, arthritis. A 45-year-old man with low energy and stiff fingers might get antidepressants or painkillers for years. His blood tests? Maybe his ALT and AST (liver enzymes) are slightly high, so he’s told to cut back on alcohol. But if he doesn’t drink, no one connects the dots.
The fix is simple - but only if you know to ask. Two blood tests are all you need:
- Transferrin saturation - this measures how much iron is floating in your blood. If it’s above 45%, that’s a red flag.
- Serum ferritin - this tells you how much iron you’ve stored. Over 300 ng/mL in men or 200 ng/mL in women means your body is overloaded.
Once those are high, genetic testing for HFE mutations (C282Y, H63D) confirms it. No biopsy needed anymore. MRI scans can now measure liver iron accurately without poking your skin. And the cost? Genetic tests now run under $300 - down from over $1,200 just 15 years ago.
And here’s the kicker: if you’re diagnosed before ferritin hits 1,000 ng/mL, your life expectancy is normal. After that? Your risk of liver cancer and cirrhosis jumps. That’s why early detection saves lives.
Phlebotomy: The Treatment That’s Been Working Since the 1950s
There’s no magic pill. No supplement. No diet that fixes this. The only proven, effective, and free treatment is phlebotomy - removing blood. Yes, like donating blood. But instead of giving it away, you’re taking it out to save your organs.
Each 500 mL of blood removed takes out about 200-250 mg of iron. That’s the same amount your body absorbs from food in a week. So when you’re overloaded, you need to remove blood weekly - often for a year or more - until your ferritin drops to 50-100 ng/mL. That’s the sweet spot: low enough to stop damage, high enough to avoid anemia.
One patient from Melbourne, diagnosed at 48 with a ferritin of 2,850, needed 62 sessions over 15 months. He went from barely walking to hiking the Dandenongs. He didn’t feel better because of a new drug. He felt better because the rust was being pulled out of his body.
Once you’re at target levels, you switch to maintenance: every 2 to 4 months, you get a pint taken. Most people need 4 to 6 sessions a year. It’s not glamorous. It’s not trendy. But it works. And it’s covered by Medicare in Australia. Most private insurers cover it too.

What Happens If You Don’t Treat It
Untreated hemochromatosis doesn’t just make you tired. It rewires your body.
- Liver: Iron builds up, causes inflammation, then fibrosis, then cirrhosis. Once cirrhosis sets in, your risk of liver cancer rises 20-fold.
- Pancreas: Iron kills insulin-producing cells. That’s why 1 in 4 patients develop diabetes - often called "bronze diabetes" because it comes with the skin discoloration.
- Heart: Iron deposits can cause arrhythmias or heart failure. This is why some patients die suddenly, even without liver disease.
- Testes and Pituitary: Low testosterone, loss of libido, erectile dysfunction - these aren’t just "getting older." They’re signs of iron poisoning your endocrine system.
And here’s the worst part: once cirrhosis or heart damage happens, phlebotomy can’t undo it. You can stop the bleeding - but you can’t unscorch the liver. That’s why timing matters more than anything.
Why Chelation Therapy Isn’t the First Choice
You might hear about iron-chelating drugs like deferasirox or deferoxamine. They bind to iron and help your body get rid of it. Sounds perfect, right? But they’re expensive - $25,000 to $35,000 a year - and come with nasty side effects: nausea, kidney damage, hearing loss. They’re reserved for people who can’t tolerate phlebotomy: those with severe anemia, heart failure, or poor veins.
For 95% of people, phlebotomy is better. It’s safer. It’s free. And it’s proven over decades. No drug comes close.
Family Screening: The Hidden Key to Stopping Hemochromatosis
If you’re diagnosed, your siblings, kids, and parents have a 25% to 50% chance of carrying the same mutation. Yet, fewer than 30% of families get tested. That’s a missed opportunity.
One man in Adelaide found out he had hemochromatosis after his daughter’s routine blood test showed high ferritin. He got tested - and so did his wife and two sons. His youngest son, age 19, had a ferritin of 1,200. He started phlebotomy before he even had symptoms. He’ll likely live a normal life.
That’s the power of cascade screening. It doesn’t require fancy tech. Just a simple blood test and a conversation with your doctor. The Hemochromatosis Foundation says 70% of new cases are found this way.
What You Can Do Right Now
If you’re of Northern European descent - Irish, Scottish, Welsh, Scandinavian - and you’re over 30, ask your doctor for two tests: transferrin saturation and serum ferritin. Don’t wait for symptoms. Don’t wait for your liver enzymes to spike. If you’re tired, achy, or have unexplained diabetes or low libido, get tested.
If you’re already diagnosed, stick with the phlebotomy schedule. Even when you feel fine. Maintenance isn’t optional - it’s your lifeline. And if your doctor doesn’t know how to manage it, find one who does. Hepatologists, hematologists, and even some public blood banks (like the Red Cross in Australia) offer therapeutic phlebotomy.
Hemochromatosis isn’t a death sentence. It’s a treatable condition - if you catch it early. The tools are simple. The treatment is free. And the cost of ignoring it? It’s measured in liver failure, cancer, and lost years.
Don’t let your iron be your enemy. Let it be your warning sign - and act on it.






Geraldine Trainer-Cooper
December 5, 2025 AT 12:24stop ignoring fatigue. it's not stress. it's rust.
Nava Jothy
December 6, 2025 AT 21:25How many of you are still eating red meat like it's a virtue? Wake up. The gods are watching. And they are disappointed.
Kenny Pakade
December 7, 2025 AT 11:46brenda olvera
December 9, 2025 AT 01:11you don't need to be a doctor to save someone. just care enough to ask.
Myles White
December 10, 2025 AT 00:32Saketh Sai Rachapudi
December 11, 2025 AT 00:59joanne humphreys
December 11, 2025 AT 07:01Rashmi Gupta
December 12, 2025 AT 07:58