Hepatic Impairment Opioids: Guidance and Resources
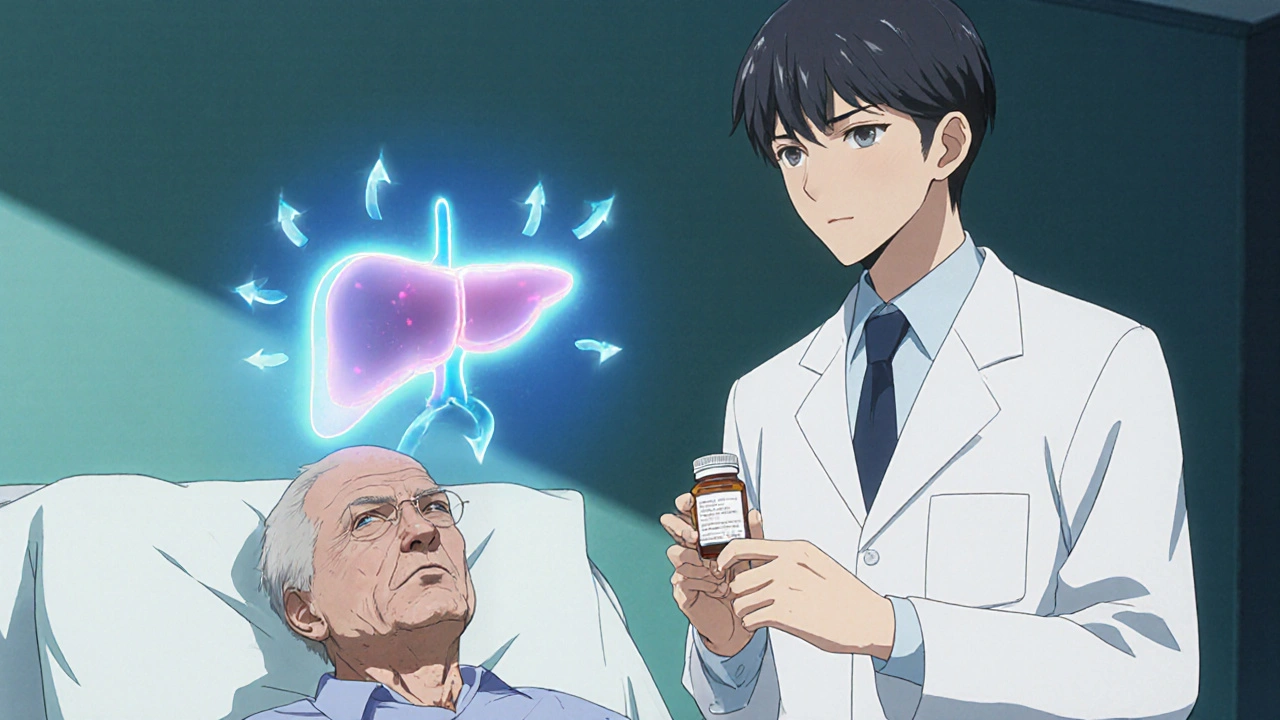
When dealing with hepatic impairment opioids, opioid use in patients with reduced liver function requires special attention to metabolism, dosing, and safety. Also known as opioid dosing in liver disease, it directly ties into how the liver processes drugs. Opioid metabolism refers to the breakdown of opioid compounds mainly by CYP enzymes in the liver and influences how long a medication stays active. Liver disease covers conditions like cirrhosis, hepatitis, and fatty liver that diminish enzymatic activity and blood flow creates the backdrop for every dosing decision. Understanding these connections lets clinicians balance pain relief with the risk of accumulation and side effects.
Key Considerations for Safe Opioid Use
The first step is to assess the severity of liver impairment. Child‑Pugh class A patients often tolerate standard doses, while class B or C may need a 25‑50% reduction. This dose adjustment for hepatic impairment is guided by how much the liver can metabolize, which varies by opioid. For example, morphine and codeine rely heavily on glucuronidation, so they may build up in severe disease, whereas fentanyl, which is metabolized by CYP3A4, can be safer if the enzyme activity is only mildly reduced. Pain management in liver disease focuses on choosing opioids with predictable clearance and minimal active metabolites to avoid hepatic encephalopathy or respiratory depression.
Another factor is concurrent renal function. Many opioids generate metabolites cleared by the kidneys, so if a patient also has renal impairment, the risk of toxicity rises. Monitoring serum drug levels, when available, helps catch accumulation early. Education is equally important: patients should know to report increased drowsiness, confusion, or constipation promptly. Adjusting the dosing interval instead of the dose can sometimes provide steadier pain control while keeping peak concentrations lower.
Finally, always review other medications that affect liver enzymes. CYP3A4 inhibitors like ketoconazole or certain antibiotics can raise opioid levels, while inducers such as rifampin can lower them, leading to inadequate pain relief. A quick drug‑interaction check becomes part of the routine when prescribing for anyone with hepatic impairment.
Below you’ll find a curated collection of articles that dive deeper into these topics—ranging from specific drug interaction guides to practical dosing tables. Whether you’re a prescriber looking for quick reference or a patient seeking understandable advice, the posts ahead cover the full spectrum of hepatic impairment opioid care.
Opioids & Liver Disease: Metabolism, Accumulation, and Side Effects
Learn how liver disease changes opioid metabolism, causes drug accumulation, and heightens side effects. Get dosing tips, safety checklists, and a quick reference table.
Detail