Drug interactions: simple rules to stay safe
A single grapefruit or an over-the-counter painkiller can change how your prescription works. Drug interactions happen when one medicine, food, or supplement alters another’s effect — making it weaker, stronger, or more dangerous. You don’t need a pharmacy degree to avoid most of them. Start with a clear list of what you take and follow a few practical steps.
Quick red flags to know
Watch for certain high-risk combos. Blood thinners plus anti-inflammatories can cause bleeding (warfarin + NSAIDs). Clopidogrel (Plavix) can be affected by some stomach acid drugs like omeprazole — that may reduce Plavix’s benefit. Some statins (eg, simvastatin) jump to risky levels with certain antibiotics or antifungals, raising muscle breakdown risk. Grapefruit juice can boost levels of many drugs including some statins and immune drugs. Herbal supplements matter too: St. John’s wort lowers levels of many meds, including some birth control and antidepressants.
Antidepressant mixes deserve extra caution. Combining MAO inhibitors with SSRIs or certain migraine meds risks serotonin syndrome — a serious reaction with high fever, tremor, or confusion. Nefazodone is an older antidepressant that affects liver enzymes and can raise levels of other drugs; check before starting or stopping it.
How to check and what to do
Keep a current medicine list (prescription, OTC, vitamins, herbs) on your phone. Before adding anything new, run it through a reputable checker like Drugs.com interaction tool or your local health service checker, and show the list to your pharmacist or prescriber. Pharmacists are often the fastest safety net — ask them about new prescriptions, especially if you’re on blood thinners, seizure meds, immunosuppressants, or multiple antidepressants.
If you notice worrying signs after a new combo — heavy bruising or bleeding, shortness of breath, very high temperature, severe muscle pain, fainting, seizures, or sudden confusion — seek urgent care. For milder issues like increased sleepiness, nausea, or dizziness, call your prescriber or pharmacist before stopping medicines; abrupt stops can be risky.
Practical habits cut risk: take prescriptions exactly as directed, avoid mixing alcohol with sedatives, don’t assume “natural” means safe, and ask for alternatives when a risky interaction appears. When switching drugs (for example changing statins) ask about equivalent dosing and interaction differences — that avoids surprises with insurance and side effects.
This tag collects pieces that dig into specific interactions (Plavix, statins, antidepressants, steroids and more). Browse articles here for real-world examples and easy steps you can use right now to keep your meds working the way they should.

Garlic Supplements and Anticoagulants: What You Need to Know About Bleeding Risk
Garlic supplements can dangerously increase bleeding risk when taken with blood thinners like warfarin or aspirin. Learn why even natural supplements need caution, what doses are risky, and how to stay safe before surgery.
Detail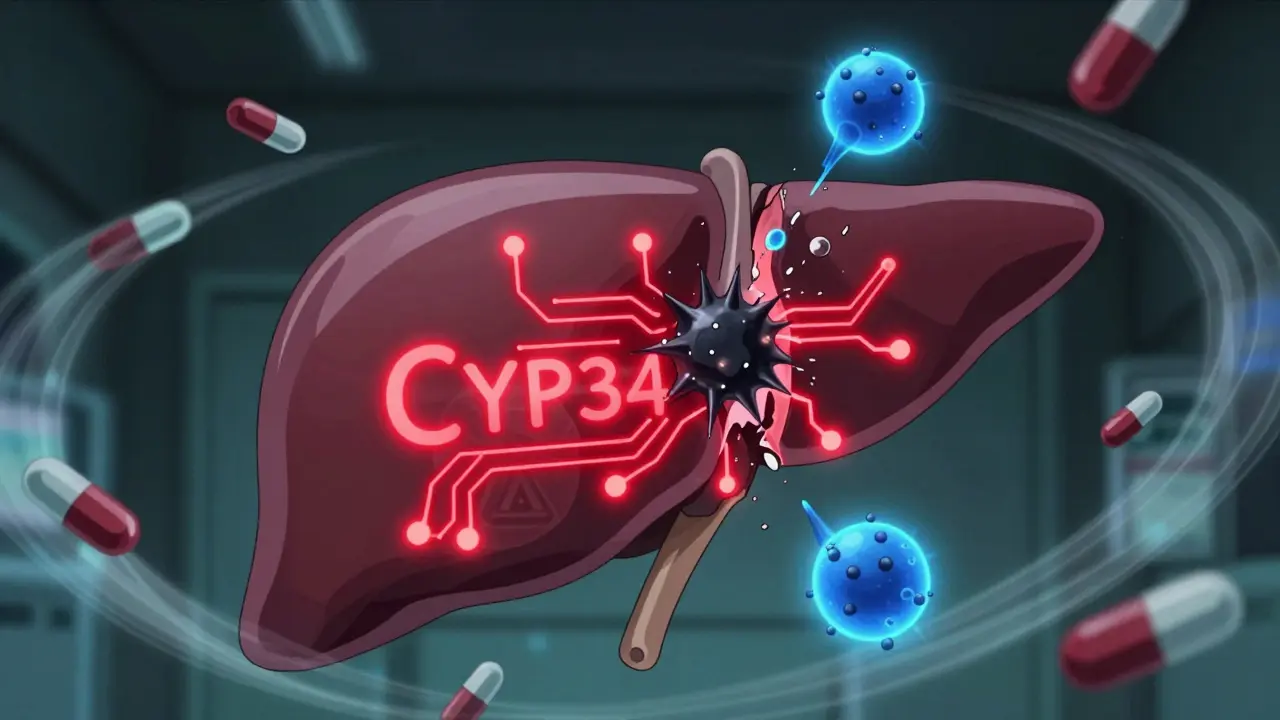
Lopinavir/Ritonavir Boosting: How CYP3A4 Interactions Impact Drug Safety and Efficacy
Lopinavir/ritonavir boosts HIV treatment by blocking CYP3A4, but this causes dangerous interactions with many common drugs. Learn which meds are risky, why it's still used, and how to stay safe.
Detail
Amiodarone, Digoxin, and Warfarin: The Dangerous Drug Triad You Can't Afford to Miss
Amiodarone, digoxin, and warfarin together can cause deadly drug interactions. Learn how this triad raises the risk of digoxin toxicity and life-threatening bleeding - and what you must do to stay safe.
DetailFexofenadine and Drug Interactions: What to Watch Out For
As a blogger, I recently did some research on Fexofenadine and discovered that it's essential to be aware of potential drug interactions. Fexofenadine is an antihistamine used to treat allergies, but it can interact with certain medications, leading to unwanted side effects. It's important to watch out for interactions with drugs like ketoconazole, erythromycin, and antacids containing aluminum or magnesium. Always consult your healthcare provider before starting any new medication, especially while taking Fexofenadine. Stay informed and proactive to ensure the safest and most effective use of this medication.
Detail